Uworld 2
Variable Decel
maternal repositioning
amnionic fluid infusion
CVID
Common variable immunodeficiency
Manifestations
Recurrent respiratory (eg, pneumonia, sinusitis, otitis) & GI (eg, Salmonella, Campylobacter) infections Autoimmune disease (eg, RA, thyroid disease) Chronic lung disease (eg, bronchiectasis) GI disorders (eg, chronic diarrhea, IBD-like conditions)
Diagnosis
↓↓ IgG, ↓ IgA/IgM No response to vaccination
Management
Immunoglobulin replacement therapy
GI = gastrointestinal; IBD = inflammatory bowel disease; RA = rheumatoid arthritis.
This girl has had episodes of sinusitis, streptococcal bacteremia, and Giardia lambliainfection, as well as failure to thrive and a history of asthma. Her presentation is most suggestive of common variable immunodeficiency (CVID). In CVID, abnormal B-cell differentiation results in deficiency of multiple immunoglobulin classes (IgG and either IgA, IgM, or both). Affected patients are at risk for recurrent respiratory infections, frequently from encapsulated organisms such as Streptococcus pneumoniae and Haemophilus influenzae. Many patients have Giardia lamblia infection. In some cases in which T-cell immunity is also affected, patients are also at increased risk for enteroviral encephalitis. Failure to thrive and chronic respiratory problems (eg, asthma, bronchiectasis) are common. CVID can present in childhood (around puberty) or, more commonly, in adulthood (age 20-40).
Management of CVID is focused on avoiding infection, so the mainstay of treatment is intravenous immunoglobulin infusion. Early initiation of therapy may prevent some complications of chronic infection. Patients with CVID have increased risk of autoimmune disease and certain malignancies regardless of treatment.
SBP
Spontaneous bacterial peritonitis
Clinical presentation
Temperature >37.8 C (100 F) Abdominal pain/tenderness Altered mental status (abnormal connect-the-numbers test) Hypotension, hypothermia, paralytic ileus with severe infection
Diagnosis from ascitic fluid
PMNs >250/mm3 Positive culture, often gram-negative organisms (eg, Escherichia coli, Klebsiella) Protein less than 1 g/dL SAAG >1.1 g/dL
Treatment
Empiric antibiotics - third-generation cephalosporins (eg, cefotaxime) Fluoroquinolones for SBP prophylaxis
PMN = polymorphonuclear leukocytes; SAAG = serum-ascites albumin gradient; SBP = spontaneous bacterial peritonitis.
This patient has cirrhosis and ascites accompanied by fever and lethargy, a presentation concerning for spontaneous bacterial peritonitis (SBP) and hepatic encephalopathy. The asterixis (flapping hand tremor), ascites, and laboratory abnormalities are all manifestations of his underlying cirrhosis. SBP superimposed on cirrhosis can be a subtle presentation, requiring a low threshold of suspicion. Fever and subtle changes in mental status are the most common symptoms, while abdominal pain often less prominent than in peritonitis due to other causes.
For making the diagnosis, paracentesis is the test of choice with the main diagnostic criteria being a positive ascites fluid culture and neutrophil count of >250/mm3. Paracentesis should be done before antibiotic therapy is initiated as therapy often results in negative ascites cultures. Enteric organisms such as Escherichia coli and Klebsiella are the most commonly cultured organisms followed by the streptococcal species; empiric therapy usually includes a third-generation cephalosporin.
Scarlet Fever
Scarlet fever
Etiology
Streptococcus pyogenes
Clinical features
Fever & pharyngitis Tonsillar erythema & exudates Strawberry tongue Tender anterior cervical nodes Sandpaper rash
Diagnosis
Rapid streptococcal antigen test Throat culture
Treatment
Penicillin (eg, amoxicillin)
Scarlet fever is an illness caused by group A Streptococcus that develops most commonly in children who have streptococcal pharyngitis. Certain strains of Streptococcus pyogenes produce erythrogenic exotoxins, which are responsible for the characteristic rash of scarlet fever.
Fever, sore throat, and headache typically precede the rash, which usually spreads across the trunk, groin, and axillae. The exanthem has a characteristic, finely papular, "sandpaper" texture and is most pronounced in the skin folds. As the illness resolves, desquamation of the rash results in peeling of the hands and feet.
An erythematous pharynx with tonsillar exudates, palatal petechiae, and a strawberry tongue are classic findings on examination. The area around the mouth may appear pale in comparison with the red cheeks, giving the appearance of circumoral pallor. Tender, shotty, anterior cervical lymphadenopathy, as seen in this patient, is another nonspecific finding.
Scarlet fever is managed the same as streptococcal pharyngitis. Diagnosis is confirmed by rapid streptococcal antigen test or throat culture, and treatment is with penicillin. No additional therapy is required for the rash.
Diagnosis of Kawasaki disease (KD) requires 5 days of fever and ≥4 clinical criteria: >1.5 cm cervical node, polymorphous rash, edema of the hands/feet, conjunctivitis, and mucosal changes (eg, strawberry tongue, dry/cracked lips). KD is unlikely in this patient with only 2 days of fever and 2 of the listed criteria.

Ureteral colic
ureteral colic ileus
This ileus is possibly due to a vagal reaction caused by ureteral colic. Needle-shaped crystals on urinalysis indicate uric acid stones. Uric acid stones, which are radiolucent, have to be evaluated by CT of the abdomen or intravenous pyelography. Abdominal ultrasonography may also detect radiolucent stones. CT is also useful for diagnosing other pathology, such as appendicular abscess or bowel obstruction, especially in this patient with ileus. Ileus will resolve when the ureterolithiasis is treated. Stones <1 cm may pass spontaneously with hydration and analgesia; otherwise, surgical intervention is needed.
Varenicline
Varenicline, an alpha-4 beta-2 nicotinic acetylcholine receptor partial agonist, can diminish nicotine cravings. Despite earlier concerns, varenicline does not appear to increase the risk of suicidality or depression compared with placebo. It has been associated with an increased risk of cardiovascular events in patients with preexisting cardiovascular disease.
ARDS
Most patients with ARDS require mechanical ventilation with the following goals:
Avoiding complications of mechanical ventilation by using lung-protective strategies such as low tidal volume ventilation (LTVV): LTVV (6 mL/kg of ideal body weight) decreases the likelihood of overdistending alveoli and provoking barotrauma due to high plateau pressures (pressure applied to small airways and alveoli). LTVV improves mortality in patients with ARDS. In contrast, higher tidal volumes in ARDS may result in elevated pulmonary pressures due to the work of forcing larger volumes into stiff lungs (decreased compliance), leading to increased alveolar distension.
Providing adequate oxygenation: Increasing the fraction of inspired oxygen (FiO2) administered by the ventilator improves oxygenation; however, prolonged FiO2 levels >0.6 are associated with oxygen toxicity. Increasing positive end-expiratory pressure (PEEP) also improves oxygenation by preventing alveolar collapse at the end of expiration, thereby decreasing shunting and the work of breathing. Given the severe hypoxemia seen in ARDS, PEEP levels up to 15-20 cm H2O may be necessary to maintain oxygenation. The goal is arterial partial pressure of oxygen (PaO2) at 55-80 mm Hg or peripheral saturation (SpO2) at 88%-95% (ie, preventing SpO2 <88%, not <92%) (Choices A and E).
New lung nodule

The size of an SPN strongly correlates with the chances of it being malignant. Nodules 0.8 cm require additional management or surveillance**.
In addition to size, other factors that influence the probability of an SPN being malignant include patient age, sex, smoking history, family history, location of the nodule in the lung, and radiographic appearance of the nodule (eg, regular versus irregular borders). Nodules >0.8 cm that are intermediate or high probability for malignancy (ie, ≥5% risk) based on these factors require tissue diagnosis with biopsy or surgical excision.
For patients in whom the need for tissue diagnosis is unclear, positron emission tomography (PET) scan can be helpful. Nodules demonstrating high metabolic activity on PET scan are more likely malignant than benign and warrant biopsy or surgical excision.
Sclerosis
Systemic sclerosis subtype characteristics
Limited cutaneous
Diffuse cutaneous
Scleroderma on head & distal UE Prominent vascular manifestations Raynaud phenomenon Cutaneous telangiectasia Pulmonary arterial hypertension CREST syndrome Anticentromere antibodies Better prognosis
Scleroderma on trunk & UE Prominent internal organ involvement Scleroderma renal crisis Myocardial ischemia & fibrosis Interstitial lung disease Anti-Scl-70 (topoisomerase-1) antibodies Anti-RNA polymerase III antibodies Worse prognosis
UE = upper extremities.
PHTN
Clinical features of pulmonary hypertension
Classification
Pulmonary arterial hypertension (WHO group 1) Due to left-sided heart disease (group 2) Due to chronic lung disease (eg, COPD, ILD) (group 3) Due to chronic thromboembolic disease (group 4) Due to other causes (eg, sarcoidosis) (group 5)
Symptoms
Dyspnea, fatigue/weakness Exertional angina, syncope Abdominal distension/pain
Signs
Left parasternal lift, right ventricular heave Loud P2, right-sided S3 Pansystolic murmur of tricuspid regurgitation JVD, ascites, peripheral edema, hepatomegaly
Brain Abscess

Invasive aspergillosis
CT scan of the chest usually reveals nodules with surrounding ground-glass opacities ("halo sign").,
Cholesteatoma
Cholesteatomas in children can either be congenital or acquired, with congenital lesions typically found in younger patients around the age of five. Acquired cholesteatomas usually occur secondary to chronic middle ear disease. The diagnosis should be suspected in any patient with continued ear drainage for several weeks despite appropriate antibiotic therapy. Chronic middle ear disease leads to the formation of a retraction pocket in the tympanic membrane, which can fill with granulation tissue and skin debris, as seen in this patient. Complications of cholesteatomas include hearing loss (which this patient appears to already be experiencing), cranial nerve palsies, vertigo, and potentially life-threatening infections such as brain abscesses or meningitis. This patient should be referred to an otolaryngologist for a dedicated otologic exam, possibly accompanied by a CT and/or surgical visualization to confirm the diagnosis.
An osteoma is a benign, solitary area of bony overgrowth that can form in the outer ear and lead to hearing loss.
Ventricular Aneurysm
Usually, ST-segment elevations resolve within a few weeks of an MI. VAs present with ECG findings of persistent ST-segment elevation after a recent MI and deep Q waves in the same leads. Large VAs can lead to progressive left ventricle (LV) enlargement, causing heart failure, refractory angina, ventricular arrhythmias, mural thrombus with systemic arterial embolization, or mitral annular dilation with mitral regurgitation (MR) (explaining this patient's murmur). Diagnosis is confirmed by echocardiography (thinned, dyskinetic LV portion in the area of prior MI).
Boeerhave

Disseminated gonococcal

This patient has the classic triad of polyarthralgia, tenosynovitis, and painless vesiculopustular skin lesions for disseminated gonococcal infection. Her complaints of wrist, elbow and ankle pain are consistent with gonococcal polyarthralgias, and her pain elicited along the tendon sheaths suggests tenosynovitis. The lesions shown in the photograph are typical vesiculopustular lesions of disseminated gonococcal infection; they tend to number from two to ten and may be dismissed as furuncles or pimples. Fevers and chills may be present. A history of recent unprotected sex with a new partner is frequently associated with disseminated gonococcal infection, while symptoms of symptomatic venereal disease are most often absent.
Metatarsus adductus



Congenital clubfoot can be distinguished from MA by rigid medial and upward deviation of both forefoot and hindfoot.
Reactive Attachment Disorder
This child's history of neglect, social withdrawal, lack of positive response to attempts to comfort, and decreased emotional responsiveness is consistent with reactive attachment disorder (RAD). RAD may develop in young children when abuse, neglect, prolonged institutionalization, or inconsistent care (eg, frequently moving between foster homes) disrupts the development of a healthy, secure attachment to caregivers. These children seldom seek comfort and do not respond to attempts to comfort them. Other symptoms include lack of social responsiveness, lack of positive emotions, and episodes of unexpected irritability or sadness in response to nonthreatening encounters.
Another possible outcome of early neglect is disinhibited social engagement disorder, which is characterized by overfamiliarity and an unhesitant approach to unfamiliar adults (Choice D). Other disturbances commonly seen in children with a history of abuse or neglect include poor emotion regulation, toileting and sleep difficulties, anxiety, aggression, hyperactivity and/or impulsivity.
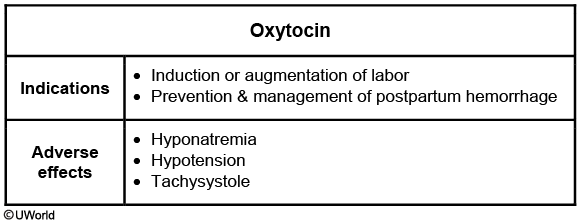
Oxytocin
Whipple
Whipple's disease is a rare multi-systemic illness. It is an infectious disease caused by the bacillus Tropheryma whippelii. It is most commonly seen in white men in the fourth-to-sixth decades of life, and often presents with weight loss. Gastrointestinal symptoms include abdominal pain, diarrhea, and malabsorption with distension, flatulence, and steatorrhea. Extraintestinal manifestations include migratory polyarthropathy, chronic cough, and myocardial or valvular involvement leading to congestive failure or valvular regurgitation. Later stages of the disease may be characterized by dementia and other central nervous system findings, such as supranuclear ophthalmoplegia and myoclonus. Intermittent low-grade fever, pigmentation and lymphadenopathy may also be occasionally seen. PAS-positive material in the lamina propria of the small intestine is a classical biopsy finding.
Schizophrenia
These symptoms include the presence of ≥2 of the following: Delusions, hallucinations, disorganized speech (eg, frequent derailment, incoherence), grossly disorganized or catatonic behavior, and negative symptoms (eg, flat affect, social withdrawal).
Lesch Nyhan
Lesch-Nyhan syndrome
Pathophysiology
X-linked recessive Deficiency of hypoxanthine-guanine phosphoribosyltransferase Hypoxanthine & uric acid accumulation
Clinical features
Delayed milestones & hypotonia in infancy Early childhoodIntellectual disability Extrapyramidal symptoms (eg, dystonia, chorea) Pyramidal symptoms (eg, spasticity, hyperreflexia) Self-mutilation Gouty arthritis in late, untreated disease
Lesch-Nyhan syndrome is an X-linked recessive disorder caused by a deficiencyof hypoxanthine-guanine phosphoribosyltransferase, an enzyme involved in purine metabolism. This deficiency results in the accumulation of hypoxanthine and uric acid in the urine, serum, and central nervous system. The development of dopaminergic pathways appears to be particularly affected, which may explain the progressive neuropsychiatric manifestations of the condition.
Presentation begins in early infancy with delayed milestones and hypotonia. By age 3, children develop the extrapyramidal symptoms of dystonia and chorea as well as the pyramidal symptoms of spasticity and hyperreflexia. A distinct finding in Lesch-Nyhan syndrome is self-mutilation (eg, biting of the fingers and hands, banging of the head and limbs), as shown in this child. In untreated, late disease, excessive uric acid can lead to gouty arthritis and obstructive nephropathy.
Iron Poisoning
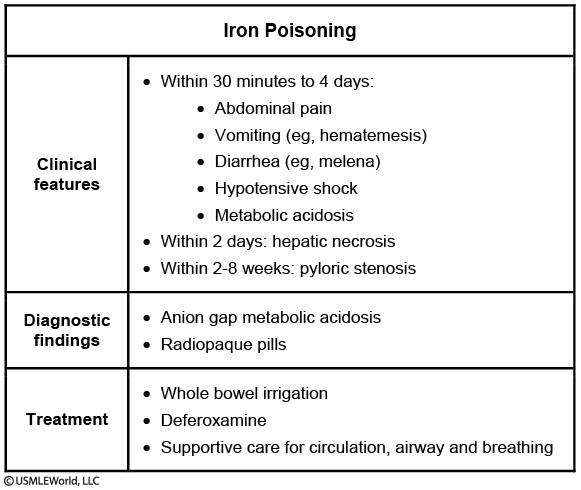
This patient's symptoms and x-ray findings are highly suggestive of iron poisoning, one of the most common causes of death by poisoning. When ingested in large amounts, elemental iron is corrosive to the gastrointestinal mucosa, causing abdominal pain, nausea, vomiting, diarrhea, and hematemesis within 30 minutes to 6 hours of ingestion. Iron is also a potent vasodilator and toxic to cellular processes. Severely affected patients develop hypotensive shock and anion-gap metabolic acidosis from poor perfusion and accumulation of lactic acid. These patients may become tachypneic and develop respiratory alkalosis to compensate for the acidosis. Other dangerous complications include liver necrosis, coagulopathy, seizures, and death. Patients who survive acute toxicity are at risk of gastric scarring and pyloric stenosis within weeks of ingestion.
The diagnosis is confirmed by measuring serum iron levels. Iron is radiopaque, and visualization of gastric tablets on abdominal x-ray further supports the diagnosis. Treatment depends on the severity of the poisoning. Whole-bowel irrigation is sometimes instituted, but other methods of decontamination (eg, activated charcoal, syrup of ipecac, gastric lavage) are not routinely recommended. Chelation therapy with intravenous deferoxamine is used in moderate-to-severe cases and would be indicated in this patient.
Acute Mediastinitis
acute mediastinitis, surgical debride and abx
Photosensitivity

Brain Death
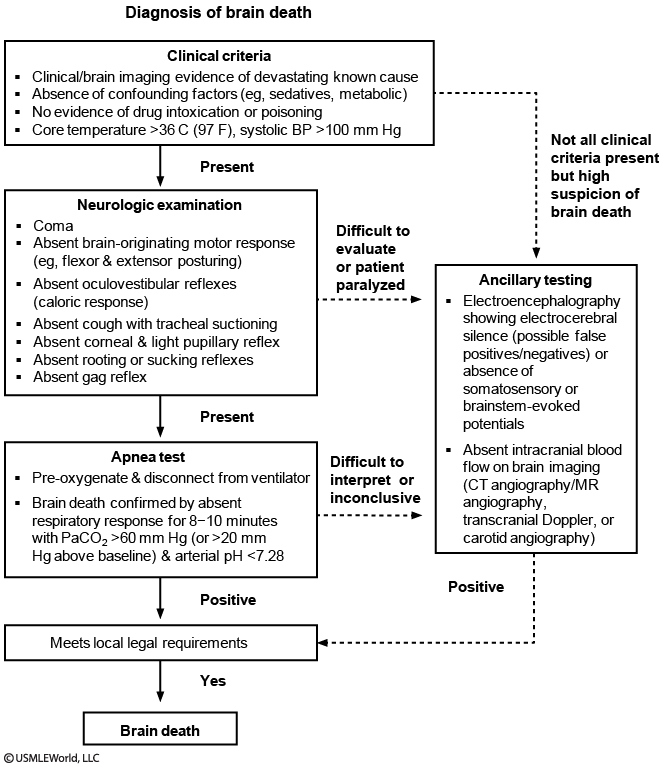
Brain death is a legally acceptable definition of death, and artificial life support does not need to be continued. In this patient's case, no further steps are legally required to remove him from the ventilator. Copyright (c) UWorld, Please do not save, print, cut, copy or paste anything while a test is active.
Acetaminophen toxicity
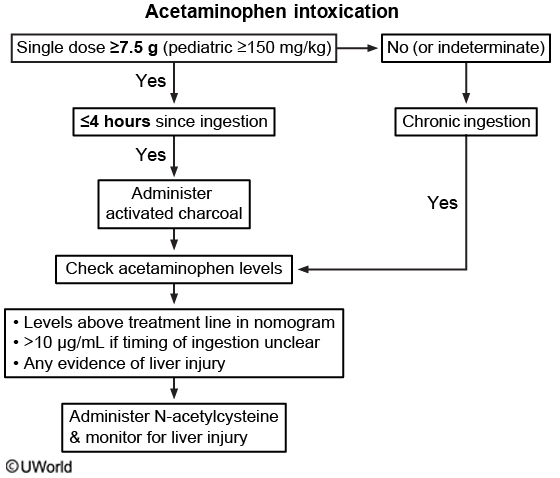
This patient was brought to the emergency department 2 hours after ingesting a potentially toxic dose (single dose of >7.5 g) of acetaminophen. Patients at this early stage of acetaminophen intoxication can be asymptomatic (first 24 hours) or may have only nonspecific symptoms such as nausea, vomiting, and anorexia. After 24 hours, patients may develop severe liver injury.
The initial management should be focused on gastric decontamination with activated charcoal if the patient presents within 4 hours of ingestion. Acetaminophen levels should be obtained at the same time. The Rumack-Matthew nomogram provides the likelihood of hepatotoxic effects of acetaminophen overdose after a single ingestion based on plasma acetaminophen level and hours since ingestion. This tool is also used in guiding the administration of N-acetylcysteine in patients with dangerous acetaminophen levels. The first data point begins at 4 hours. However, patients with an overdose often report incorrect times and doses; although an acetaminophen level may not be predictive of hepatotoxicity at this stage, it is prudent to obtain one. If the level is not within the toxic range by the nomogram, it should be repeated in 2 hours based on the patient’s history of ingestion.
Thalassemia
beta: A2 on gel electrophoresis
Sturge Weber
Sturge-Weber syndrome
Pathophysiology
Mutation in GNAQ gene
Clinical features
Port wine stain (trigeminal nerve [CN V1/V2] distribution) Leptomeningeal capillary-venous malformation Seizures ± hemiparesisIntellectual disability Visual field defects Glaucoma
Diagnosis
MRI of the brain with contrast
Management
Laser therapy Antiepileptic drugs Intraocular pressure reduction
This patient has had a new-onset seizure with a facial port wine stain and neurologic deficits, findings concerning for Sturge-Weber syndrome (SWS). SWS is a neurocutaneous disorder characterized by a capillary malformation (nevus flammeus, also known as port wine stain) in the distribution of the first or second branches of the trigeminal nerve with an associated leptomeningeal capillary-venous malformation affecting the brain and eye.
Patients with SWS have variable intellectual disability, which may present as developmental delays in infancy and early childhood. Seizures begin in early childhood and often originate focally with subsequent generalization, as seen in this patient. Hemiparesis contralateral to the intracranial malformation may present at the time of seizure onset. Glaucoma is the most common intraocular abnormality, and involvement of the occipital lobe or optic tract can cause visual field defects. For example, homonymous hemianopia, a defect in the right or left visual field of both eyes, results from a lesion involving the contralateral visual pathway.
MRI of the brain with contrast detects the intracranial vascular malformation and is diagnostic. Treatment is aimed at controlling seizures and reducing intraocular pressure. Laser therapy is also helpful in reducing the appearance of the port wine stain.
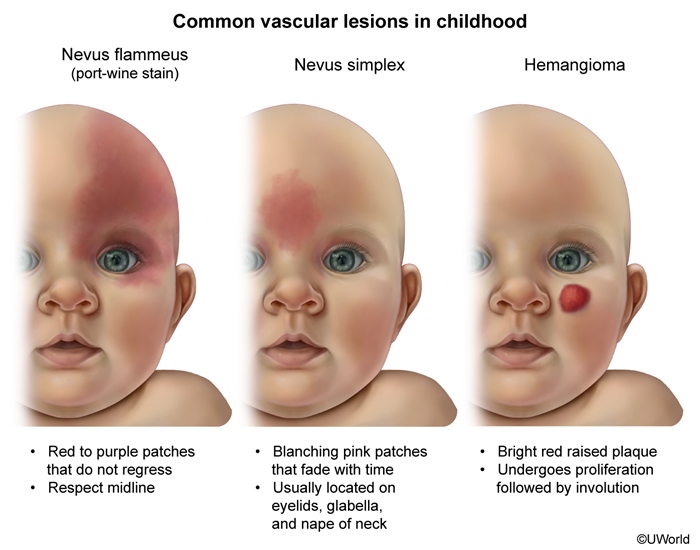

Infantile Hemangioma

Infantile hemangioma is a raised, vascular lesion composed of small capillaries and presents at birth or shortly after with a bright red papule/nodule. Hemangiomas initially proliferate in infancy before spontaneous involution. Seizures and neurologic deficits are not associated with hemangiomas.
NF1


Neurofibromatosis type 1 is an autosomal dominant neurocutaneous disorder that can cause intellectual disability and seizures. Patients typically have neurofibromas, axillary freckling, and café-au-lait macules but do not present with capillary malformations.
TS
Tuberous sclerosis is a neurocutaneous disorder that often presents with seizures and intellectual disability. Ocular abnormalities include retinal hamartomas, and typical skin findings are hypopigmented ash-leaf spots, angiofibromas (malar erythematous papules), and shagreen patches (flesh-colored plaque on the back).
Tuberous sclerosis is a neurocutaneous genetic (TSC1 and TSC2genes) syndrome associated with intracranial tumors (eg, cortical tubers or hamartomas, subependymal giant cell astrocytomas, subependymal nodules). Additional characteristics include hypopigmented macules ("ash leaf spots"), facial angiofibromas, cardiac rhabdomyomas, renal angioleiomyomas, mental retardation, and seizures.

COPD
Oxygen (target SpO2 of 88%-92%)
Inhaled bronchodilators
Systemic glucocorticoids
Antibiotics if ≥2 cardinal symptoms
Oseltamivir if evidence of influenza
NPPV if ventilatory failure
Tracheal intubation if NPPV failed or contraindicated
Breastfeeding CI

Skin

An acrochordon (skin tag) is a flesh-colored papule usually seen in regions of the body subjected to friction, such as the neck, axillae, and inner thighs.
Hemoptysis

Cerebral Amyloid Angiopathy

Cerebral amyloid angiopathy is the second most common cause of intracerebral hemorrhage after hypertension and is typically lobar in location. It most often occurs in patients age >75 and is due to abnormal beta-pleated amyloid protein deposition in cerebral blood vessels, leading to arteriopathy and vessel fragility.
Ludwig angina
ludwig angina
Ludwig angina is a rapidly progressive cellulitis of the submandibular space. Most cases arise from dental infections in the mandibular molars that spread contiguously down the root into the submylohyoid (and then sublingual) space. The infection is usually polymicrobial with a mixture of oral aerobic (eg, viridans streptococci) and anaerobic bacteria.
Patients develop symptoms rapidly with systemic (fever, chills, malaise) and local compressive (eg, mouth pain, drooling, dysphagia, muffled voice, airway compromise) manifestations. Physical examination findings are often striking due to mass effect from edema. The submandibular area is usually tender and indurated, and the floor of the mouth is often elevated, displacing the tongue. Anaerobic, gas-producing bacteria may cause crepitus.
CT scan of the neck confirms the diagnosis and rules out an abscess. Most patients are treated with intravenous antibiotics (eg, ampicillin-sulbactam, clindamycin) and removal of the inciting tooth. Drainage and surgery are rarely required as the process is cellulitic and typically nonsuppurative. Impaired respiratory status requires prompt attention and early intervention with a mechanical airway.
Transfusions
packed RBC: stable patients with low Hgb
whole RBC: unstable patients need volume expansion
FFP: has clotting factors and plasma proteins. Coagulation problems (liver cirrhosis, DIC)
platelet: <10k or <50k with bleed
Tourette
Pharmacotherapy can also be considered when HRT is ineffective or when symptoms interfere with social, academic, or occupational functioning. Alpha-2 adrenergic receptor agonists (eg, clonidine, guanfacine) have been used in mild cases. Dopamine-blocking agents (tetrabenazine) are the most effective treatment and should be considered in more severe cases. The first-generation antipsychotics haloperidol and pimozide are the only FDA-approved medications for Tourette disorder. However, due to side effects of high-potency antipsychotics (muscle stiffness, dystonias, parkinsonism) and prolongation of the QTc interval associated with pimozide, second-generation antipsychotics are increasingly being used. Among these, risperidone is the best studied.
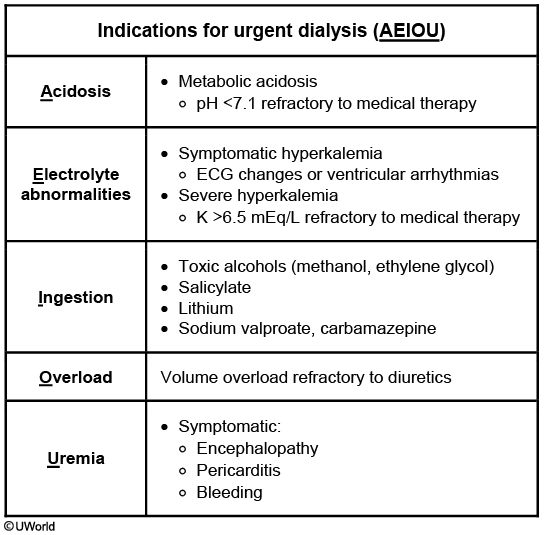
Dialysis
Lung

Ascitic Fluid
Ascites fluid characteristics
Color
Bloody: Trauma, malignancy, TB (rarely) Milky: Chylous, pancreatic Turbid: Possible infection Straw color: Likely more benign causes
Neutrophils
<250/mm3: No peritonitis ≥250/mm3: Peritonitis (secondary or spontaneous bacterial)
Total protein
≥2.5 g/dL (high-protein ascites) CHF, constrictive pericarditis, peritoneal carcinomatosis, TB, Budd-Chiari syndrome, fungal (eg, coccidioidomycosis) <2.5 g/dL (low-protein ascites) Cirrhosis, nephrotic syndrome
SAAG
≥1.1 g/dL (indicates portal hypertension) Cardiac ascites, cirrhosis, Budd-Chiari syndrome <1.1 g/dL (absence of portal hypertension) TB, peritoneal carcinomatosis, pancreatic ascites, nephrotic syndrome
Ascites can be due to portal hypertensive (eg, cardiac ascites, cirrhosis) or non-portal hypertensive (eg, malignancy, pancreatitis, nephrotic syndrome, tuberculosis) causes. Assessment of color, neutrophil count, total protein, and the serum-to-ascites albumin gradient (SAAG) in ascitic fluid analysis can help to diagnose the etiology.
SAAG is calculated by subtracting the peritoneal fluid albumin concentration from the serum albumin concentration and is useful to differentiate between portal and non-portal hypertensive etiologies. A SAAG >1.1 g/dL indicates portal hypertension while a SAAG <1.1 g/dL suggests other causes. This patient's SAAG of 1.3 g/dL (3.8 – 2.5 g/dL) is consistent with portal hypertension (eg, cirrhosis) with increased hydrostatic pressure within hepatic capillary beds.
Brain bleeds

Cardiac Stress Test
Type of stress
Mechanism
Best for
Not for
Exercise ECG test
↑ HR↑ BP
Patients able to reach tHR (tHR = 85% of 220 − age)
LBBB Pacemaker Patients unable to reach tHR
Pharmacologic stress test with adenosine or dipyridamole
Nonselective adenosine agonist Dilates coronary arteries without ↑ HR or BP
LBBB Pacemaker Patients unable to reach tHR
Reactive airway disease Patients on dipyridamole or theophylline
Dobutamine stress echocardiography
Β-1 agonist ↑ HR ± BP
Reactive airway disease Patients unable to reach tHR
Tachyarrhythmias
IO Line
When intravenous access cannot be obtained in emergency cases, intraosseous (IO) access should be attempted immediately. IO access requires less skill and practice than central line placement, and clinical trials have demonstrated IO lines to be safer and faster than central lines. IO catheters provide a cannula large enough to deliver fluids and medications rapidly and to obtain blood samples for laboratory testing.
The most common site for IO access is the proximal tibia due to its wide, flat surface and distance from the sternum in case cardiopulmonary resuscitation is performed simultaneously. However, any large bone can be used. IO catheters can be placed manually or with a driver. Contraindications to IO placement include infection (eg, cellulitis) overlying the access site, fracture or previous IO attempts in the chosen extremity, or bone fragility (eg, osteogenesis imperfecta).
Septic Thrombophlebitis
postpartum fever unresponsive to abx and negative infection evaluation.,
vesiculourethral Reflux

Recurrent urinary tract infections (UTIs) in infants and children are a serious problem as they often involve the kidney and signify a congenital urinary tract anomaly. One of the most common abnormalities is primary vesicoureteral reflux (VUR). Normal urine should have unidirectional flow from the kidneys, ureters, bladder, and out the urethra. Patients with severe VUR have urinary reflux from the bladder into the kidney, and the regurgitant urine causes dilation of the ureters (hydroureter) and kidneys (hydronephrosis).
The definitive diagnosis of VUR is made by contrast voiding cystourethrogram. Renal ultrasound is performed to screen for hydronephrosis. Recurrent and/or chronic pyelonephritis can lead to blunting of calices (calyceal clubbing) and focal parenchymal scarring. Renal scintigraphy with dimercaptosuccinic acid is the preferred modality for long-term evaluation for renal scarring. Renal function should be followed by serial creatinine. Patients should be monitored closely for complications of chronic renal insufficiency, such as hypertension and anemia.
LAD

This child's presentation of recurrent bacterial infections, severe periodontitis, and marked leukocytosis is consistent with leukocyte adhesion deficiency (LAD). LAD is caused by defective integrins on the leukocyte surface, which normally allow neutrophils to adhere to vascular endothelium, exit the vasculature, and migrate to areas of infection or inflammation.
Lack of neutrophil migration in LAD results in recurrent skin (eg, cellulitis, abscess, omphalitis) and mucosal (eg, periodontal) infections as well as poor wound healing. Examination shows inflammation with a notable lack of purulence. Biopsy of infected tissue is devoid of neutrophils and culture often grows Staphylococcus aureus or Gram-negative bacilli. Peripheral serum studies show marked leukocytosis and neutrophilia, particularly during episodes of infection. Classically, the first presenting sign of LAD is delayed umbilical cord separation (age >3 weeks).
Hypothyroid Myopathy
In a relatively young, otherwise healthy woman with fatigue and delayed deep tendon reflexes, this presentation is most consistent with hypothyroid myopathy. Myopathy occurs in over one third of patients with hypothyroidism, and can range from an asymptomatic elevation in CK to myalgias, muscle hypertrophy, proximal myopathy, and rhabdomyolysis. Serum CK can be elevated for years before a patient develops clinical symptoms of hypothyroidism, and there is no clear correlation between the degree of CK elevation and severity of muscle disease. Inflammatory markers (eg, erythrocyte sedimentation rate, C-reactive protein) may be normal or mildly elevated
NF
Neurofibromatosis types 1 & 2
Diagnosis
NF1 (von Recklinghausen disease)
NF2 (central neurofibromatosis)
Gene mutation
NF1 tumor suppressor gene; codes the protein neurofibromin
NF2 tumor suppressor gene; codes the protein merlin
Location of mutated gene
Chromosome 17
Chromosome 22
Main clinical features
Café-au-lait spotsMultiple neurofibromasLisch nodules
Bilateral acoustic neuromas
Neurofibromatosis type 1 (NF1) is an autosomal dominant neurocutaneous syndrome. Café-au-lait macules are the earliest manifestations. Numerous macules can appear as early as infancy. With increasing age, axillary/inguinal freckles, Lisch nodules (iris hamartomas), and neurofibromas (benign peripheral nerve sheath tumors) become significant. Patients with NF1 are also at risk for developing intracranial neoplasms. Optic pathway glioma is the most common type of intracranial lesion and typically manifests during toddlerhood.
This patient's holocranial headache (pain involving the whole head), vision changes, vomiting, and hypertension may indicate a symptomatic intracranial mass. An MRI of the brain and orbits should be ordered to thoroughly evaluate the intracranial structures. It is more sensitive and specific than CT in showing soft-tissue contrast and anatomy.
Reflex
By age 6 months, primitive reflexes (eg, Moro, grasp) have typically already disappeared as the infant initiates purposeful movement of the extremities. The tongue protrusion reflex also disappears by age 4-6 months, allowing for coordination to ingest solid foods at this age. The Babinski reflex is the only primitive reflex that may persist in healthy children up to age 2 years but can disappear as early as age 12 months.
Focal Generalized Seizures
Seizures can be classified as focal or generalized. Focal seizures arise from a discrete focus in the brain but can spread to the entire brain (ie, focal with secondary generalization); generalized seizures involve both hemispheres of the brain from the beginning of the event.
Tongue-biting, urinary incontinence, and perioral cyanosis may be seen during or after seizures, but these characteristics can also be seen in syncopal or nonepileptiform events. After a generalized seizure, the child typically enters a postictal phase of sleepiness and confusion for minutes to hours. This phase does not occur in vasovagal syncope (Choice G), the most common cause of syncope in children; rather, these events typically occur after prolonged standing or stressful experiences and are preceded by a prodrome of dizziness and/or visual changes.
Cervical Adenitis

Acute lymphadenitis (LAD) arises over a few days, whereas subacute/chronic LAD has a more indolent presentation over weeks to months. This child has acute, unilateral LAD, which is most commonly caused by *Staphylococcus aureus* and *Streptococcus pyogenes*. Acute LAD is most common in children age <5 and usually affects the submandibular nodes. Affected lymph nodes are enlarged, markedly tender, warm, and erythematous. If untreated, LAD can progress to suppuration and abscess.
The diagnosis of uncomplicated acute lymphadenitis can usually be made clinically. Empiric antibiotic therapy for acute, unilateral lymphadenitis typically involves clindamycin, which has activity against methicillin-resistant S aureus as well as S pyogenes.
Adenovirus and other upper respiratory tract infections are the most common cause of acute, bilateral LAD. Adenovirus can cause marked fever, pharyngitis, and conjunctivitis along with LAD.
Non-tuberculous mycobacteria (eg, Mycobacterium avium) are the most common cause of subacute unilateral LAD in young children. The onset is very slow and the affected lymph node is not tender.
Oral anaerobes, such as Prevotella sp, can cause acute LAD in the setting of poor dentition and caries. This child's dentition is normal.
Last updated