Uworld 5
Kaiser
 .,
.,
Bacillary

*Bartonella* species are gram-negative, intracellular bacteria that typically establish infection through cutaneous penetration after a cat scratch (*Bartonella henselae*) or body/head lice bite (*Bartonella quintana*). The organism causes a local dermal infection, spreads to the vascular endothelium, and then attacks red blood cells. The major manifestations of infection are therefore mostly cutaneous, lymphatic, and endovascular (Cat-scratch disease, bacillary angiomatosis, endocarditis).
Bacillary angiomatosis (BA) is a Bartonella infection seen primarily in patients with HIV with CD4 counts <100/mm3 (CD4-mediated immune response is crucial for control and elimination of the organism). Symptoms feature vascular cutaneous lesions that often begin as small reddish/purple papules and evolve into friable pedunculated or nodular lesions. Constitutional symptoms (eg, fever, malaise, night sweats) are typically present and organ (liver, central nervous system, bone) involvement may occur. Diagnosis is made by tissue biopsy with histopathology and microscopic identification of organisms. Treatment requires antibiotics (eg, doxycycline, erythromycin) and the initiation of antiretroviral therapy (usually 2-4 weeks later).

Tricuspid Valve Atresia

In the normal fetus, blood is shunted away from the lungs by the patent ductus arteriosus, and the systemic circulation relies primarily on the right heart. As a result, newborns are born with a larger right ventricle compared to the left ventricle, which appears as physiologic right axis deviation and R waves in the precordial leads (V1-V3) on electrocardiogram (ECG).
Tricuspid valve atresia (TVA) should be suspected in a cyanotic infant with left axis deviation and small or absent R waves in the precordial leads. The lack of communication between the right heart chambers results in a hypoplastic right ventricle and diminished right ventricular forces on ECG. The lack of blood flow to the right ventricle and pulmonary outflow tract consequently results in underdevelopment of the pulmonary valve and/or artery. Pulmonary undercirculation is the reason for decreased pulmonary markings on chest x-ray. Associated atrial and ventricular septal defects are necessary for survival, allowing for mixing of oxygenated and deoxygenated blood to provide some oxygenated blood for the systemic circulation. The atrial septal defect permits increased blood flow to the right atrium and subsequent enlargement, resulting in tall, peaked P waves on ECG. The ventricular septal defect manifests as a holosystolic murmur that is loudest at the left lower sternal border.
The cause of TVA is unknown, but it can occur in any patient with congenital heart disease risk factors (eg, congenital rubella syndrome, Down syndrome, maternal diabetes, family history of congenital heart disease). In the absence of surgical intervention, most children will die in the first year of life. Surgical repair improves 10-year survival rates to 80%.
The following congenital heart defects also cause cyanosis but with different ECG and chest x-ray findings.
Ebstein's anomaly is associated with maternal lithium use during pregnancy. The primary problem is displacement of a malformed tricuspid valve into the right ventricle. The droopy tricuspid valve results in severe tricuspid regurgitation and right atrial enlargement, resulting in tall P waves and right axis deviation on ECG. Extreme cardiomegaly from heart failure can be seen on chest x-ray.
MVO2
Septic: Elevated mixed venous oxygen (MvO2) saturation due to hyperdynamic circulation (as cardiac output is increased in response to reduced SVR to maintain peripheral tissue perfusion) with an inability of tissues to adequately extract oxygen (may develop lactic acidosis from tissue hypoperfusion)
AS
Supravalvular aortic stenosis (AS), the second most common type of AS, usually refers to congenital left ventricular outflow tract obstruction due to discrete or diffuse narrowing of the ascending aorta. This causes a systolic murmur similar to that seen with valvular AS; however, the murmur is usually best heard at the first right intercostal space, higher than where the valvular AS murmur is best heard. Patients may also have unequal carotid pulses, differential blood pressure in the upper extremities (high-pressure jet in ascending aorta), and a palpable thrill in the suprasternal notch.
Patients with significant supravalvular AS develop left ventricular hypertrophy over time and can also have coronary artery stenosis as an associated anomaly. These changes, along with the increase in myocardial oxygen demand during exercise, can lead to subendocardial or myocardial ischemia, which is likely responsible for this patient's anginal symptoms during exercise.
Noninvasiv PPV

Initial management of AECOPD (acute exacerbation) includes inhaled short-acting bronchodilators, glucocorticoids, and antibiotics. Patients with continued symptoms despite medical management should be considered for noninvasive ventilatory support.
Noninvasive positive-pressure ventilation (NPPV) is ventilatory support delivered by facemask rather than endotracheal tube; it can be delivered in several different modes, including continuous positive airway pressure and bilevel positive airway pressure. NPPV decreases work of breathing, improves alveolar ventilation, and is the preferred method of respiratory support in patients with AECOPD. Physiologic benefits include a decrease in respiratory rate and arterial carbon dioxide tension (PaCO2), with an increase in tidal volume, minute ventilation, and arterial oxygen tension (PaO2). NPPV in patients with AECOPD is associated with a decrease in mortality, intubation rate, treatment failure, length of hospital stay, and incidence of nosocomial infection.
Toxic Alcohol
Toxic alcohols
Toxicity
Clinical features
Laboratory results
Alcohol ketoacidosis
Slurred speechUnsteady gaitAltered mentation
High osmolar gapIncreased anion gap metabolic acidosis (ketosis)
Methanol ingestion
Visual blurring, central scotomataAfferent pupillary defectAltered mentation
High osmolar gapIncreased anion gap metabolic acidosis
Ethylene glycol ingestion
Flank painHematuria, oliguriaCranial nerve palsies, tetany
High osmolar gapIncreased anion gap metabolic acidosisCalcium oxalate crystals in urine
Isopropyl alcohol ingestion
CNS depressionDisconjugate gazeAbsent ciliary reflex
High osmolar gapNo increased anion gap or metabolic acidosis
CNS = central nervous system.
This patient's acute toxicity following ingestion of automotive antifreeze raises concern for possible ethylene glycol poisoning. Ethylene glycol is often ingested intentionally as an ethanol substitute or as a mode of attempted suicide. Following ingestion, ethylene glycol causes inebriation and sedation, similar to ethyl alcohol. Metabolism via alcohol and aldehyde dehydrogenases produces glycolic acid, which is subsequently converted to oxalic acid. Oxalic acid can bind to calcium, leading to hypocalcemia and precipitation of calcium oxalate crystals in the urine.
Renal toxicity from ethylene glycol is characterized by acute kidney injury (due to direct nephrotoxicity of glycolate and obstruction of tubules by calcium oxalate crystals) with flank pain and hematuria (as noted in this patient) as well as oliguria. Patients typically have severe metabolic acidosis with an increased anion gap, very low bicarbonate level, and compensatory drop in pCO2. The osmolal gap (measured plasma osmolality – calculated plasma osmolality, which is often estimated by [(2 x plasma Na) + (glucose/18) + (blood urea nitrogen/2.8)]) is typically elevated as well.
Sickle Cell Infections
Infections in sickle cell disease
Infection
Etiology
Pneumonia
Streptococcus pneumoniae
Osteomyelitis/septic arthritis
Staphylococcus aureus**Salmonella species
Bacteremia/sepsis
Streptococcus pneumoniae**Haemophilus influenzae type B
Meningitis
Streptococcus pneumoniae
IE Prophylaxis
Current guidelines for prevention of IE recommend antibiotic prophylaxis for specific invasive procedures in patients with cardiac conditions that are associated with the highest risk of adverse outcomes from IE. These conditions include:
Prosthetic heart valve
Previous history of IE
Structurally abnormal valve in a transplanted heart
Certain congenital heart disease (CHD) (eg, unrepaired cyanotic CHD, repaired CHD with prosthetic material within 6 months of repair, repaired CHD with residual defects)
For patients with these high-risk conditions, antibiotic prophylaxis is indicated prior to certain invasive procedures (eg, surgery on infected skin or muscle). Prophylaxis is not routinely indicated prior to gastrointestinal or genitourinary procedures, unless patients have active infection (particularly with Enterococcus).
Acute Scrotal Pain

Pharyngitis in Children

Centor criteria unreliable in children
DKA management
Management of DKA & HHS
IV fluids
High-flow 0.9% normal saline is initially recommendedAdd dextrose 5% when serum glucose is ≤200 mg/dL
Insulin
Initial continuous IV insulin infusionSwitch to SQ (basal bolus) insulin for the following: Able to eat, glucose <200 mg/dL, anion gap <12 mEq/L, serum HCO3 ≥15 mEq/LOverlap SQ & IV insulin by 1-2 hours
Potassium
Add IV potassium if serum K+ ≤5.2 mEq/LHold insulin for serum K+ <3.3 mEq/LNearly all patients K+ depleted, even with hyperkalemia
Bicarbonate
Consider for patients with pH <6.9
Phosphate
Consider for serum phosphate <1.0 mg/dL, cardiac dysfunction, or respiratory depressionMonitor serum calcium frequently
DKA = diabetic ketoacidosis; HHS = hyperglycemic hyperosmolar nonketotic state; IV = intravenous;SQ = subcutaneous.
VQ

In pregnant patients with a normal chest x-ray (and no manifestations of deep venous thrombosis), a ventilation/perfusion (V/Q) scan is the test of choice (as CT angiograms may have lower diagnostic accuracy in pregnant women). V/Q scan results are stratified into normal, low, moderate, and high probability, but they need to be combined with PE pretest probability to arrive at a diagnosis of PE:
A normal V/Q scan can reliably rule out PE, regardless of pretest probability.
In patients with high pretest probability of PE, a high-probability V/Q scan result would confirm the diagnosis; in patients with low pretest probability of PE, a low-probability V/Q scan result would exclude the diagnosis.
Any other combination warrants additional testing (eg, CT angiogram), as with this patient.
In this patient with high pretest probability for PE, a V/Q scan was an appropriate initial test because a high-probability V/Q scan result would have confirmed the diagnosis of PE. However, given her low-probability V/Q scan result, further testing is now required. At this time, the risk-benefit ratio of CT angiogram is acceptable given the relatively high mortality associated with untreated PE in pregnancy and the relatively low risk of radiation exposure from CT angiogram.
Blood Pressure Control
Joint National Committee 8 recommendations for treating hypertension
Initiate Rx
Goal blood pressure
Age >60
>150 mm Hg systolic BP or >90 mm Hg diastolic BP
<150/90 mm Hg
Age <60,**chronic kidney disease,**diabetes
>140 mm Hg systolic BP or >90 mm Hg diastolic BP
<140/90 mm Hg
Initial treatment choice
Black
Thiazide diuretic or CCB, alone or in combination (ACEI/ARB, not first-line)
Other ethnicities
Thiazide diuretic, ACEI, ARB, or CCB, alone or in combination
All ethnicities with chronic kidney disease
ACEI or ARB, alone or in combination with other drug classes
FFN

Fetal fibronectin (FFN) testing is used to determine whether a patient at <34 weeks gestation with regular uterine contractions and no cervical change is in preterm labor. FFN is a protein found at the interface of the chorion and decidua; contractions disrupt this interface and release FFN into vaginal secretions. A positive FFN test is a strong predictor of delivery within the next week and an indication for administration of antenatal corticosteroids (eg, betamethasone). Patients with a negative FFN test have a low likelihood of delivery within the next 2 weeks and can resume routine prenatal care and expectant management (Choice D).
Livedo
Livedo reticularis (LR) is a transient red or purplish, blotchy or latticelike rash that primarily affects the lower extremities. It is caused by obstruction, vasospasm, or sluggish flow in the superficial venules. LR is often a benign finding and can frequently be seen in otherwise healthy women during cold weather. However, LR can also be a sign of vasculitic (eg, polyarteritis nodosa, systemic lupus erythematosus) or vasoocclusive (eg, cholesterol embolization, antiphospholipid syndrome, cryoglobulinemia) disorders.
This patient has LR with acute leg swelling (likely due to deep venous thrombosis) and a history of recurrent miscarriages. In this context, LR is likely due to antiphospholipid (APL) syndrome. LR is the most common dermal sign of APL syndrome and is associated with an increased risk of arterial occlusive complications (eg, stroke, retinal artery occlusion). However, although APL is associated with thrombosis, the partial thromboplastin time – but not prothrombin time (Choice D)– will be prolonged, likely due to binding of phospholipid reagents in the assay by the antiphospholipid antibodies (lupus anticoagulant). Mixing of patient plasma containing lupus anticoagulant with normal plasma will not correct the partial thromboplastin time in contrast to patients with clotting factor deficiencies in which the addition of normal plasma will supply the necessary factors to normalize the assay.
Cardiotoxicity
Chemotherapy-induced cardiotoxicity
Type I
Associated with anthracyclinesMyocyte necrosis & destruction (fibrosis)Progression to overt clinical heart failureLess likely to be reversible
Type II
Associated with trastuzumabMyocardial stunning/hibernation without myocyte destructionAsymptomatic left ventricular systolic dysfunctionMore likely to be reversible
Liver Mass
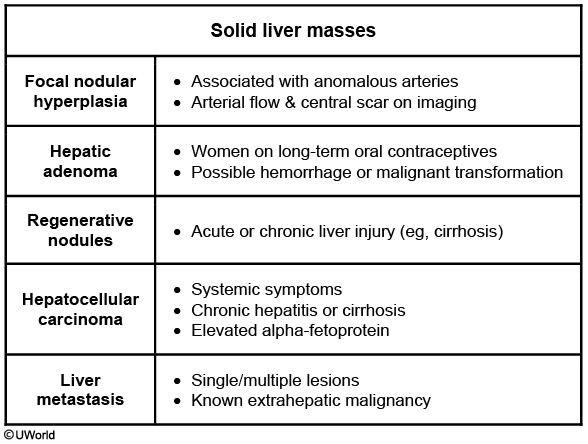
This patient likely has focal nodular hyperplasia (FNH), the most common benignnonvascular liver lesion. It is normally asymptomatic, and most cases are discovered incidentally during evaluations for other causes of intraabdominal pathology (eg, gallstone disease, dyspepsia). Occasionally, patients may have abdominal symptoms due to the mass effect of the growing lesion.
FNH is most commonly a small (<5 cm), solitary lesion and is due to a hyperplastic response to hyperperfusion that is caused by an inappropriately large artery typically found at the center of the lesion. The appearance of FNH on ultrasound is variable, although color Doppler may help distinguish the abnormal arterial flow. CT scan or MRI can be highly suggestive, demonstrating a hypo- or isodense lesion with arterial enhancement and a central stellate scar.
FNH is more common in women than men. It may be estrogen sensitive, and patients on oral contraceptives tend to have larger and more vascular lesions. FNH is generally stable and does not normally result in complications. Management is conservative; some providers advise women to discontinue use of oral contraceptives and offer serial examinations for patients with larger masses (>8 cm).
Biopsy hepatic adenoma.
Femoral artery

Complications at the site of vascular access are common in patients undergoing cardiac catheterization; the right common femoral artery is the most commonly used vascular access point. This patient has most likely developed a pseudoaneurysm of the right femoral artery. A pseudoaneurysm occurs when a defect in the arterial wall (eg, inadequately sealed arterial puncture site) causes bleeding that remains confined within the surrounding layer of periarterial connective tissue. The result is a contained hematoma that has ongoing communication with the arterial lumen. Diastolic pressure equalizes between the artery and the confined hematoma; therefore, as blood is forced through the arterial wall defect during systole, a systolic bruit is heard at the site of the pseudoaneurysm. A tender, pulsatile mass is also typically present.
Inadequate post-procedural arterial compression is the strongest risk factor for pseudoaneurysm development. The diagnosis should be confirmed by ultrasound.
An arteriovenous fistula can occur when inadequate hemostasis of an arterial puncture site allows blood to communicate with an inadvertently punctured adjacent vein. Patients may have localized swelling and tenderness, but no mass is present. A bruit is typically present, but it is continuous (arterial pressure exceeds venous pressure throughout the cardiac cycle) rather than systolic and is typically accompanied by a palpable thrill.
Nails

This patient with an enlarging pigmented nail lesion has a nail melanoma. Unlike dermal melanomas, which typically appear as asymmetric shapes with irregular borders, nail melanomas form longitudinal bands in the nail plate (longitudinal melanonychia) due to the presence of pigment in the nail as it grows outward. Unpigmented melanomas can also occur and present as nodules or irregularities in the nail plate.
Longitudinal melanonychia that involves multiple nails, is stable over years, or is <3 mm wide is usually benign and may be observed with regular follow-up. However, lesions that are larger, have indistinct borders, change appearance over time, or extend into the nail folds suggest possible melanoma.
(Choice A) Psoriasis is a T cell-mediated immune disorder characterized by keratinocyte hyperproliferation. It presents with erythematous plaques with a silvery scale over extensor surfaces (eg, knees, elbows) and the scalp. Associated nail findings include pitting, distal onycholysis, and hyperkeratosis.

(Choice B) Impaired cellular proliferation in the nail matrix (eg, trauma, local or systemic illness, medications) leads to formation of horizontal ridges that move outward as the nail grows (Beau lines).

(Choice D) Microemboli from infectious endocarditis can disrupt capillaries in the nail bed, leading to splinter hemorrhages, which appear as small linear or flame-shaped streaks under the nail.
(Choice E) Digital clubbing is a thickening of the distal phalanges with a "drumstick" appearance, flattening of the nail folds, and shininess of the nail and distal finger. It is typically associated with pulmonary malignancy and chronic hypoxic pulmonary disease (eg, cystic fibrosis, bronchiectasis).
(Choice F) Trauma to the nail bed can cause subungual hematoma. The appearance may resemble melanoma, but most patients recall a specific inciting injury. Given its prolonged duration, this patient's lesion is unlikely to be a simple hematoma.

DRESS
DRESS syndrome is a rare, potentially life-threatening drug reaction characterized by the following:
Drug - most commonly allopurinol and antiepileptics (eg, phenytoin, carbamazepine)
Reaction (rash) - morbilliform eruption that starts on the face or upper trunk and becomes diffuse (often >50% body surface area) and confluent; facial edema is common
Eosinophilia
Systemic symptoms - fever, malaise, and diffuse lymphadenopathy; approximately 90% of patients have involvement of >1 organ system (eg, liver [transaminitis], kidney, lung)
DRESS syndrome, unlike other drug reactions, has an unusually long latency (2-8 weeks) between drug initiation and the manifestation of symptoms. The pathogenic mechanism remains unclear, but the majority of patients with this syndrome also have antibody evidence of human herpesvirus 6 reactivation. Some studies suggest cross-reactivity between herpesvirus lymphocytes and drug antigens.
Diagnosis is largely clinical; treatment involves the immediate cessation of the inciting drug and supportive care (eg, fluid, electrolyte, nutrition support). Most patients recover completely within weeks or months, but relapses may occur.

Last updated