Uworld 2
Macrocytic Anemia
Myelodysplastic syndromes
Acute myeloid leukemias
Drug-induced (eg, hydroxyurea, zidovudine, chemotherapy agents)
Liver disease
Alcohol abuse
Hypothyroidism
Pancreatic cancer

Classic manifestations include weight loss and insidious onset of gnawing abdominal pain (usually epigastric and radiating to the back), which is worse at night, with eating, or when lying supine.
Cancers in the head of the pancreas (60%-70%) typically present with jaundice (common bile duct obstruction, elevated alkaline phosphatase and bilirubin) and steatorrhea (pancreatic exocrine insufficiency or pancreatic duct blockage). In patients with these findings, abdominal ultrasound is preferred for detecting pancreatic head tumors and excluding other potential causes of biliary obstruction (eg, choledocholithiasis).
Cancers in the body and tail usually do not present with obstructive jaundice. Abdominal CT scan is preferred (more sensitive and specific) and helps exclude other conditions. Ultrasound is less sensitive for visualizing the pancreatic body and tail (due to overlying bowel gas) and for detecting smaller (<3 cm) tumors.
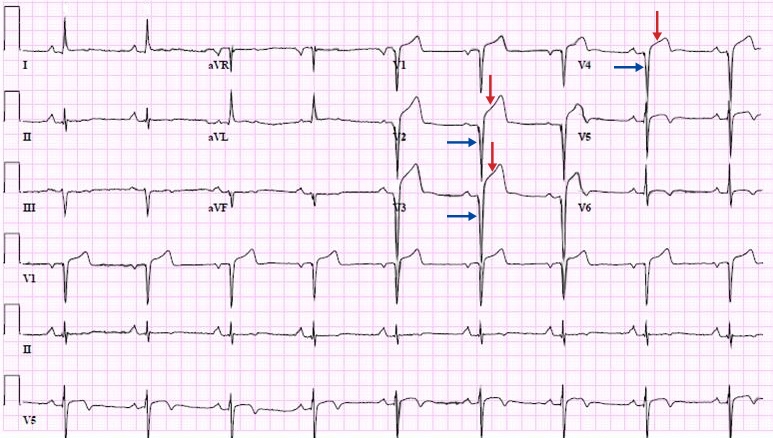
Ventricular aneurysm
persistent deep Q and ST elevation
DKA
DKA
IV fluids
High-flow 0.9% normal saline is initially recommended Add dextrose 5% when serum glucose is <200 mg/dL
Insulin
Initial continuous IV insulin infusion Switch to SQ (basal bolus) insulin for the following: Able to eat, glucose less than 200 mg/dL, anion gap less than12 mEq/L, serum HCO3 >15 mEq/L Overlap SQ & IV insulin by 1-2 hours
Potassium
Add IV potassium if serum K+ less than 5.2 mEq/L Hold insulin for serum K+ less than 3.3 mEq/L Nearly all patients K+ depleted, even with hyperkalemia
Bicarbonate
Consider for patients with pH <6.9
Phosphate
Consider for serum phosphate less than 1.0 mg/dL, cardiac dysfunction, or respiratory depression Monitor serum calcium frequently
Lower back pain
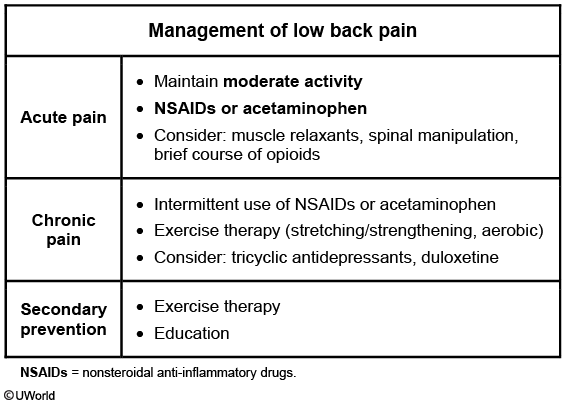
This patient has uncomplicated chronic (>12 weeks) low back pain (LBP). Patients with acute (<4 weeks) LBP should be advised to maintain moderate activity with short courses of acetaminophen or nonsteroidal anti-inflammatory drugs(NSAIDs) to provide pain relief. Most patients will have resolution without any additional intervention. However, those with subacute (4-12 weeks) or chronic LBP are more likely to continue to have recurrent or persistent pain.
In patients with chronic LBP, exercise has proven to be beneficial in reducing pain and improving function. Patients often start with a supervised exercise program that emphasizes stretching and strengthening of the back muscles. Aerobic exercise is also helpful. Subsequently, patients can transition to a home exercise program, which should be continued on a long-term basis. Short courses of acetaminophen or NSAIDs can be used intermittently. Some patients also may benefit from tricyclic antidepressants or duloxetine, but opioids, benzodiazepines, and muscle relaxants are not advised for routine use.
Fluoroquinolone
This patient's presentation suggests Achilles tendinopathy likely due to recent fluoroquinolone use. Continued use of this medication can lead to rupture of the tendon. Risk factors include age >60, female, normal body mass index, concurrent oral corticosteroid use, and history of organ transplant. Tendinopathy most commonly involves the Achilles tendon but can also occur in the rotator cuff, hand, biceps, thumb, and other tendon sites.
Pain/tenderness is present 2-6 cm above the posterior calcaneus in Achilles tendinopathy. Drug manufacturers are required to include a boxed warning notifying patients of the increased risk of tendinopathy and tendon rupture associated with fluoroquinolones. Patients should stop the drug at the onset of symptoms, avoid exercise and/or use of the affected area, and seek medical care for symptom evaluation and changing to a non-fluoroquinolone antibiotic.
Pes Anserine Bursitis
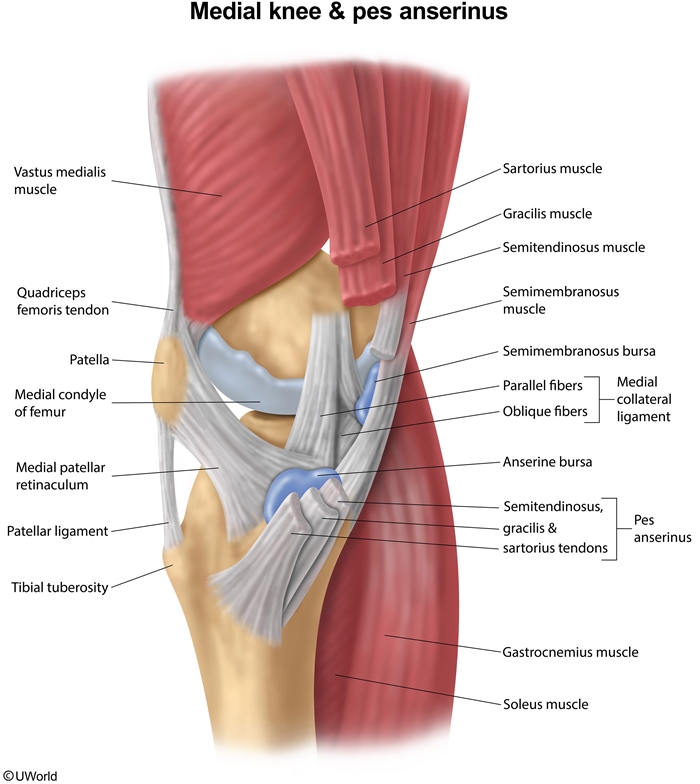
This patient with medial knee pain and focal tenderness has pes anserinus pain syndrome (PAPS). This condition is often referred to as anserine bursitis, but most patients do not have true inflammation in the bursa, and multiple regional structures can contribute to the pain. The pes anserinus is formed by the conjoined tendons of gracilis, sartorius, and semitendinosus. The anserine bursa is located anteromedially over the tibial plateau, just below the joint line of the knee and deep to the pes anserinus.
PAPS can be caused by an abnormal gait, overuse, or trauma. Localized pain is typical over the anteromedial tibia and is often exacerbated by pressure from the opposite knee while lying on the side. Examination shows a well-defined area of tenderness over the medial tibial plateau just below the joint line. A valgus stress test does not aggravate the pain, indicating no medial collateral ligament involvement (Choice A). The diagnosis is primarily based on clinical features, although x-ray can exclude concurrent osteoarthritis of the knee.
Behcet
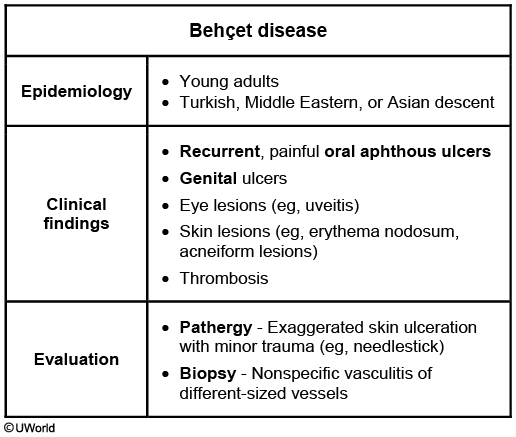
This patient has characteristic features of Behçet syndrome, including recurrent painful oral and genital aphthous ulcers, uveitis, and erythema nodosum (tender red nodules usually in the pretibial area). These patients are also at high risk of vascular disease (vasculitis) with venous and arterial thrombosis. Patients may also demonstrate pathergy, an exaggerated ulcerating skin response following minor injuries (eg, needlestick).
Behçet syndrome is more common in patients of Turkish, Middle Eastern, and Asian descent. The diagnosis is made based on clinical features, and laboratory evaluation is primarily directed to ruling out other disorders. Biopsy of affected tissues is not usually needed but may show a nonspecific vasculitis, often involving small or medium-sized vessels.
Pathergy:

Felty Syndrome

This patient has inflammatory arthritis, splenomegaly, and neutropenia. This triad of clinical findings is characteristic of Felty syndrome (FS). FS is most common in patients with long-established rheumatoid arthritis (RA) but occasionally precedes the diagnosis. Patients with FS typically have severe, seropositive RA with increased risk for extra-articular manifestations (eg, vasculitis, skin ulcers). The neutropenia of FS may be detected incidentally but increases the risk for recurring bacterial infections.
FS is more common in women, with a peak incidence in the fourth and fifth decades. The pathophysiology is unknown, but FS is associated with HLA-DR4 and has an increased incidence in patients with a family history of RA, suggesting a genetic component. The diagnosis is based primarily on clinical features, but hematologic studies (eg, peripheral blood smear, bone marrow biopsy) are frequently performed to exclude other causes of neutropenia. FS usually improves with treatment of the underlying RA (eg, methotrexate).
Cervical spondylosis
This patient is most likely suffering from cervical spondylosis. It is estimated that cervical spondylosis affects 10% of people older than 50 years of age. The history of chronic neck pain is typical. Limited neck rotation and lateral bending is due to osteoarthritis and secondary muscle spasm. Sensory deficit is due to osteophyte-induced radiculopathy and isolated sensory abnormalities are associated with good prognosis. Typical radiographic findings include bony spurs and sclerotic facet joints. Interestingly, such 'osteoarthritic' changes are common in asymptomatic patients older than 50 years of age; therefore, specificity of these findings are low. Other findings during cervical spondylosis may include narrowing of the disk spaces and hypertrophic vertebral bodies
Epidermal cyst
This patient has an epidermal inclusion cyst (EIC), also known as an epidermal cyst, a discrete benign nodule lined with squamous epithelium that contains a semisolid core of keratin and lipid. An EIC occurs when the epidermis becomes lodged in the dermis due to trauma or comedones, or it can arise de novo. EICs can be seen anywhere on the body, but are most common on the face, neck, scalp, or trunk. The lesion can gradually increase in size and may intermittently produce a cheesy white discharge. Some patients may develop significant inflammation with rupture and involvement of surrounding tissue. An EIC will usually resolve spontaneously but can recur.
Diagnosis is made clinically with examination showing a dome-shaped, firm, and freely movable cyst or nodule with a central punctum (small, dilated, pore-like opening). Excision is typically performed only for cosmetic reasons. Incision and drainage are occasionally needed for infected and fluctuant cysts that are painful and erythematous.

Lipomas are benign, painless subcutaneous masses with normal overlying epidermis. In contrast to epidermal cysts, lipomas are usually soft to rubbery and irregular, and do not typically regress and recur.
Tinea Corporis
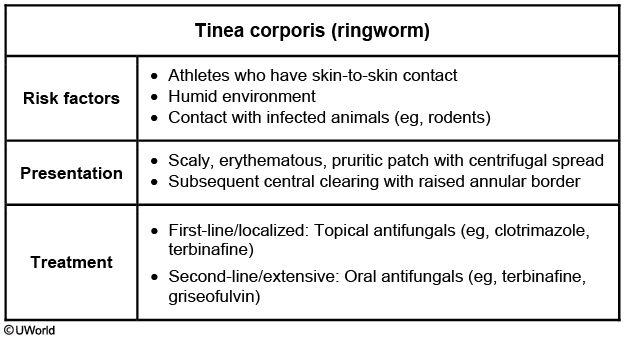
This patient has a pruritic rash with a scaly, erythematous border and central clearing consistent with tinea corporis (ringworm). Patches of tinea corporis are typically round or ovoid but may become confluent to form a "flower petal" shape. Skin contact, especially in warm and humid environments, is a common risk factor. Any species of dermatophyte may cause this condition, but Trichophyton rubrum is the most frequent culprit. Tinea corporis is often more extensive in patients with immunocompromising conditions (eg, HIV, diabetes mellitus).
The diagnosis is confirmed using potassium hydroxide (KOH) preparation of skin scrapings, which can show the characteristic segmented hyphae and arthrospores. Mild to moderate cases can be treated with topical antifungal preparations (eg, terbinafine, clotrimazole), but patients who fail topical therapy or have extensive disease may need systemic therapy. In adults, oral terbinafine, fluconazole, and itraconazole are preferred over griseofulvin due to greater efficacy and fewer side effects.

Pityriasis Rosea

Pityriasis rosea is characterized by numerous oval, scaly plaques that follow the cleavage lines of the trunk. It often presents with an initial lesion called a herald patch, which is much larger than the later lesions.
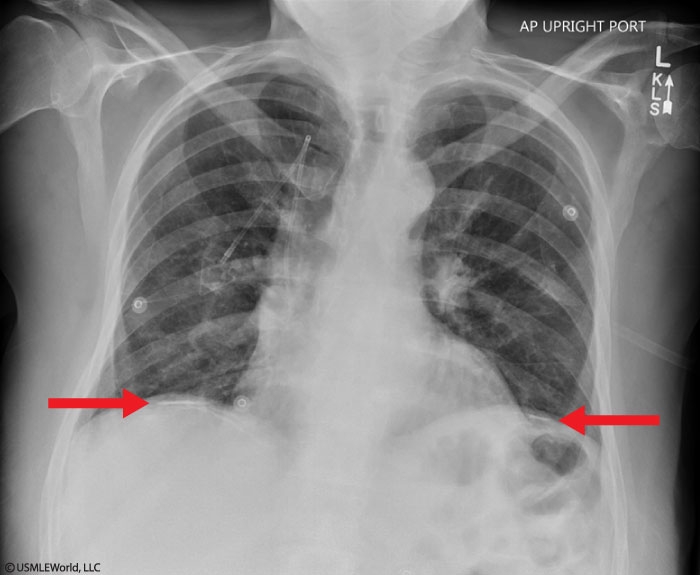
Asbestosis
Asbestosis and bronchogenic carcinoma can present similarly, with most patients developing progressive dyspnea. However, patients with asbestosis can be asymptomatic for up to 20-30 years after asbestos exposure. Cough, sputum production, and wheezing are not typically present (unless there is concurrent chronic obstructive pulmonary disease). Physical examination frequently shows bibasilar, end-inspiratory crackles and fingernail clubbing as the disease progresses. Chest x-ray can show bibasilar reticulonodular infiltrates, honeycombing (cystic areas surrounded by interstitial infiltrates), and bilateral pleural thickening. High-resolution chest computed tomography typically shows subpleural linear densities and parenchymal fibrosis. Almost 50% of patients have pleural plaques, which can help differentiate asbestosis from other causes of pulmonary fibrosis. Imaging studies may also show signs of bronchogenic carcinoma.
Arsenic Poisoning
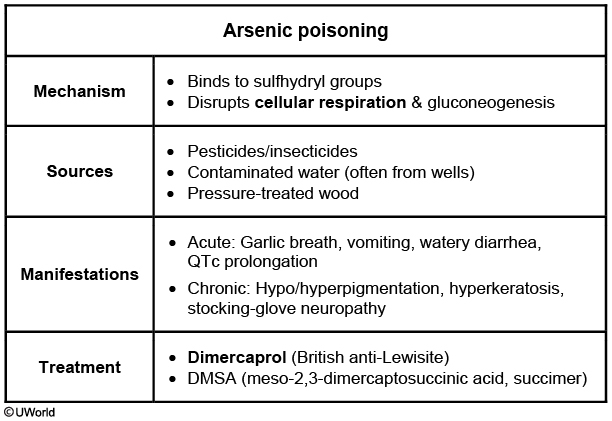
This patient, who is routinely exposed to antique wood, has polyneuropathy, pancytopenia, mild transaminase elevation, and a variety of skin lesions characteristic of chronic arsenic toxicity.
Arsenic is a metalloid element that exists in numerous forms, including both natural and manmade compounds. Although humans are often exposed to low levels through diet and water, toxic exposure is more likely through mining, pesticide manufacturing, metalworking, and working with antique pressure-treated wood preserved with arsenic. Arsenic binding to sulfhydryl groups and interfering with various enzymes is likely responsible for the clinical manifestations of acute and chronic arsenic toxicity.
Patients chronically exposed to arsenic develop a sensorimotor neuropathy in a stocking-glove distribution with burning, painful hypersensitivity, distal weakness, and hyporeflexia. Hypo- and hyperpigmentation of the skin occurs early in arsenic toxicity, and hyperkeratosis and scaling of the soles and palms is often seen later. Mees lines (horizontal striation of fingernails) are characteristic. Acute, severe arsenic toxicity can lead to profound pancytopenia and hepatitis, and chronic exposure leads to these manifestations to a smaller degree. Diagnosis is made through history, physical examination, and measurement of urine arsenic levels. Chelation (eg, dimercaprol, dimercaptosuccinic acid) is the treatment of choice for severe toxicity.
Chronic lead poisoning can lead to sensorimotor neuropathy in a stocking-glove distribution along with microcytic anemia. Although the neuropathy is similar to arsenic toxicity, gastrointestinal complaints are typical and skin changes are not usually seen.
Transfusions
Whole blood transfusion, which includes PRBCs in addition to plasma, may be used in patients with severe hemorrhage (eg, major trauma) requiring massive blood transfusions to assist in volume expansion.
Platelet transfusions are typically given for a platelet count <10,000/mm3 (increased risk of spontaneous hemorrhage) or for a platelet count <50,000/mm3 with active bleeding.
Fresh frozen plasma contains all clotting factors and plasma proteins from one unit of blood. It is usually indicated for severe coagulopathy (eg, liver disease, disseminated intravascular coagulation) with active bleeding. Fresh frozen plasma is generally not needed to correct a minimally abnormal INR (<1.6), which is a common finding in gastrointestinal bleeding.
Packed red blood cell (PRBC) transfusion can increase oxygen-carrying capacity in patients with significantly low hemoglobin levels. In general, stable patients without significant comorbid conditions should receive PRBC transfusion for hemoglobin <7 g/dL. Patients with active bleeding and hypovolemia may need PRBC transfusion at higher hemoglobin levels due to the initial hemoglobin concentration not fully reflecting blood loss.
Diabetes
Symmetric distal sensorimotor polyneuropathy is the most common neuropathy in patients with diabetes, and clinical features depend on the type of nerve fibers involved.
Small fiber injury is characterized by predominance of positive symptoms (eg, pain, paresthesias, allodynia).
Large fiber involvement is characterized by predominance of negative symptoms (eg, numbness, loss of proprioception and vibration sense, diminished ankle reflexes).
Lead toxicity
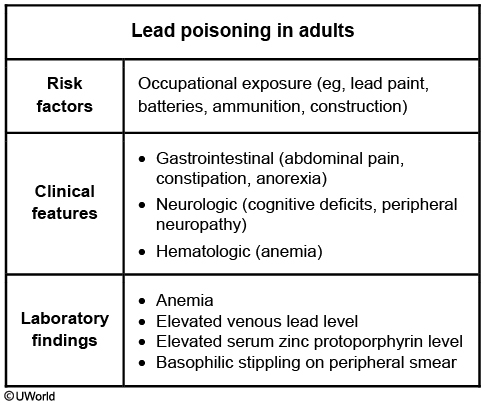
This patient's presentation suggests acute lead toxicity, which can include:
Gastrointestinal manifestations (eg, abdominal pain, constipation)
Neuropsychiatric manifestations (eg, forgetfulness), motor and sensoryneuropathies (eg, extensor weakness, stocking-glove distribution)
Hematologic manifestations (eg, microcytic anemia)
Nonspecific symptoms (eg, fatigue, irritability, insomnia) are common. Chronic lead exposure can also cause hypertension and nephropathy. Diagnosis hinges on eliciting a history of exposure through occupation (eg, battery manufacturing, plumbing, home restoration) or other means (eg, distillation of alcohol through parts with lead soldering).
Lead is primarily absorbed via the respiratory tract in adults but may otherwise be absorbed through the skin or gastrointestinal tract. It is 99% bound to erythrocytes and can disrupt heme synthesis to cause microcytic anemia. Diagnosis is made via blood lead levels, complete blood count with blood smear, and x-ray fluorescence to measure bone lead concentration. Peripheral blood smear can show basophilic stippling. Hyperuricemia (due to impaired purine metabolism) is also typical.
PCV
Two types of vaccines are currently available for use in the United States:
Pneumococcal polysaccharide vaccine (PPSV23) contains capsular material from 23 serotypes that have historically been responsible for the majority of pneumococcal infections. Because polysaccharides alone cannot be presented to T cells, the vaccine induces a relatively T-cell-independent B-cell response that is less effective in young children and the elderly.
Pneumococcal conjugate vaccine (PCV13) consists of capsular polysaccharides from 13 of the most common serotypes that have been covalently attached to inactivated diphtheria toxin protein. This polysaccharide-protein conjugate induces a T-cell-dependent B-cell response, resulting in improved immunogenicity due to the formation of higher-affinity antibodies and memory cells.
Routine administration of the PCV13 is recommended for all infants and young children. PPSV23 is administered to adults age <65 with predisposing comorbidities (eg, chronic heart or lung disease, diabetes mellitus, cirrhosis). Immunocompromised patients and all individuals age >65 should receive both vaccines to maximize protection.
Patellofemoral pain
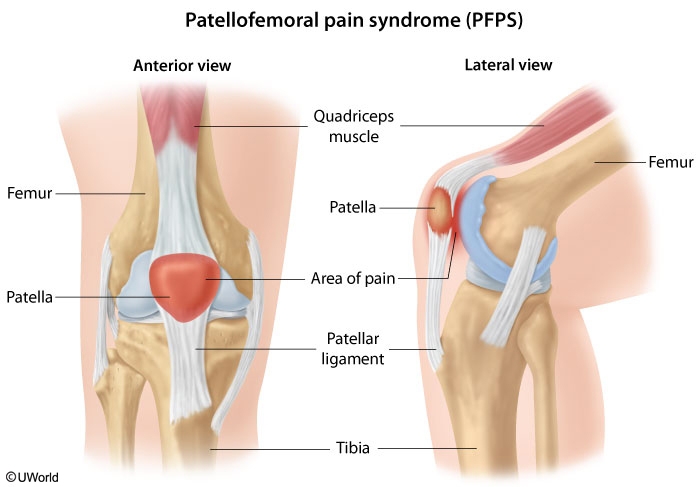
commonly seen in young female athletes with chronic overuse rather than acute trauma to the knee. Patients usually develop pain over the anterior knee that is reproduced by extending the knee while compressing the patella (patellofemoral compression test). Although the anterior knee may have swelling, true knee effusions and hemarthrosis are not seen.
Meniscal tear
Meniscal tears are possible in athletes subjected to rapid direction changes and are characterized by a subacute or chronic locking or popping sensation in the knee. However, immediate symptoms at the time of the injury may be mild. Effusions are possible but typically develop slowly, and hemarthrosis is rare.
ACL: blood
Leprosy
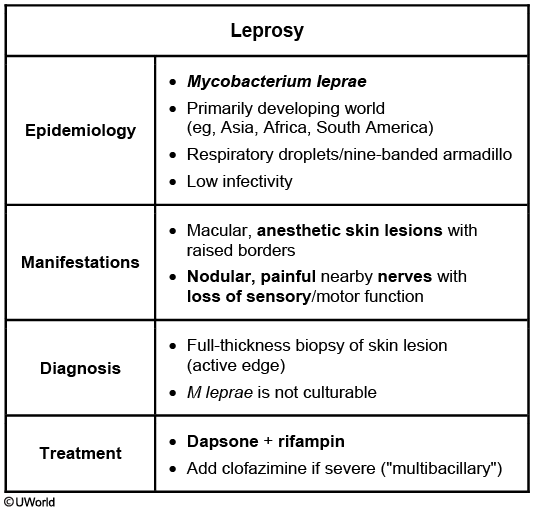
Leprosy is a chronic granulomatous disease of the skin and peripheral nerves caused by the acid-fast bacillus *Mycobacterium leprae*. Transmission is thought to occur via respiratory droplets, although cases are occasionally linked to close contact with a nine-banded armadillo. Infections are rare in the United States and occur primarily in immigrants or travelers to endemic regions (eg, Asia, Africa, South America).
Manifestations include >1 chronic, anesthetic, macular (often hypopigmented) skin lesions with raised, well-demarcated borders. Nearby nerves often become nodular and tender, and segmental demyelination may result in loss of sensation and motor function. Diagnosis is clinical in endemic regions, but in the United States patients usually require a full-thickness biopsy of the skin lesion edge (as M lepraeis not culturable). Patients with minimal lesions ("paucibacillary") are treated with dapsone and rifampin; those with extensive lesions ("multibacillary") require the addition of clofazimine. Lesions often take months or years to heal completely.
Hydroxychloroqine
Retinopathy
PCP
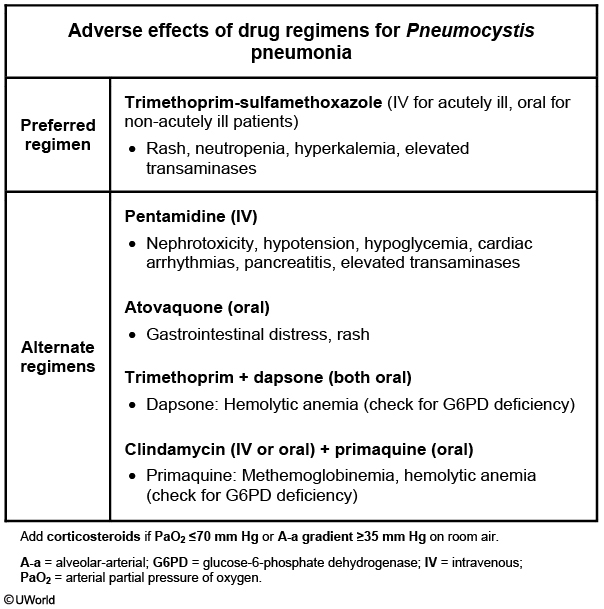
Trimethoprim-sulfamethoxazole (TMP-SMX) is the initial drug of choice for the treatment of PCP regardless of pneumonia severity. Treatment typically lasts for 21 days. Adjunctive corticosteroids have been shown to decrease mortality in cases of severe PCP (possibly by reducing inflammation due to dying organisms). Indications for corticosteroid use include partial pressure of oxygen (PaO2) <70 mm Hg or an alveolar-arterial (A-a) gradient >35 mm Hg on room air.
ABG
HF: The blood gas findings show hypoxia, hypocapnia, and respiratory alkalosis
In COPD exacerbation, examination typically shows widespread bilateral wheezes, and ABG findings include respiratory acidosis and hypoxia.
Gastric outlet
This physical examination maneuver is known as the abdominal succussion splash, which is elicited by placing the stethoscope over the upper abdomen and rocking the patient back and forth at the hips. Retained gastric material >3 hours after a meal will generate a splash sound, indicating the presence of a hollow viscus filled with fluid and gas. Although the test has modest sensitivity and specificity for diagnosing gastric outlet obstruction (GOO), it may suggest the need for more definitive evaluations. Initial management of GOO includes nasogastric suctioning to decompress the stomach, intravenous hydration, and endoscopy for definitive diagnosis.
Asthma
An elevated or even normal PaCO2, as seen in this patient, suggests an inability to meet increased respiratory demands (likely due to respiratory muscle fatigue) and impending respiratory failure. Other clinical signs or symptoms of impending respiratory failure include:
Markedly decreased breath sounds
Absent wheezing
Decreased mental status
Marked hypoxia with cyanosis
Farmer's lung
This patient is most likely suffering from bird fancier's lung, a form of hypersensitivity pneumonitis (HP). HP is caused by repeated inhalation of an inciting antigen, which leads to alveolar inflammation. Common responsible antigens include aerosolized bird droppings ("bird fancier's lung") and molds associated with farming ("farmer's lung"). HP can vary significantly in its clinical presentation and severity. A history of antigen exposure in the setting of compatible symptoms is highly suggestive. Acute episodes may present with cough, breathlessness, fever and malaise that occur 4-6 hours after antigen exposure. With chronic exposure, patients may develop pulmonary fibrosis and a restrictive pattern on lung spirometry. Classic radiographic findings include ground glass opacity, or "haziness," of the lower lung fields. Studies have shown that the best treatment for HP is avoidance of antigen exposure. In many patients, this produces complete remission. Continued exposure risks disease progression.
Aortic Stenosis
Some physical examination findings suggestive of severe AS include:
Diminished and delayed carotid pulse ("pulsus parvus and tardus") due to blood flow obstruction
Mid- to late-peaking systolic murmur from turbulence due to the stenosis
Presence of soft and single second heart sound (S2)
Thickening and calcification of the aortic leaflets leads to reduced mobility and causes a soft S2, as S2 is due mainly to sudden aortic valve closure (A2). In addition, as a result of the reduced mobility, A2 is delayed and occurs simultaneously with pulmonic valve closure (P2), leading to a single S2.
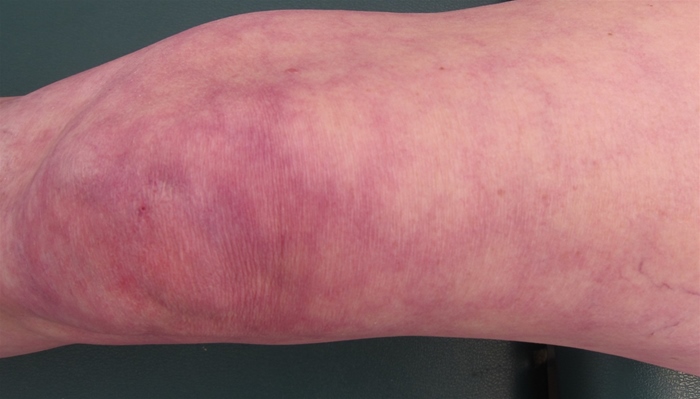
Erysipelas
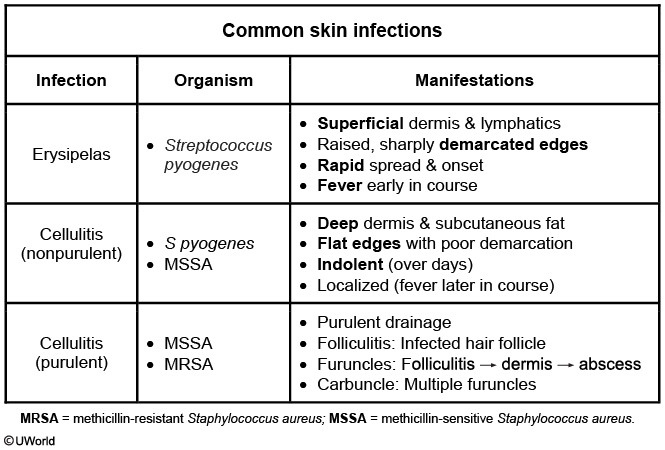
Erysipelas is a skin infection of the upper dermis and superficial lymphatic system most commonly caused by group A Streptococcus. Infections take hold in areas of skin disruption, often due to minor trauma, inflammation, concurrent infection, or edema. Patients rapidly develop systemic symptoms (fever, chills), regional lymphadenitis, and a warm, tender, erythematous rash notable for raised, sharply demarcated borders. Involvement of the external ear is particularly suggestive of erysipelas as this skin lacks a lower dermis level (making cellulitis, a deeper skin infection, unlikely).

The diagnosis of erysipelas is usually based on clinical findings, but blood cultures are useful in patients with extensive rash, systemic toxicity, or underlying comorbidities (eg, diabetes). Most patients receive intravenous antibiotics (eg, ceftriaxone, cefazolin), but those without systemic symptoms may be treated with oral medication (eg, amoxicillin). If possible, the underlying source of skin breach should be addressed to help prevent recurrence.
Hep B
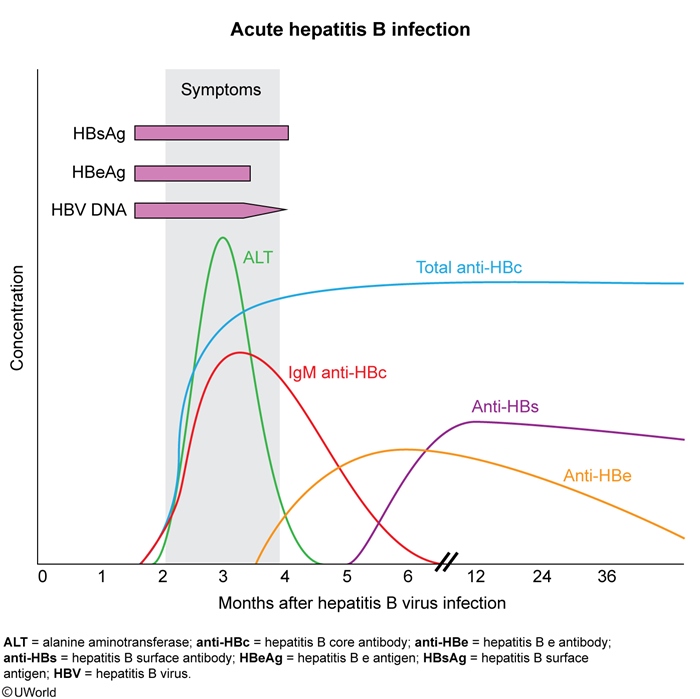
This patient's new-onset symptoms (eg, fatigue, nausea/abdominal pain, dark urine) and abnormal liver function tests (eg, elevated serum transaminases, hyperbilirubinemia) in the setting of unprotected sex with multiple partners is concerning for acute hepatitis B infection. The first serologic marker to appear in the serum with acute hepatitis B is HBsAg, which appears usually 4-8 weeks after infection. IgM anti-HBc appears shortly thereafter, which is around the time clinical symptoms occur and patients develop elevations in hepatic aminotransferase levels (often >25 times the normal limit).
There can be a time lag (weeks to months) between the disappearance of HBsAg and the appearance of anti-HBs, which is termed the window period. IgM anti-HBc may be the only detectable marker for acute hepatitis B infection during this period. As such, HBsAg and anti-HBc are the most appropriate diagnostic tests for acute hepatitis B infection as these are both elevated during initial infection and anti-HBc will remain elevated during the window period.
Hepatitis B virus DNA is obtained in patients with chronic hepatitis B to determine candidacy for antiviral therapy or monitor response to treatment.
HIV vaccines
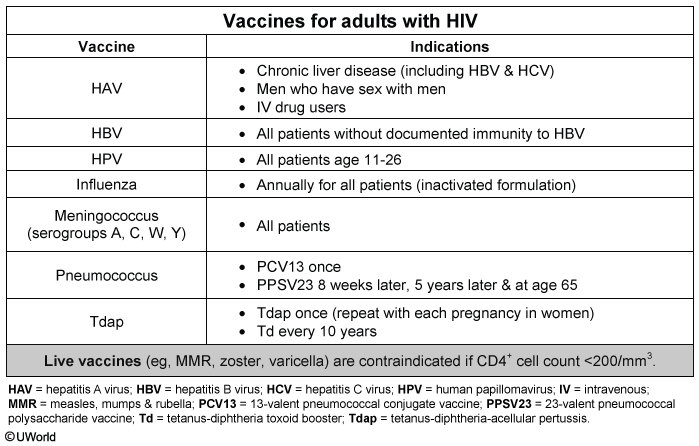
As with all adults, patients with HIV should receive vaccination for influenza annually in the fall (but with the inactivated formulation rather than the live, attenuated or nasal formulations). They should also receive revaccination for tetanus and diphtheria (Td) every 10 years, with a single dose of tetanus-diphtheria-acellular pertussis (Tdap) recommended to address waning pertussis immunity, particularly in those who have not previously received Tdap.
Patients with HIV should receive the following additional vaccines due to elevated risk:
They should receive vaccination for hepatitis B unless they have documented immunity (as in this patient with positive hepatitis B surface antibody results).
They also should receive vaccination for Streptococcus pneumoniae with the 13-valent pneumococcal conjugate vaccine (PCV13), followed by the 23-valent pneumococcal polysaccharide vaccine (PPSV23) 8 weeks later and again in 5 years and at age 65.
Many experts also recommend varicella vaccine for adults with HIV born after 1979 who do not have evidence of immunity, provided that their CD4+ count is >200/mm3. This patient would be eligible for the vaccine given his negative anti-varicella IgG antibody result.
HIV itself is not an indication for meningococcal vaccination, which would be recommended only if the patient were at otherwise increased risk (eg, asplenia, complement deficiency).
Post op endophthalmitis
Postoperative endophthalmitis is the most common form of endophthalmitis. It usually occurs within six weeks of surgery. It is an infection within the eye, particularly the vitreous. Patients usually present with pain and decreased visual acuity. Examination reveals swollen eyelids and conjunctiva, hypopyon, corneal edema and infection. The vitreous can be sent for Gram stain and culture. Based on the severity, intravitreal antibiotic injection or vitrectomy is done.
Warfarin
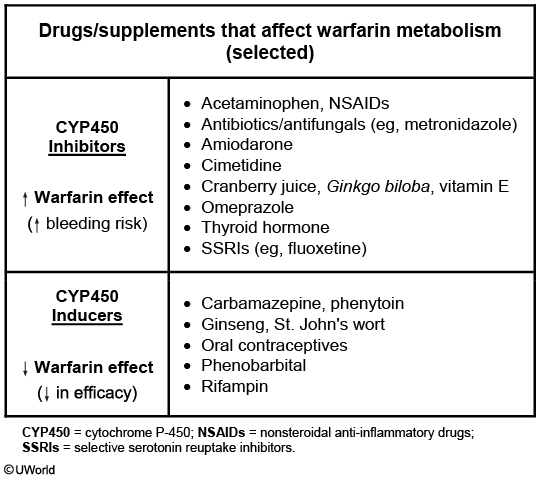
The table summarizes commonly used drugs, herbal supplements, and over-the-counter medications that affect warfarin metabolism, vitamin K synthesis, and vitamin K metabolism. These interactions can either increase the effect of warfarin to increase bleeding risk or decrease the drug's effect to increase thrombosis risk. Acetaminophen taken at higher doses (>2 g/day) for >1 week may significantly increase the anticoagulant effects of warfarin. Although the exact mechanism is unclear, this interaction is likely mediated via enzyme inhibition in vitamin K metabolism.
Brussels sprouts and spinach are excellent sources of vitamin K and decrease the anticoagulant effects of warfarin. Ginseng is also known to decrease the serum concentration of warfarin. Their use would ultimately decrease the risk of bleeding episodes and increase thrombosis risk.
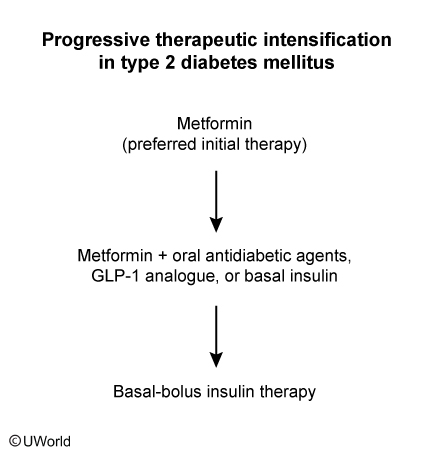
Type 2 DM
BP
weight loss
dash diet
exercise
sodium intake
alcohol cessation
Gout Xray

Gout causes an inflammatory effusion and needle-shaped, negatively birefringent crystals; x-rays characteristically show punched-out erosions with a rim of cortical bone.
Paget
Typical findings on imaging include cortical thickening and osteolytic or mixed lytic/sclerotic lesions on x-ray as well as focally increased radiotracer uptake on bone scan.,

Ichthyosis Vulgaris
This patient has ichthyosis vulgaris, a chronic, inherited skin disorder characterized by diffuse dermal scaling. It is caused by mutations in the filaggrin gene and is significantly worse in individuals who are homozygous. The skin appears dry and rough with horny plates resembling fish or reptile scales ("ikhthýs" is Greek for "fish"). Ichthyosis is a lifelong condition, but symptoms in early life are frequently mild and may be attributed to simple dryness. However, the condition often worsens later in life, leading to the diagnosis.
Ichthyosis often worsens in the winter due to decreased ambient humidity. If simple emollients are ineffective, keratolytics (eg, coal tar, salicylic acid) and topical retinoids are useful for controlling symptoms.

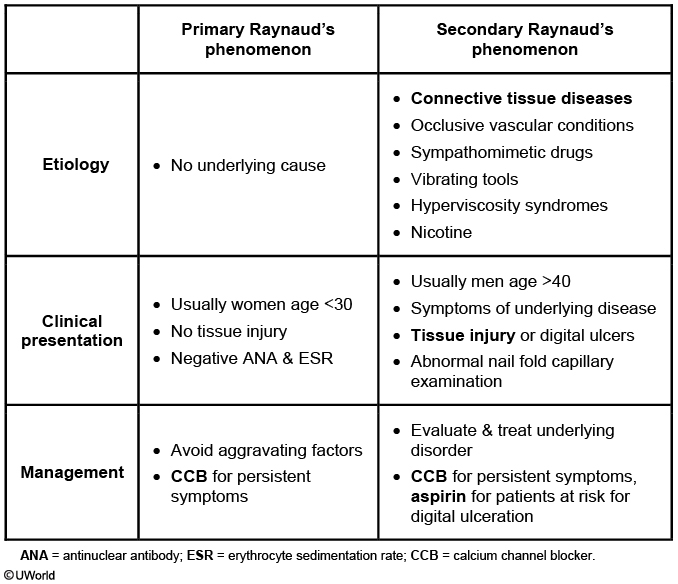
Raynaud
Chronic Prostatitis
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), typically defined as chronic pelvic pain (including pain in the perineum and testes, which can radiate to the back) for >3 months without an identifiable cause, can present as voiding difficulties, irritative voiding symptoms (eg, frequency, urgency, hesitancy), pain with ejaculation, or blood in the semen. Patients are generally afebrile and have little or no prostate tenderness (despite the term "prostatitis"), with a normal urinalysis and negative urine culture results. Prostate-specific antigen levels are often normal. There is usually no history of urinary tract infection. CP/CPPS can be categorized as inflammatory or noninflammatory based on the presence of leukocytes in urine and prostatic secretions, but this distinction has uncertain clinical significance. The exact etiology of CP/CPPS is unclear, but it is thought to be due tononinfectious chronic prostate inflammation.
CP/CPPS is a diagnosis of exclusion, and additional testing (eg, scrotal ultrasound, cystoscopy) is individualized based on the patient's particular clinical features. Even though a bacterial cause is not known, antibiotics (eg, fluoroquinolones) are often helpful in symptom relief. Other interventions include alpha-adrenergic inhibitors (eg, tamsulosin) and 5-alpha-reductase inhibitors (eg, finasteride).
Chronic bacterial prostatitis (not to be confused with CP/CPPS) presents with dysuria and urinary frequency, but patients often have a history of urinary tract infection, prostatic tenderness or induration, and a positive urine culture. Acute bacterial prostatitis is characterized by fever, perineal pain, and severe tenderness on prostate examination.
FAP
Guidelines generally recommend annual screening sigmoidoscopies for children starting at age 10-12, followed by annual colonoscopies once colorectal adenomas are detected or if the patient is age >50. Patients with the attenuated version of FAP can have a delayed start of screening (age 25) and longer screening intervals (1-2 years). In addition to colonoscopies, patients with FAP should also undergo regular screening for upper gastrointestinal tract tumors.
Proctocolectomy should be performed in patients who initially present with CRC or adenomas with high-grade dysplasia. Other indications for colorectal surgery include severe symptoms from colonic neoplasia (eg, hemorrhage) or a significant increase in polyp number during the screening interval. In patients with classic FAP who do not have any of the above findings, surgery does not need to be performed urgently and may be delayed until early twenties
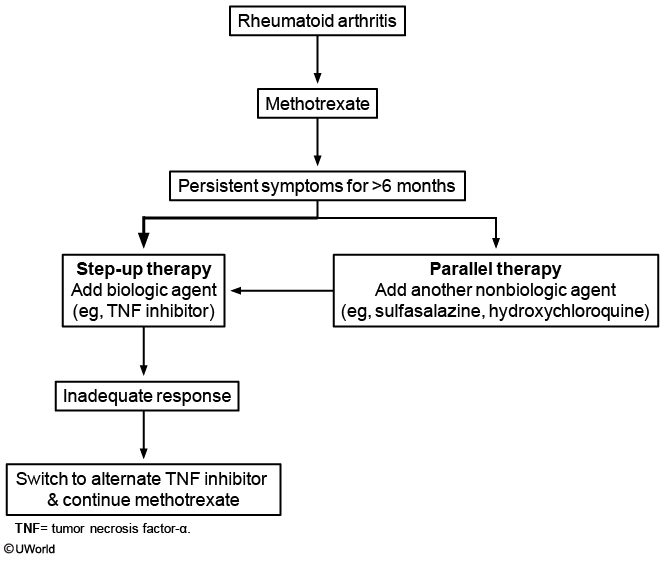
RA
Macular Degen
One of the earliest findings in macular degeneration is distortion of straight lines such that they appear wavy. The grid test described above is frequently used to screen for patients with macular degeneration.
SBP
SBP is most likely due to either intestinal bacterial translocation directly into the ascitic fluid or hematogenous spread to the liver and ascitic fluid (due to other bacterial infections).
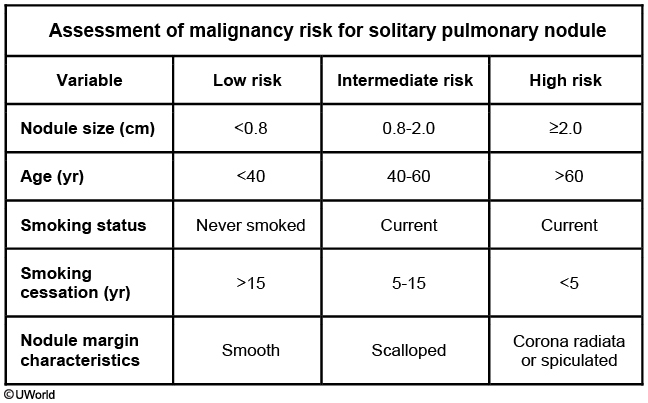
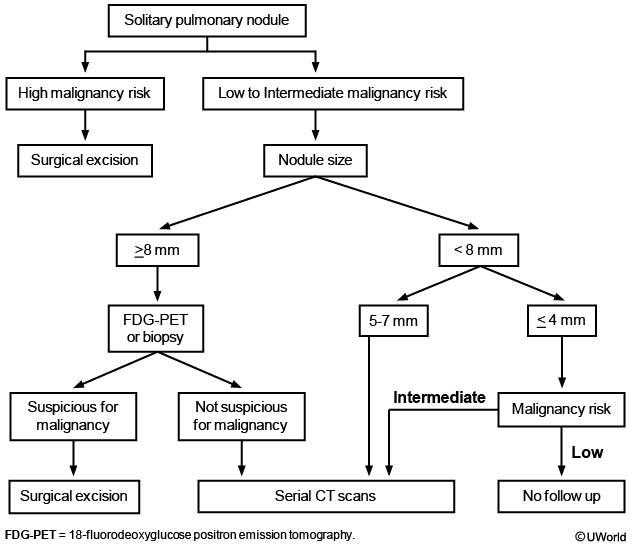
Solitary Pulmonary Nodules
A solitary pulmonary nodule (SPN) is defined by the following features:
Rounded opacity
<3 cm
Completely surrounded by pulmonary parenchyma
No associated lymph node enlargement
MM

This patient with constipation, back pain, and laboratory evidence of anemia, renal insufficiency, and hypercalcemia likely has multiple myeloma (MM). MM is a plasma cell neoplasm that commonly presents with manifestations related to bone marrow infiltration (bone pain, fractures, hypercalcemia, anemia) or elevations in serum monoclonal protein (renal insufficiency). At the time of diagnosis, approximately 25% of patients with MM have hypercalcemia. Typically, this is a result of osteolytic bone destruction by the neoplastic plasma cells. Although hypercalcemia may be asymptomatic with a calcium level <12 mg/dL, fatigue,constipation, and depression are common. This patient's constipation is likely a result of hypercalcemia.
HPV
HPV vaccination is recommended for both male and female patients at age 11-12 and may be considered as early as age 9. For patients who did not receive the initial vaccine series, it is recommended through age 26 for women and through age 21 for men.
Acute Limb Ischemia
The patient has the classic clinical presentation of acute arterial occlusion of the left lower extremity (acute limb ischemia): pain, pallor, poikilothermia (cool extremity), paresthesia, pulselessness, and paralysis (6 Ps). This is most likely due to thromboembolic occlusion from left atrial thrombus due to atrial fibrillation(irregular heartbeat) in a patient with preexisting peripheral vascular disease (multiple risk factors, intermittent claudication, diminished pulses).
Patients with suspected acute arterial occlusion leading to an immediately-threatened limb (sensory loss, rest pain, muscle weakness) should be immediately started on anticoagulation while further diagnostic procedures are performed. Heparin prevents further thrombus propagation and thrombosis in the distal arterial and venous circulation.
Ankle-brachial index (ratio of systolic pressure in ankle to that in arm) is often used as a screening and/or diagnostic tool in patients with suspected peripheral arterial disease (PAD). Although this patient likely has PAD, the more acute limb-threatening complication should be addressed first.
Arterial Doppler study or duplex ultrasonography can identify the presence and location of acute arterial occlusion; however, the clinical suspicion for acute embolic occlusion in this patient is so high that anticoagulation initiation should not be delayed while obtaining additional confirmatory testing.
HIV retinitis
In an immunocompromised individual, HSV retinitis may be characterized by rapidly progressing bilateral necrotizing retinitis (referred to as the "acute retinal necrosis syndrome"). This patient's clinical presentation is suggestive of acute retinal necrosis most likely due to HSV. The initial symptoms are keratitis and conjunctivitis with eye pain, followed by rapidly progressive visual loss. Funduscopy reveals widespread, pale, peripheral lesions and central necrosis of the retina.
HSV infection of the eye is the most common cause of corneal blindness in the United States.
CMV retinitis is the most common serious ocular complication of HIV-positive patients; however, it is typically painless, and funduscopy shows fluffy or granular retinal lesions located near the retinal vessels and associated hemorrhages. It does not usually cause initial conjunctivitis or keratitis, as in this patient.
Epidydimidis
Epididymitis
Epidemiology
Age les than 35: Sexually transmitted (chlamydia, gonorrhea) Age >35: Bladder outlet obstruction (coliform bacteria)
Symptoms
Unilateral testicular pain Epididymal edema Dysuria, frequency (with coliform infection)
Diagnosis
Urinalysis/culture NAAT for chlamydia & gonorrhea
Treatment
Ceftriaxone/doxycycline (if STI) Levofloxacin (if coliform bacteria)
Pyelo
Acute pyelonephritis
Uncomplicated
Otherwise healthy, nonpregnant Primarily Escherichia coli Oral fluoroquinolone, trimethoprim-sulfamethoxazole Intravenous antibiotics if vomiting, elderly, septic
Complicated
Diabetes, urinary obstruction/instrumentation, renal failure, immunosuppression, hospital-acquired ↑ Risk of antibiotic resistance/treatment failure Intravenous fluoroquinolone, aminoglycoside, extended spectrum beta-lactam/cephalosporin
Osteomyelitis
Pseudomonas infections are particularly prevalent after puncture wounds through the sole of a shoe as the warm, moist environment is quite hospitable to this microorganism.
Malaria
The effective prevention of malaria relies on a thorough understanding of endemic strains, antimicrobial resistance, and relative risk of infection. Travelers new to an endemic region or those returning after a long absence are at high risk of clinical illness and require chemoprophylaxis. India is a malaria endemic country with a high prevalence of both Plasmodium falciparum and P vivax. Chloroquine resistance is common; therefore, travelers are usually given chemoprophylaxis with atovaquone-proguanil, doxycycline, or mefloquine. Mefloquine treatment should begin >2 weeks prior to travel, continued during the stay, and discontinued 4 weeks after returning. Neuropsychiatric side effects (eg, anxiety, depression, restlessness) occur in approximately 5% of patients and should prompt a change to an alternate medication.
In addition to chemoprophylaxis, travelers are advised to prevent mosquito bites with protective clothing, insect repellent, and insecticide-treated bed netting.
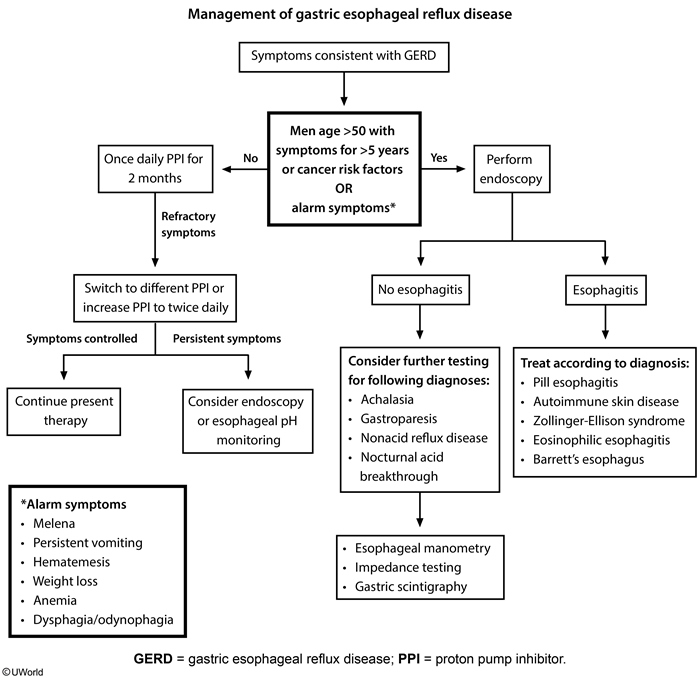
Gerd
Chest Pain
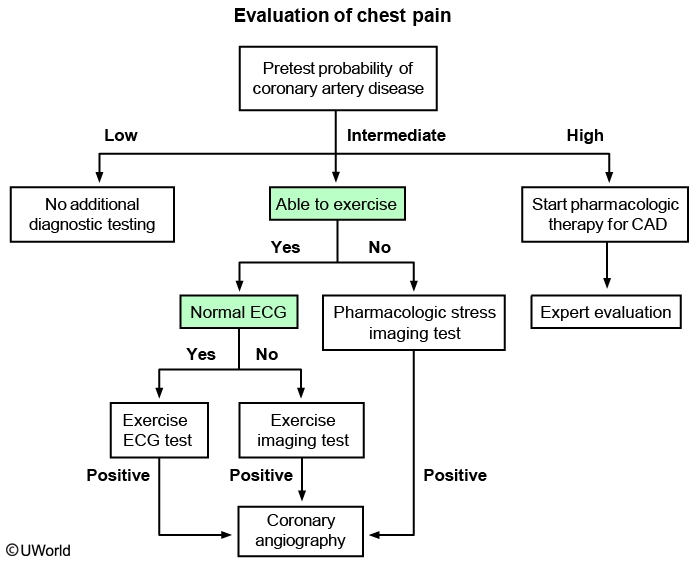
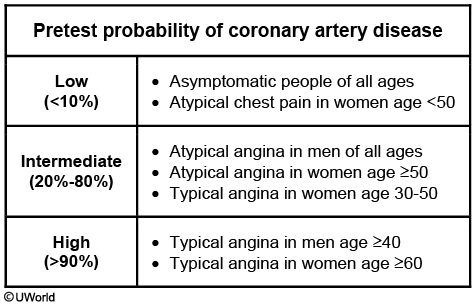
Classification
Classic
Typical location (eg, substernal), quality & duration Provoked by exercise or emotional stress Relieved by rest or nitroglycerin
Atypical
2 of the 3 characteristics of classic angina
Nonanginal
<2 of the 3 characteristics of classic angina
Ingestion
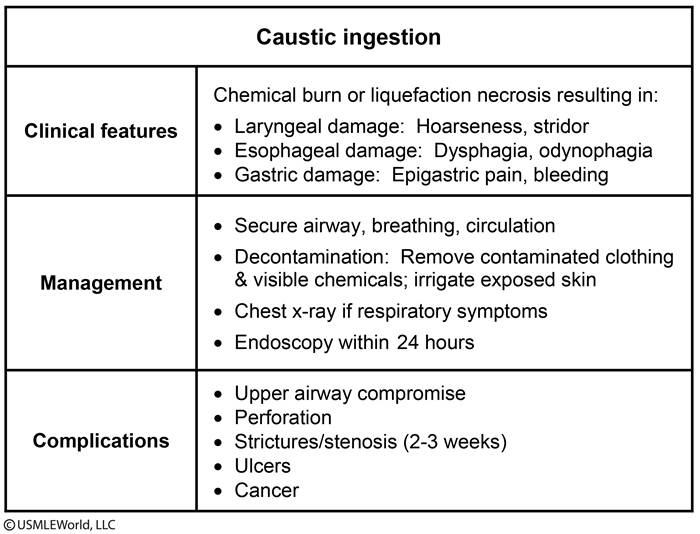
This patient's presentation is consistent with a likely suicide attempt by ingestion of sodium hydroxide (lye), a strongly caustic alkaline solution. The severity of caustic esophageal injury depends on the ingested substance's corrosive properties, amount and concentration, and duration of contact with the mucosa. Patients typically develop vomiting with occasional hematemesis, dysphagia/odynophagia, retrosternal or epigastric pain, and hypersalivation. Absence of oral injury does not rule out significant esophageal damage.
Alkali ingestion can cause immediate chemical burn or liquefaction necrosis in the esophagus that spreads within seconds to minutes through the esophageal wall toward the mediastinum. Possible complications include perforation and mediastinitis. This process can last for 3-4 days with slow mucosal healing over the next 1-3 months. Patients should initially undergo decontamination of skin and clothing and receive intravenous hydration. Serial chest and abdominal x-rays should be obtained to identify any perforation. Upper gastrointestinal x-ray study with water-soluble contrast should be performed in patients with suspected perforation.
In the absence of perforation or severe respiratory distress, early endoscopic evaluation within the first 12-24 hours is recommended in hemodynamically stable patients to assess the severity of esophageal damage. Patients with no or mild esophageal injury may be managed with simple supportive measures. However, more severe injury may require tube feedings and possible surgery (esophagectomy).
Pleural Effusion
Normal pleural fluid pH is approximately 7.60. Transudative fluid is usually due to systemic factors (eg, increased hydrostatic pressure or hypoalbuminemia) and has a pleural fluid pH of 7.4-7.55. Exudate is usually due to inflammation with a pleural fluid pH of 7.30-7.45. Pleural fluid pH <7.30 (with normal arterial pH and low pleural glucose) is usually due to increased acid production by pleural fluid cells and bacteria (eg, empyema) or decreased hydrogen ion efflux from the pleural space (eg, pleuritis, tumor, pleural fibrosis).
DVT/PE
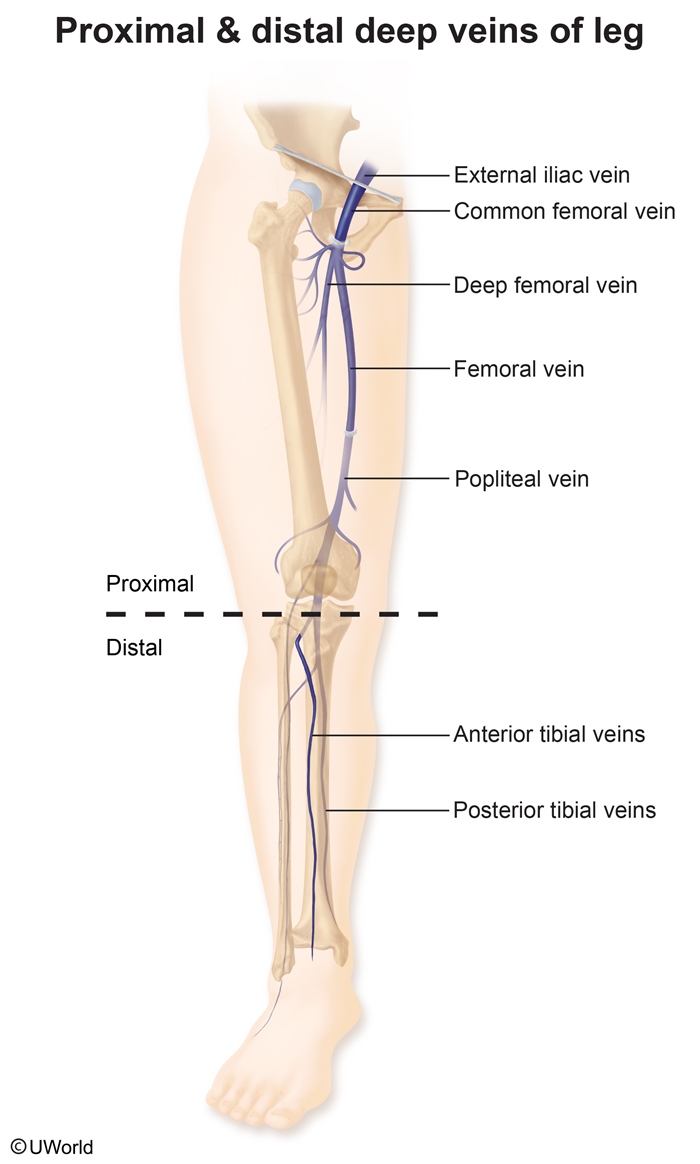
The finding of a thrombus in the right pulmonary artery on CT angiogram is diagnostic of pulmonary embolus (PE). The deep veins of the lower extremities are the most frequent source. Lower extremity deep vein thrombosis (DVT) is divided into 2 categories:
Proximal/thigh (eg, iliac, femoral, popliteal): These are the source of >90% of acute PEs, probably due to their large caliber and proximity to the lungs.
Distal/calf: These are less likely to embolize and more likely to spontaneously resolve.
Effect Modification
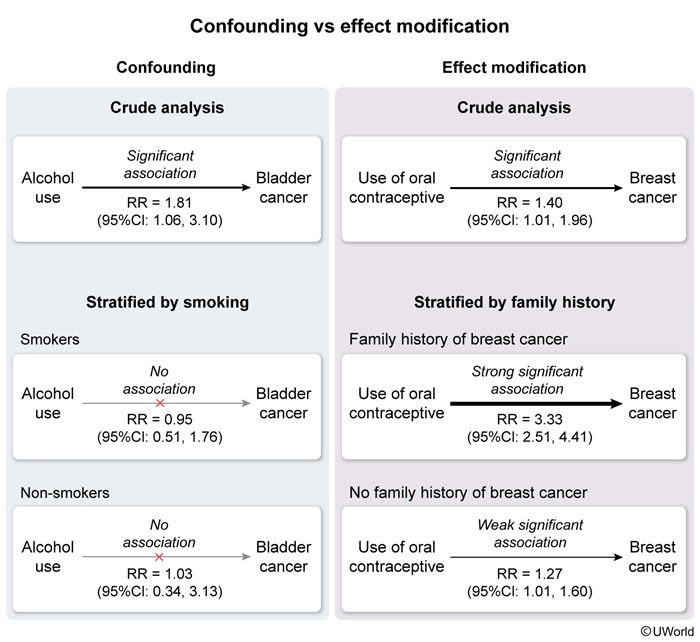
Effect modification (interaction) results when an extraneous variable (modifier)changes the direction or strength of an association between a risk factor and a disease. A modifier is associated with the disease but not the risk factor. Effect modification can sometimes be confused with confounding, the bias that results when the exposure-disease relationship is obscured by the effect of an extraneous factor (confounder) associated with both exposure and disease.
Stratified analysis by the extraneous variable can help distinguish whether that variable is a confounder or an effect modifier, as follows:
Confounder (left panel): The measures of association (eg, relative risk [RR] of bladder cancer among alcohol users) calculated in each of the stratified groups (eg, smokers and nonsmokers) are similar to one another (eg, nonstatistically significant RR = 0.95 [95%CI: 0.51, 1.76] and RR = 1.03 [95%CI: 0.34, 3.13]), but they differ from the measure of association calculated in the crude analysis (eg, statistically significant RR = 1.81 [95%CI: 1.06, 3.10]); stratification can remove the effects of the confounder (eg, smoking).
Effect modifier (right panel): The measures of association calculated in each of the strata are significantly different (in strength or direction) from one another; stratification can make the effects of the modifier more apparent.
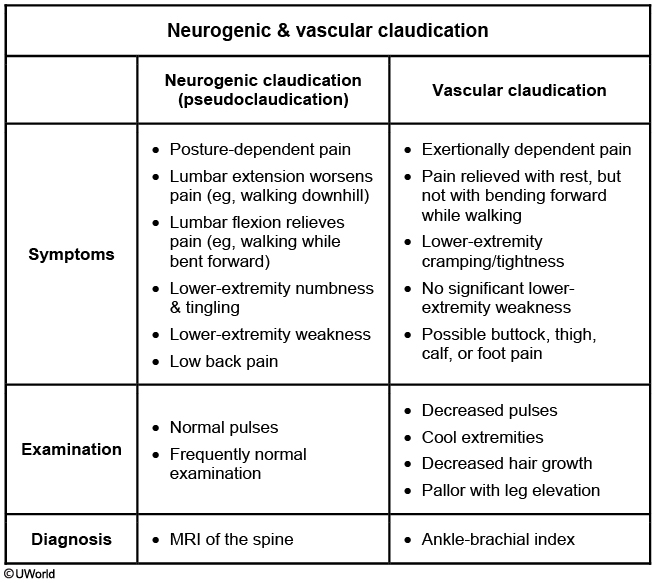
Claudication
Spider angioma
In patients with cirrhosis, spider angioma and palmar erythema both arise from hyperestrinism due to impaired hepatic metabolism of circulating estrogens, a process that begins in the cytochrome P450 system. Circulating estrogens affect vascular wall dilation. Spider angioma consists of a central, dilated arteriole surrounded by smaller radiating vessels. Palmar erythema is a result of increased normal speckling of the palm due to increased vasodilation, especially at the thenar and hypothenar eminences. Other manifestations of hyperestrinism in patients with cirrhosis include gynecomastia, testicular atrophy, and decreased body hair in males.
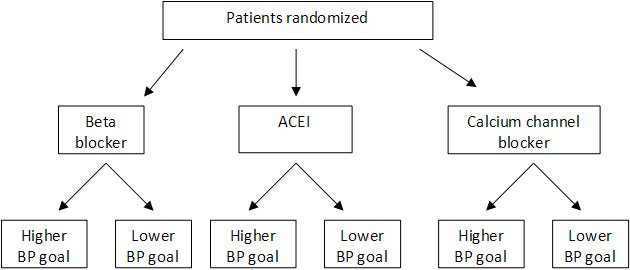
Factorial Design
HTN and Hypokalemia
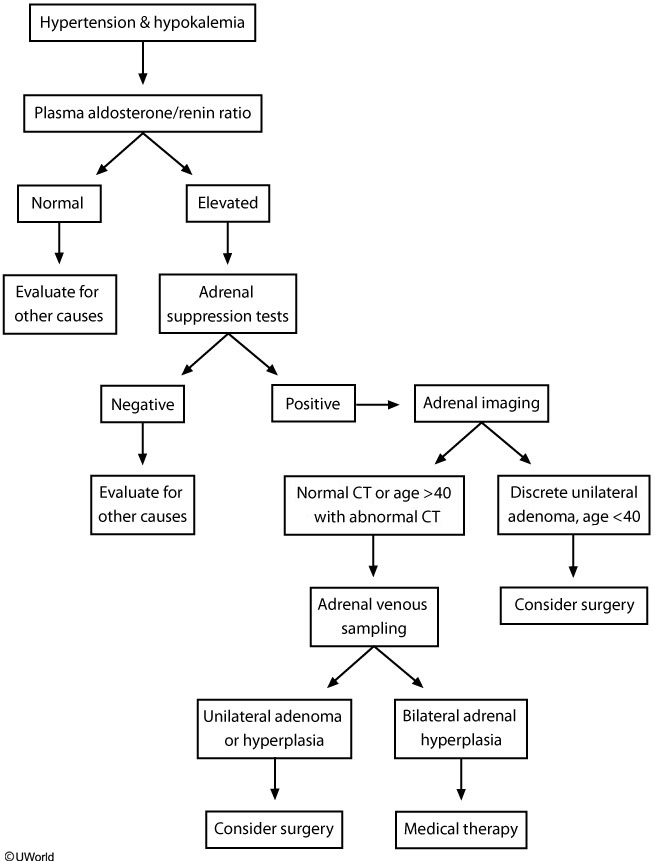
The best screening test is early-morning plasma aldosterone concentration (PAC) to plasma renin activity (PRA) ratio. However, drugs that significantly alter the PAC/PRA ratio (eg, spironolactone, eplerenone, amiloride, triamterene) should be withdrawn for 4 weeks before testing. A PAC/PRA ratio >20 with plasma aldosterone >15 ng/dL suggests primary hyperaldosteronism and requires further confirmatory adrenal suppression testing. Adrenal suppression testing usually involves salt loading and documenting inability to suppress serum aldosterone. Patients with positive adrenal suppression testing should then undergo adrenal imaging, usually by computed tomography (CT) scan
Marijuana
This patient's clinical presentation and examination findings are most consistent with acute cannabis (marijuana) intoxication. Signs of marijuana intoxication include tachycardia, tachypnea, hypertension, dry mouth, conjunctival injection, and increased appetite. Marijuana slows reaction time; causes slurred speech; and impairs coordination, attention, concentration, and short-term memory. Impairment of cognition, judgment, and coordination can last much longer than the acute euphoric effect, affecting the ability to operate automobiles and increasing the risk of motor vehicle collisions. Patients with cannabis intoxication are managed supportively.
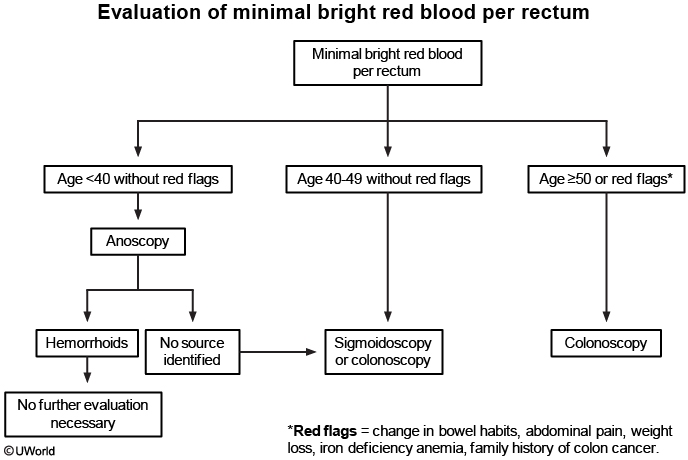
Blood rectum
Dermatofibroma
This patient's skin lesion is consistent with a dermatofibroma (DF), which is due to fibroblast proliferation causing isolated or multiple lesions, most commonly on the lower extremities. The etiology is unknown, but some patients may develop lesions after trauma or insect bites. Typical lesions are nontender and appear as discrete, firm, hyperpigmented nodules that are usually <1 cm in diameter. The lesions have a fibrous component that may cause dimpling in the center when the area is pinched ("dimple" or "buttonhole" sign).
Diagnosis of DF is made clinically based on the appearance of the lesion. Treatment (cryosurgery or shave excision) is usually not required unless the lesion is symptomatic, bleeds, or changes in color or size. Patients may also request treatment for cosmetic reasons or because of recurrent cuts when shaving the legs.

Pyogenic granuloma

Pyogenic granuloma is a benign vascular skin tumor that presents as a small red papule that grows rapidly over weeks or months to a pedunculated or sessile shiny mass. The lesions most commonly occur on the lip and oral mucosa and can bleed with minor trauma.
Cholesterol emboli
This patient most likely has atheroembolism (cholesterol embolism) caused by recent cardiac catheterization. Atheroembolism occurs when an atherosclerotic plaque is disrupted and cholesterol crystals and debris are showered into the circulation. This leads to partial or total occlusion of arterioles with resultant tissue or organ ischemia. Risk factors for atheroembolism are advanced age, obesity, smoking, hypercholesterolemia, hypertension, and diabetes. Atheroembolism is most commonly seen as a complication of cardiac catheterization and other vascular procedures.
Clinical manifestations can be immediate or delayed (>30 days after inciting event). Atherosclerotic plaques in the aortic arch can embolize to the brain and cause cerebral infarction. Diffuse showering of emboli into the peripheral circulation can cause intestinal ischemia, gastrointestinal bleeding, pancreatitis, and acute kidney injury. Skin manifestations are the most common complication (34% of patients) and include "blue toe syndrome" (cyanotic toes with intact pulses), livedo reticularis (reticular, lacy skin discoloration/erythema that blanches on pressure), gangrene, and ulcers. Examination of the retina may show Hollenhorst plaques, bright, yellow, refractile plaques in the retinal artery, which indicate a proximal source such as the internal carotid artery.
Treatment of atheroembolism is primarily supportive. Atheroembolism also reinforces the indication for statin therapy in patients with atherosclerotic vascular disease. Some patients may have renal dysfunction that persists beyond 2 weeks (compared to contrast nephropathy, which usually resolves within 1 week).

Prostate mets
Flutamide is a non-steroidal anti-androgen which provides androgen blockade by competitively binding to dihydrotestosterone receptors. This drug, when combined with a LHRH agonist, prolongs the survival of patients with limited disease. However, there have been no demonstrable benefits in patients who underwent orchiectomy, as in this patient.
Radiation therapy is the most appropriate for the management of progressive pain in a patient with prostate cancer and bony metastases after androgen ablation (orchiectomy).
Malignant Hypertension
Malignant hypertension is usually seen in patients with long-standing and uncontrolled hypertension. It is associated with retinal hemorrhages, exudates, and/or papilledema. Patients also can develop malignant nephrosclerosis (acute renal failure, hematuria, and proteinuria). However, renal findings are not always present and are not required for the diagnosis of malignant hypertension
Pill Esophagitis
This patient has abrupt-onset retrosternal pain and severe odynophagia, suggestive of medication-induced esophagitis (pill esophagitis). Pill esophagitis is due to a direct effect of certain medications on esophageal mucosa. Mucosal injury in pill esophagitis can be due to acid effect (eg, tetracyclines), osmotic tissue injury (eg, potassium chloride), or disruption of normal gastroesophageal protection (eg, nonsteroidal anti-inflammatory drugs). Patients usually do not have prior esophageal disease, although pill esophagitis can be worse in those with concurrent gastroesophageal reflux.
Typical symptoms of pill esophagitis include sudden-onset odynophagia and retrosternal pain that can sometimes cause difficulty swallowing. It is most common in the mid-esophagus due to compression by the aortic arch or an enlarged left atrium. The diagnosis is usually made clinically but can be confirmed on endoscopy, which shows discrete ulcers with relatively normal-appearing surrounding mucosa. Treatment includes primarily stopping the offending medication to prevent future injury.
Septic Emboli
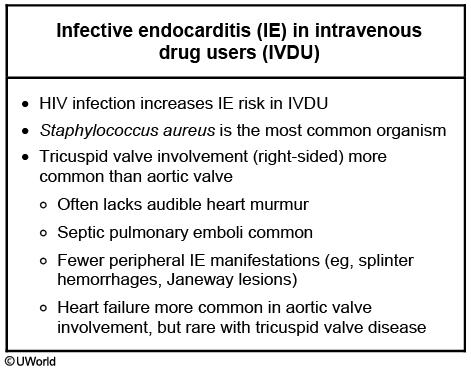
This patient's presentation (pulmonary symptoms, history of intravenous drug abuse with track marks, and cavitary lesions on imaging) suggests septic embolism from infective endocarditis (IE). HIV greatly increases IE risk in intravenous drug users (IVDU), most commonly at the tricuspid valve. Patients typically present with systemic symptoms (eg, fever, chills), pleuritic chest pain, dyspnea, and/or cough. However, there may not be a tricuspid valve murmur on cardiac examination due to the relatively low pressure gradient across the valve. Peripheral manifestations (eg, splinter hemorrhages, Janeway lesions) are also less common in patients with tricuspid valve disease.
IE diagnosis in IVDU can be difficult and requires a high degree of suspicion. Septic pulmonary emboli occur in up to 75% of patients with tricuspid endocarditis, most commonly due to Staphylococcus aureus in IVDU with IE. Imaging may show pulmonary septic emboli as pulmonary infiltrates, abscesses, infarction, pulmonary gangrene, or cavities, as seen in this patient's CT scan. These lesions are typically located in lung periphery.
Acne
Initial management for inflammatory acne includes topical retinoids and benzoyl peroxide. However, most patients with moderate or moderate-to-severe inflammatory acne require topical antibiotics (eg, erythromycin, clindamycin). Oral antibiotics (eg, tetracyclines) are reserved for patients with severe or nodular acne and for moderate acne unresponsive to topical antibiotics. Oral antibiotics are also considered in patients with widespread acne (eg, on the back or upper arms) that makes topical therapy impractical.
HS

This patient has hidradenitis suppurativa (HS, also known as acne inversa). It most commonly occurs in intertriginous areas (eg, axilla; inguinal, perineal areas) but can occur in any hair-bearing skin. HS is due to chronic inflammatory occlusion of folliculopilosebaceous units, which prevents keratinocytes from properly shedding from the follicular epithelium. Risk factors include family history of HS, smoking, obesity, diabetes, and mechanical stress on the skin (eg, friction, pressure).
HS initially presents as solitary, painful, inflamed nodules that can last for several days to months. The nodules may regress or can progress to abscesses that open to the surface with purulent or serosanguineous drainage. Most patients have a chronic, relapsing course. Complications include sinus tracts, comedones, and scarring. Severe scarring can lead to dense, rope-like bands in the skin with strictures and lymphedema. The diagnosis of HS is usually made clinically without the need for biopsy or cultures.
Dysphagia
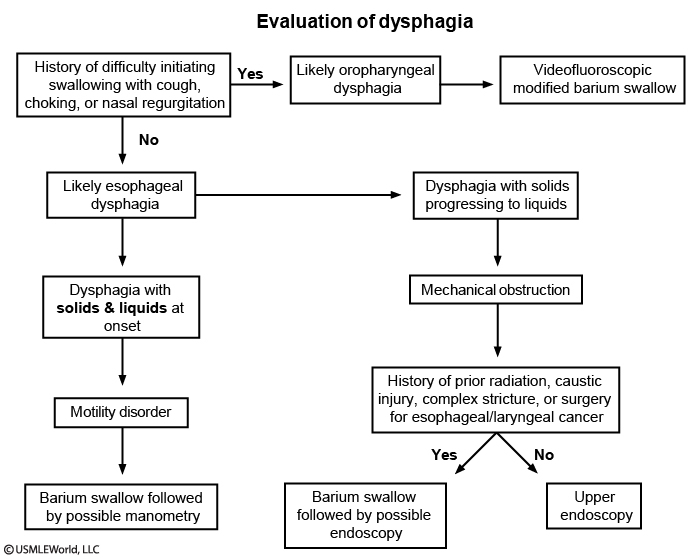
Dysphagia can be classified as oropharyngeal or esophageal. Oropharyngeal dysphagia presents with difficulty initiating swallowing due to inability to properly transfer food from the mouth to the pharynx. Underlying etiologies for oropharyngeal dysphagia can include stroke, advanced dementia, oropharyngeal malignancy, or neuromuscular disorders (eg, myasthenia gravis).
Patients with oropharyngeal dysphagia can also have associated coughing, choking, or nasal regurgitation on swallowing. Other complications can include aspiration pneumonia and weight loss. This patient's history of stroke with coughing and choking on swallowing suggests oropharyngeal dysphagia. Recurrent right lower lobe pneumonia suggests likely aspiration pneumonia. Videofluoroscopic modified barium swallow study is preferred initially in these patients to evaluate swallowing mechanics, degree of dysfunction, and severity of aspiration.
Crystalline Nephropathy
Drugs: acyclovir, methotrexate, sulfonamides, protease inhibitors, uric acid (tumor lysis), ethlyene glycol
The kidney rapidly excretes acyclovir into the urine, but the drug has low urine solubility. As a result, it easily precipitates in renal tubules, causing intratubular obstruction and direct renal tubular toxicity. Crystal-induced AKI is more common with large intravenous doses of acyclovir and occurs only rarely with oral acyclovir. Intravenous acyclovir less commonly causes AKI through acute tubular necrosis or acute interstitial nephritis.
Risk factors for crystal-induced AKI include underlying volume depletion or chronic kidney disease. Most patients develop AKI within 24-48 hours after drug exposure and can be asymptomatic or develop nonspecific symptoms (eg, nausea, flank/abdominal pain). Urinalysis can show hematuria, pyuria, and crystals visualized with a polarizing microscope. Treatment involves discontinuing the drug and providing volume repletion. Administration of intravenous fluids for adequate hydration while giving the drug can also prevent AKI.
Tourniquet test
dengue fever
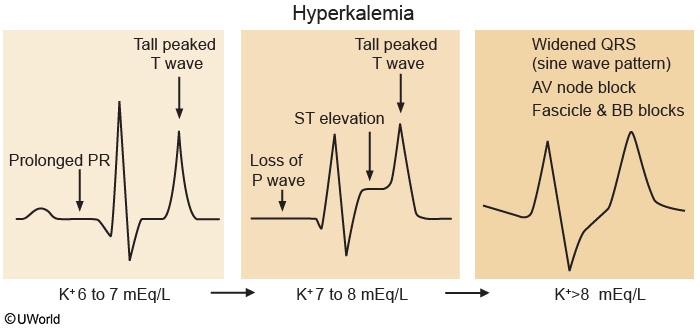
Hyperkalemia
PML
Symptoms include altered mental status, motor deficits, ataxia, and vision abnormalities (eg, diplopia). CT of the brain with contrast usually reveals nonenhancing, hypodense white matter lesions with no surrounding edema. Diagnosis requires lumbar puncture with cerebral spinal fluid evidence of JC virus (by PCR). Brain biopsy is occasionally required. Patients with AIDS are treated withantiretroviral therapy; this may prevent death, but significant neurologic impairment often remains.
HIV-associated dementia usually affects deep gray matter structures and causes subacute cognitive, behavioral, and motor deficits. Imaging reveals cerebral atrophy with ventricular enlargement.
Episcleritis vs Uveitis
Anterior uveitis (iritis) is the most common extraarticular manifestation of AS and occurs in 25%-40% of patients. It is characterized by inflammation of the uveal tract (iris, ciliary body, and choroid). Anterior uveitis typically presents with intense pain and photophobia in one eye.
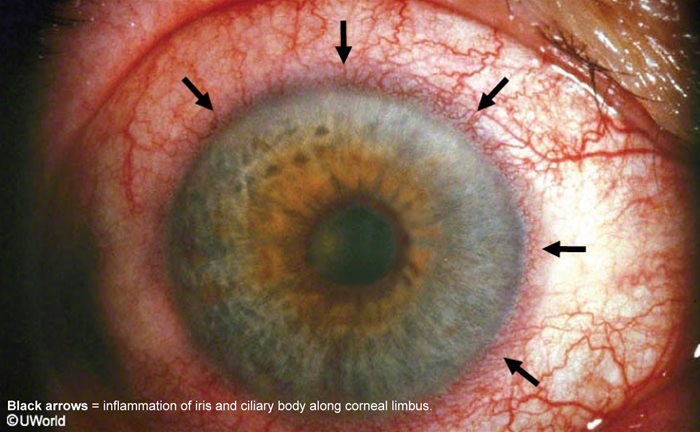
Episcleritis is characterized by inflammation seen at the white of the eye, without involvement of the uveal tract. It is most strongly associated with rheumatoid arthritis and inflammatory bowel disease but is not associated with AS.
Pseudoachalasia
This patient's presentation, with dysphagia to solids and liquids and a dilated esophagus with smooth tapering of the distal esophagus, suggests either primary achalasia (ie, loss of peristalsis in the distal esophagus with lack of lower esophageal sphincter relaxation) or pseudoachalasia due to esophageal cancer. Several clues point to pseudoachalasia (eg, narrowing of distal esophagus not due to denervation) caused by malignancy.
Tobacco use is a major risk factor for esophageal adenocarcinoma and squamous cell carcinoma; alcohol use is also an important risk factor for esophageal squamous cell carcinoma. Significant weight loss, rapid symptom onset (less than 6 months), and presentation at age >60 all increase the likelihood of malignancy (by comparison, patients with achalasia have symptoms for approximately 5 years before receiving a diagnosis, and they typically only have mild weight loss). Tumor metastasis (eg, mediastinal lymph nodes) or local involvement may give a radiologic appearance similar to that seen with a widened mediastinum. Endoscopic evaluation can differentiate between achalasia and pseudoachalasia. In achalasia, this evaluation usually shows normal-appearing esophageal mucosa and a dilated esophagus with possible residual material; in addition, it is generally possible to easily pass the endoscope through the lower esophageal sphincter (unlike in malignancy).
Thyroid
Major drug interactions
↓ Levothyroxine absorption
Bile acid binding agents (eg, cholestyramine) Iron, calcium, aluminum hydroxide Proton pump inhibitors, sucralfate
↑ TBG concentration
Estrogen (oral), tamoxifen, raloxifene Heroin, methadone
↓ TBG concentration
Androgens, glucocorticoids Anabolic steroids Slow-release nicotinic acid
↑ Thyroid hormone metabolism
Rifampin Phenytoin Carbamazepine
Amyloidosis
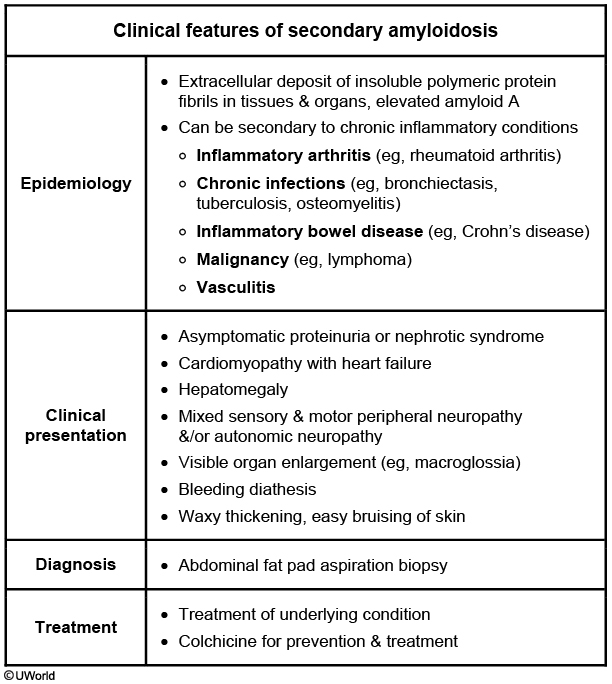
This patient's clinical presentation of facial swelling, bilateral lower-extremity edema, and massive proteinuria are consistent with nephrotic syndrome. The presence of nephrotic syndrome with palpable kidneys, hepatomegaly, and ventricular hypertrophy (suggested by an audible fourth heart sound) in the setting of chronic inflammatory disease (recurrent pulmonary infections, bronchiectasis) is suggestive of secondary amyloidosis (AA) as a common unifying diagnosis. Treatment is usually directed at the underlying inflammatory disease. Colchicine is approved for both the treatment and prophylaxis of AA.
RA complications
Increased levels of proinflammatory cytokines, corticosteroid therapy, and lack of physical activity may contribute to local (around inflamed joints) or generalized loss of bone mass in RA patients. There is an increased risk of osteopenia,osteoporosis, and bone fractures, especially if other risk factors (eg, low body weight, female sex, family history of osteoporosis, cigarette smoking, postmenopausal state, excessive alcohol use, other comorbidities) are present. The degree of bone loss generally correlates with disease activity. Strategies to prevent bone loss (adequate physical activity, optimization of vitamin D and calcium intake, minimization of glucocorticoid dose) should be implemented. Most experts suggest a low threshold for starting bisphosphonate therapy in RA patients.
Scrotal cancer
After the diagnosis of a solid testicular mass has been made, (a painless hard mass in testicle + suggestive ultrasound), the initial management is removal of the testis and its associated cord, orchiectomy. This is done through a small inguinal incision. The procedure is called high inguinal orchiectomy. The testis and abnormal tissue present is then examined under the microscope to determine the type of cancer. Depending on the cell type of the cancer present other therapies, i.e. additional surgery, radiation therapy, or possibly chemotherapy may be indicated.
Using a combination of these therapies, testicular cancer has one of the highest cure rates of all cancers. This has been achieved using a combination of surgery and chemotherapy, as well as radiation in certain instances. Cure from testicular cancer can even be achieved in individuals who have had the cancer spread into other parts of the body. This is the tumor that we kill first and investigate later. So observation, chemotherapy, and biopsies are not the next best step in this case.
FNAC, or transscrotal biopsy, is contraindicated because of the risk of spillage of cancer cells, which can potentially spread through lymphatics and blood vessels.
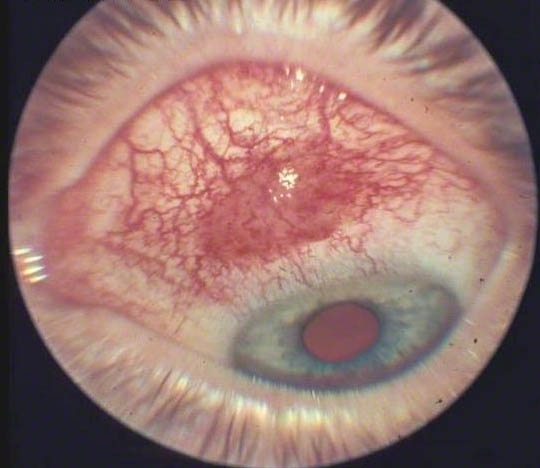
Central retinal vein occlusion
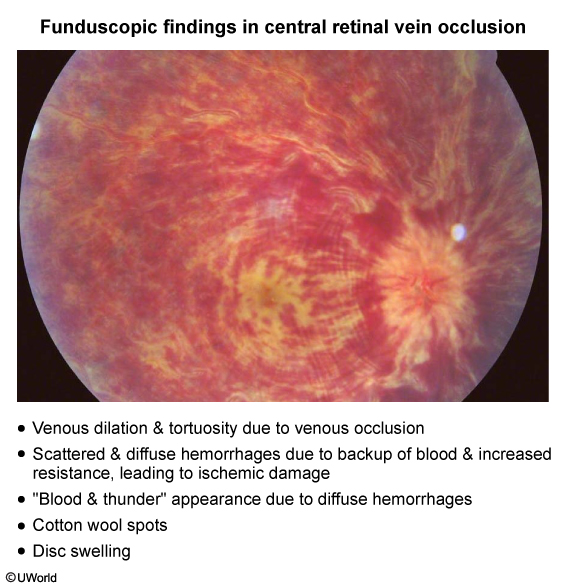
This patient with acute, unilateral, painless loss of vision has findings suggestive of central retinal vein occlusion (CRVO).
Diarrhea
Bacterial causes of diarrhea
Organism
Features
Bacillus cereus
Diarrhea, abdominal cramping Ingestion of preformed toxin in starchy foods such as rice
Staphylococcus aureus
Vomiting, abdominal pain Diarrhea not typical but may occur Caused by preformed toxin with rapid onset of symptoms
Clostridium difficile
Abdominal pain, watery diarrhea, possible fever Bloody stools unusual Associated with antibiotic exposure
Clostridium perfringens
Brief illness with watery diarrhea, cramps & fever Associated with undercooked or unrefrigerated food
Salmonella
Watery diarrhea, fever, abdominal pain & vomiting Associated with undercooked foods, especially poultry & eggs Antibiotic treatment needed only for severe disease or immunocompromised patients
Vibrio vulnificus
Vomiting, diarrhea & abdominal pain Associated with raw or undercooked shellfish May cause invasive, life-threatening disease in immunocompromised patients or those with liver disease
Escherichia coli
Watery diarrhea, may be bloody if associated with enterohemorrhagic (Shiga-toxin producing) strain Associated with undercooked beef or foods contaminated with bovine feces
Shigella
Bloody diarrhea with fever & often bacteremia Associated with contaminated food or water, especially during travel outside the United States
Campylobacter species
Abdominal pain, bloody diarrhea Highest incidence in children & young adults Associated with raw or undercooked meats
This patient has acute onset of bloody diarrhea associated with abdominal pain. In the absence of travel history, the differential diagnosis for this acute illness is relatively limited. Bloody diarrhea is most often caused by bacterial pathogens, specifically Escherichia coli, Shigella, and Campylobacter. The most common cause of bloody diarrhea in the absence of fever is E coli
The enterohemorrhagic E coli (EHEC) strain produces Shiga toxin, which causes an inflammatory diarrhea syndrome with bloody stools and abdominal pain. EHEC infection is most frequently associated with consumption of contaminated beef products, although there have been documented outbreaks associated with other foods such as fruits, leafy vegetables, and milk products. Isolated cases without a clear source are also common. The diagnosis can be confirmed with assay for Shiga toxin in stool. Stool culture can also identify toxin-producing strains. Treatment is generally supportive; antibiotics are not helpful and may increase the risk of hemolytic uremic syndrome.
Ehrlichosis
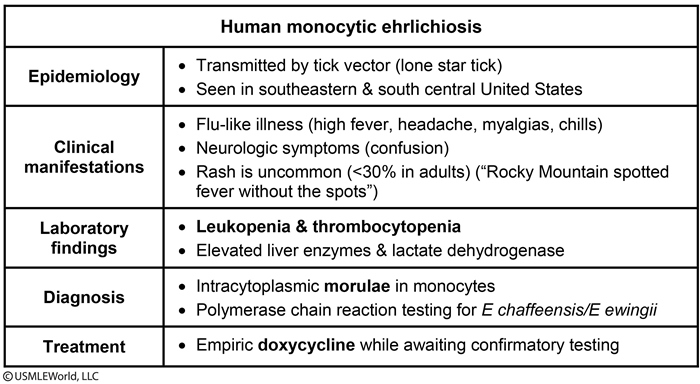
This vignette depicts a patient with a typical case of ehrlichiosis. Ehrlichiosis is a tick-borne infection caused by Ehrlichia chaffeensis and E ewingii. These bacteria are carried by ticks, including the lone star tick (Amblyomma americanum), found in the southeastern and south central United States. The principal reservoir is the white tail deer.
Ehrlichiosis is characterized by an acute febrile illness with malaise and altered mental status. Ehrlichiosis is not often associated with a rash (<30% in adults) and is described as "Rocky Mountain spotted fever (RMSF) without the spots." Neurologic symptoms may include confusion, mental status changes, clonus, and neck stiffness. Laboratory studies often show leukopenia and/or thrombocytopenia, along with elevated aminotransferases and lactate dehydrogenase.
The diagnosis is often clinical, although definitive diagnosis can be made through visualization of intracytoplasmic morulae in white blood cells or through polymerase chain reaction testing. Doxycycline is the appropriate treatment and is often initiated empirically when the diagnosis is suspected while confirmatory testing is pending.
Hirsutism
Although most women with hirsutism (excess terminal hair growth) have polycystic ovary syndrome (PCOS), rapid-onset hirsutism, with or without virilization (eg, vocal deepening, excessive muscular development, clitoromegaly), suggests very high androgen levels due to an androgen-secreting neoplasm of the ovaries or adrenal glands.
The primary ovarian androgens include testosterone, androstenedione, and dehydroepiandrosterone. The adrenals produce these as well as dehydroepiandrosterone-sulfate (DHEAS). Therefore, women with a suspected androgen-producing tumor should be evaluated with serum testosterone and DHEAS levels:
Elevated testosterone levels with normal DHEAS levels suggest an ovarian source (more common).
Elevated DHEAS levels suggest an adrenal tumor (far less common).
DHEAS and DHEA have negligible intrinsic androgenic action but are converted to androstenedione and subsequently to testosterone in peripheral tissues. Some adrenal tumors can also directly produce testosterone.
Bilirubin
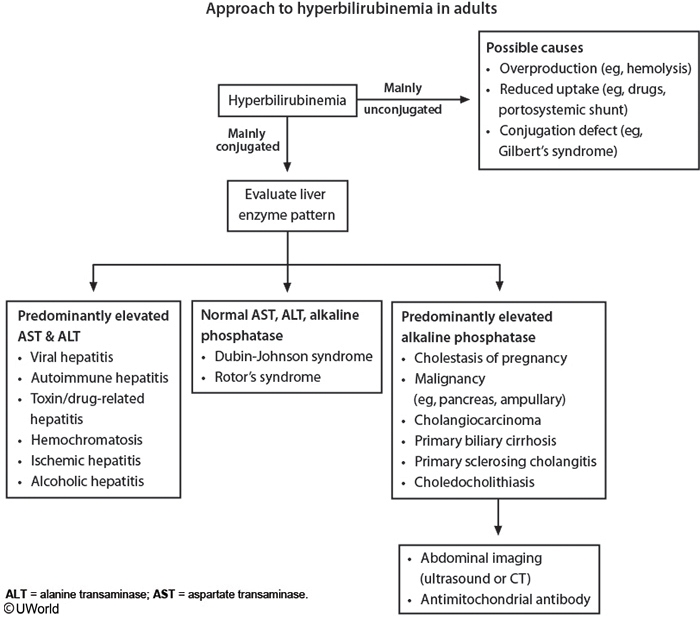
An understanding of the bilirubin metabolism pathway clarifies how a positive urine bilirubin assay reflects a buildup of conjugated bilirubin. Following hemoglobin breakdown, the majority (95%) of bilirubin is in the unconjugated form, which undergoes hepatic conjugation. Conjugated bilirubin then goes into the intestines, where it is predominantly deconjugated and recycled (enterohepatic circulation) to be reconjugated in the liver. Alternatively, some of its metabolism products are excreted in feces as urobilinogen, with ~1% of urobilinogen being renally excreted.
Unconjugated bilirubin (tightly bound to albumin) is highly insoluble, so it cannot be excreted in urine. Excess unconjugated bilirubin (eg, hemolysis) undergoes the regular conjugation pathway with eventual production of urobilinogen, and the resultant excess urobilinogen is primarily recycled; however, a higher than normal amount of urobilinogen is excreted in feces or urine, leading to a positive urine urobilinogen assay (not seen in this patient). On the other hand, conjugated bilirubin (loosely bound to albumin) is water soluble, so it can be excreted in urine. Despite this, no bilirubin is normally seen on urinalysis (negative urine bilirubin assay) because conjugated bilirubin is usually degraded in the intestines. However, when there is hepatic dysfunction, biliary obstruction, or a defect in hepatic bilirubin secretion (as in this patient), there is plasma buildup of conjugated bilirubin, which leaks into urine. This results in dark urine and a positive urine bilirubinassay.
Hepatic Adenoma
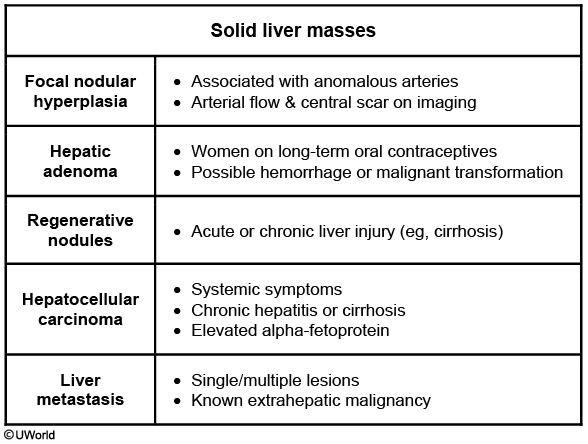
This young woman has a large, painful hepatic mass. She has elevated alkaline phosphatase and gamma glutamyl transpeptidase (GGT) levels, suggesting biliary compression or obstruction, but otherwise relatively normal liver markers. In light of her minimal alcohol consumption and long-term use of oral contraceptives, this likely represents a hepatic adenoma. Hepatic adenomas are benign epithelial tumors that are most common in young and middle-age women. Additional risk factors include anabolic androgen use and pregnancy.
Initial diagnosis is based on the clinical presentation and imaging studies. Ultrasound most commonly shows well-demarcated, hyperechoic lesions, and contrast-enhanced CT can show early peripheral enhancement. Needle biopsy is not recommended for suspected hepatic adenoma due to the risk of bleeding, and surgical excision is preferred. Possible long-term complications include progressive growth, rupture, and malignant transformation.
Hepatic adenoma can clinically resemble focal nodular hyperplasia (FNH), a common mass lesion in young women caused by hyperperfusion from anomalous arteries. However, FNH is not associated with oral contraceptives, and imaging will show evidence of increased arterial flow and sometimes a central scar.
Last updated