Psychotic Disorders
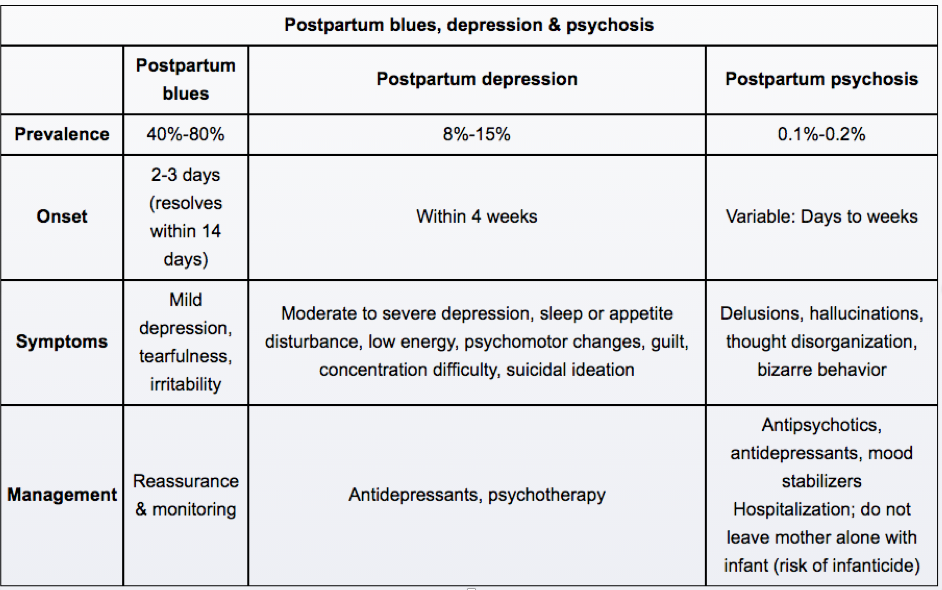
Postpartum
Schizophrenia
Overview
Schizophrenia is a disorder of thought process, characterized by both "positive" and "negative" symptoms characteristic of psychosis. It can be diagnosed after >6 months of symptoms.
Positive symptoms include hallucinations, delusions, bizarre behavior, and disorganization
Negative symptoms include social withdrawal, blunted affect, anhedonia, apathy, and alogia
Diagnosis
Diagnosis of schizophrenia requires at least 2 of the following, which must be present for most of a 1-month "active" period within the diagnostic 6 month timeframe. At least one of these must be 1-3:
Delusions
Hallucinations (esp. auditory)
Disorganized speech (e.g. loose associations)
Disorganized or catatonic behavior
Negative symptoms
Social or occupational dysfunction is also necessary for diagnosis, and is a prominent feature in schizophrenia.
Note: Schizophrenia subtypes have been removed from the DSM-5.
Imaging
Neuroimaging classically reveals enlarged cerebral ventricles secondary to decreased hippocampus (decreased GABA), amygdala volume.,
Demographics
More common in people born during months of cold weather (Northern hemisphere: January-April; Southern hemisphere: July-September).,
Treatment
In addition to treatment with an antipsychotic agent, family psychoeducational intervention is recommended for patients and family members following an acute psychotic episode.
Family psychoeducational intervention reduces the level of stress between the patient and their environment (i.e. family members), thereby reducing the frequency of psychotic relapse.
vs bipolar
The manic phase of bipolar disorder may resemble schizophrenia. It is characterized by an elated mood, rapid onset, hyperactivity, rapid speech. It can sometimes include psychotic symptoms, but usually there is little or no social or occupational impairment between episodes and possible psychotic symptoms are not bizarre (i.e. “I’m friends with the president” instead of “I’m the leader of the dolphins”).
Schizoid
Schizoid personality disorder is characterized by social withdrawal without psychosis. These people often have very few friends and they are content with this.
Schizotypal
Schizotypal personality disorder is characterized by bizarre behavior and odd thought patterns without psychosis. Thoughts are usually magical.
Delirium
Delirium may resemble schizophrenia. Patients exhibit clouding of consciousness, visual hallucinations, and illusions. This state is secondary to an organic medical cause (e.g. sepsis, CNS injury, thyrotoxicosis), which must be searched for and treated.
An EEG can be of use in differentiating between psychosis and delirium. The EEG is normal in psychosis, but abnormal in delirium.
Brief psychotic disorder and schizophreniform
Brief psychotic disorder is characterized by the sudden onset of psychotic symptoms lasting ≥1 day and ≤1 month. It is a rare disorder that requires ruling out psychotic disorders as a result of substance use or medical conditions. No negative symptoms.
Schizophreniform disorder is an episode of psychosis lasting less than 6 months but greater than 1 month:
Brief psychotic disorder < 1 month < Schizopheniform disorder < 6 months
It can be considered an “upgrade” from brief psychotic disorder after 1 month has passed
All 5 criteria of schizophrenia
Acute Psychosis

Initial treatment with an oral antipsychotic medication is appropriate. Second-generation antipsychotics, such as quetiapine, are often chosen due to their lower risk of extrapyramidal side effects and tardive dyskinesia compared with first-generation antipsychotics. With the exception of clozapine, there is no evidence that one antipsychotic is more effective than another.
Schizoaffective
Schizoaffective disorder is a disorder characterized by psychosis associated with a mood disorder, such as mania or depression.

Delusional
Delusional disorder can appear similar to schizophrenic delusions. It is characterized by a fixed, non-bizarre delusional system and few if any other thought disorders. An important difference for diagnosis is that individuals with delusional disorder have relatively normal social and occupational functioning.
Key in distinguishing it from schizophrenia, delusions in delusional disorder are classically not bizarre (i.e. not on the USMLE). Non-bizarre delusions involve beliefs that are within the realm of reality; they could actually occur in a person's life. Patients with delusional disorder may persistently believe that someone is in love with them, or that someone is conspiring against them.
Additionally, delusional disorder often presents later in adulthood (some sources report a mean age of 40 years), as opposed to the late adolescent presentation of schizophrenia.
Delusional disorder occurs when a patient experiences non-bizarre, fixed delusions that continue for >1 month. Descriptions of selected types of delusions are given below:
Grandiose type: The central theme is that of the patient's purported grand discovery, idea, or talent.
Erotomanic type: The central theme is that of another individual being in love with the patient.
Jealous type: The central theme is that the patient's love interest is unfaithful.
Persecutory type: The central theme is that the patient is being conspired against, cheated, spied on, etc.
Somatic type: The central theme involves bodily feelings or functions.
In order to diagnose delusional disorder, the following pathologies must be ruled out:
Schizophrenia or other psychotic disorders
Substance abuse
Dementia and delirium
Mania, hypomania, or a bipolar disorder

Treatment
The first-line treatment of delusional disorder is with antipsychotic agents (e.g. aripiprazole or ziprasidone).
Delusional disorder is no longer separated from shared delusional disorder or folie a deux (formerly the descriptor for shared delusional beliefs among two people who share a close relationship). If delusional disorder criteria are met, then that is the diagnosis.
Last updated