Uworld 4
multiple myeloma: anemia, hypercalcemia, bone pain, renal insufficiency
Rabies

Rabies is a fatal, neurotropic, viral disease transmitted to humans by exposure to saliva from an infected animal through a bite. Hydrophobia and aerophobia are pathognomonic features of encephalitic rabies; the feeling of water or air triggers involuntary pharyngeal muscle spasms. Many patients are disoriented and agitated, with fluctuating mental status. The incubation period is 1-3 months, and almost all patients die within weeks of developing symptoms.
The majority of rabies transmissions in the United States are caused by bat bites. Other high-risk reservoirs of rabies in the United States include raccoons (Choice C), foxes, and skunks. In contrast to the bites of these other animals, bat bites are small and relatively painless; they often go unnoticed initially and may occur during sleep. Therefore, all patients with direct exposure to bats require rabies prophylaxis unless they were aware of the bat at all times and are certain they were not bitten.
Known bites from bats or other high-risk animals require thorough wound cleansing with soap and water and urgent postexposure prophylaxis, which includes both rabies immune globulin and rabies vaccine. Prophylaxis can prevent progression to life-threatening encephalitic or paralytic rabies disease.
Bipolar
bipolar I: manic episode, no depression. 7 days, psychosis
bipolar II: hypomanic episode, must have depression in past
Vitreous Hemorrhage
Vitreous hemorrhage typically presents as a sudden loss of vision and onset of floaters. The most common cause is diabetic retinopathy. An important diagnostic clue is that the fundus is hard to visualize, and even if it is visualized, details may be obscured. Immediate ophthalmologic consultation is required. For patients with underlying medical conditions, conservative treatment (i.e upright position during sleep, which enhances settling of the hemorrhage) is recommended
LEMS

Chikungunya Fever
Chikungunya fever
Epidemiology
Central & South America, tropical regions of Africa, South Asia Vector: Aedes mosquito (same as dengue fever)
Clinicalmanifestations
Incubation period: 3-7 daysHigh fevers, severe polyarthralgias (virtually always present) Headache, myalgias, conjunctivitis, maculopapular rash Lymphopenia, thrombocytopenia, elevated liver enzymes
Management
Supportive care (resolves in 7-10 days) Development of chronic arthralgias, which may require methotrexate, in approximately 30%
Vitamins

Eye Problems
Dacryocystitis is an infection of the lacrimal sac. It usually occurs in infants and adults over the age of 40. Acute dacryocystitis is characterized by the sudden onset of pain and redness in the medial canthal region. Sometimes, a purulent discharge is noted from the punctum. A few patients present with fever, prostration, and an elevated leukocyte count. Staphylococcus aureus and beta-hemolytic Streptococcus are the usual infecting organisms. It usually responds to systemic antibiotic therapy.

(Choice A) Episcleritis is an infection of the episcleral tissue between the conjunctiva and sclera. Patients complain of an acute onset of mild to moderate discomfort, photophobia, and watery discharge. Examination reveals diffuse or localized bulbar conjunctival injection.
(Choice C) Hordeolum refers to an abscess located over the upper or lower eyelid. It is usually caused by Staphylococcus aureus. It appears as a localized red, tender swelling over the eyelid.

(Choice D) Chalazion presents as lid discomfort. It is a chronic, granulomatous inflammation of the meibomian gland. It appears as a hard, painless lid nodule.

Central retinal artery occlusion: retinal whitening and cherry red macula
Central retinal vein occlusion: dilated and tortuous veins leading to scattered and diffuse hemorrhages ("blood and thunder"), disk swelling, and/or cotton wool spots.
Patients with hypertensive retinopathy typically do not have acute vision loss. On funduscopy, there is focal spasm of arterioles, followed by progressive sclerosis and narrowing. Depending on the severity, arteriovenous nicking, copper or silver wiring, exudates, and/or hemorrhages may be present.

TTP
TTP
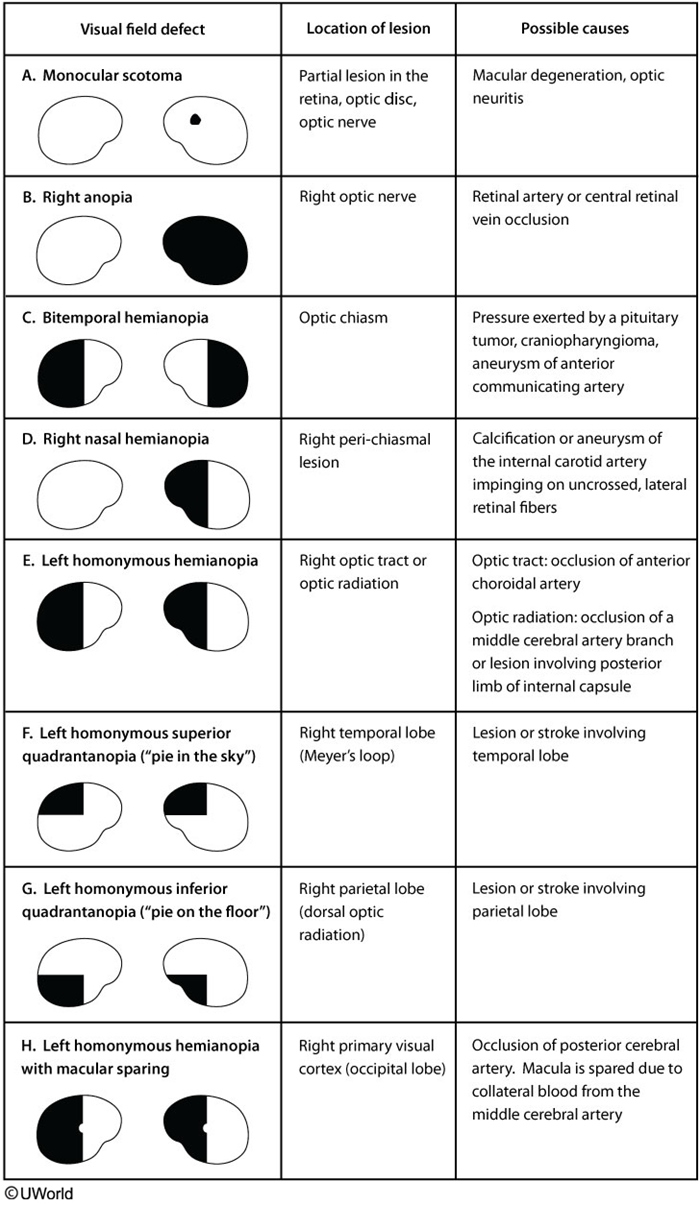
Visual Field Defect
Pregnancy Hypertension

HCM

Retinitis
CMV: painless
toxo: painful

CMV retinitis is characterized by full-thickness retinal inflammation that moves centripetally along the vasculature, causing edema and scarring. Patients experience blurred vision, floaters, and photopsia (sensation of flashing lights). Lesions near the fovea and optic nerve may cause blindness, and scarring greatly increases the risk of retinal detachment. Diagnosis is made by fundoscopyshowing yellow-white, fluffy, hemorrhagic lesions along the vasculature.
Patients with toxoplasmic chorioretinitis present with eye pain and decreased vision. Retinal lesions appear in a nonvascular distribution. This patient does not have eye pain and has lesions in a perivascular distribution.
CO
Carbon monoxide is a colorless, odorless gas emitted by automobiles, furnaces and charcoal grills. When inhaled, it prevents the body's tissues from utilizing oxygen effectively. Acute exposure can present with headaches, nausea, vomiting, abdominal discomfort, confusion and coma. Patients often present with a pinkish-red skin hue. Diagnosis is established by obtaining carboxyhemoglobin levels. Treatment consists of hyperbaric oxygen administration.
Methehemoglobinemia: cyanosis
Burning of rubber or plastic, not wood, can result in cyanide inhalation. The symptoms can be similar to those of carbon monoxide exposure, so the history is very important. Bitter almond breath is characteristic of inhaled cyanide.
VAP

This intubated patient's presentation suggests ventilator-associated pneumonia (VAP). VAP is a type of nosocomial pneumonia that usually develops >48 hours after endotracheal intubation. It is most commonly caused by aerobic gram-negative bacilli (eg, Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae) and gram-positive cocci (eg, methicillin-resistant Staphylococcus aureus, Streptococcus). Patients usually have fever, purulent secretions, difficulty with ventilation (eg, increased respiratory rate, decreased tidal volume), and leukocytosis.
The first step is to obtain a chest x-ray. Patients with a normal chest x-ray are unlikely to have VAP and should be evaluated for other causes. Those with an abnormal chest x-ray (eg, alveolar infiltrates, air bronchograms, silhouetting of adjacent solid organs) require lower respiratory tract sampling (ie, tracheobronchial aspiration) for microscopic analysis (Gram stain) and culture (Choice E). Patients should receive empiric antibiotics (usually gram-positive, anti-pseudomonal, and gram-negative coverage) until culture susceptibility results return as treatment delay can increase mortality. However, respiratory tract sampling should be done prior to starting antibiotics as treatment can decrease the sensitivity of both the Gram stain and culture.
TS
Transient Synovitis
Septic Arthritis
Clinical presentation
Well-appearing Afebrile or low-grade fever Able to bear weight
Ill-appearing Febrile Non–weight-bearing
Diagnosis
Normal or mildly elevated WBC, ESR, CRP Unilateral/bilateral ultrasound effusion Diagnosis of exclusion
Moderately elevated WBC, ESR, CRP± Positive blood culture Unilateral ultrasound effusion Synovial fluid WBC >50,000/mm3
Treatment
Conservative
Joint drainage & antibiotics
Transient synovitis is a common cause of hip pain in children, typically occurring in boys age 3-8. The cause is unknown but symptoms may develop days to weeks after a mild viral illness, such as in this patient. Synovial inflammation leads to pain, decreased range of motion, and a limp. On examination, patients are well-appearing and afebrile. The affected hip may be flexed, slightly abducted, and externally rotated. This position maximizes the joint space, thereby providing pain relief.
Laboratory evaluation shows a normal white blood cell (WBC) count and inflammatory markers (eg, C-reactive protein [CRP], erythrocyte sedimentation rate) due to lack of infection or significant inflammation. X-rays reveal normal hip joints, but ultrasound may show small bilateral effusions even if symptoms are unilateral. Treatment consists of rest and nonsteroidal anti-inflammatory medications (eg, ibuprofen). Children usually recover within 1-4 weeks with no complications.
Lower back pain
Indications for imaging in low back pain
X-ray
Osteoporosis/compression fracture Suspected malignancy Ankylosing spondylitis (eg, insidious onset, nocturnal pain, better with movement)
MRI
Sensory/motor deficits Cauda equina syndrome (eg, urine retention, saddle anesthesia) Suspected epidural abscess/infection (eg, fever, intravenous drug abuse, concurrent infection, hemodialysis)
Radionuclide bone scan or CT scan
Indications for, but patient not able to have, MRI
Takayasu

This patient with exertional arm pain (likely claudication), systemic symptoms, and pulse deficits has typical features of Takayasu arteritis, a chronic large artery vasculitis that predominantly affects Asian women age <40. It primarily involves the aorta and its branches and is characterized by mononuclear infiltrates and granulomatous inflammation of the vascular media, leading to arterial wall thickening with aneurysmal dilation or narrowing and occlusion.
Initial symptoms are nonspecific (eg, fever, arthralgias, weight loss). As the disease progresses, vascular involvement with arterio-occlusive manifestations (eg, claudication, distal ulcers) may develop, particularly in the upper extremities. Examination findings include blood pressure discrepancies, pulse deficits, and bruits. Patients commonly have anemia and elevated inflammatory markers (eg, erythrocyte sedimentation rate, C-reactive protein). Chest x-ray can reveal aortic dilation and a widened mediastinum, and CT and MRI may reveal thickening of large artery walls and narrowing of the arterial lumen. Initial treatment includes systemic glucocorticoids.
Cyanide
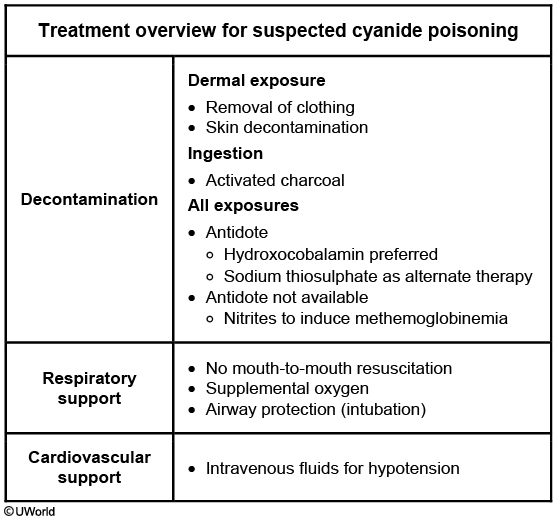
This patient is the victim of a house fire and most likely has a smoke inhalation injury; such injuries are estimated to cause 60%-80% of deaths during fire incidents. Smoke injury results in glottic edema from heat and airway irritation due to particulate matter found in smoke. Smoke also contains multiple toxins that are absorbed systemically. Hydrogen cyanide (HCN) and carbon monoxide (CO) are the 2 major products of combustion in closed spaces. HCN is produced from the combustion of nitrogen-containing synthetic polymers (eg, foam, cotton, paint, silk).
HCN is a potent and fast-acting poison, and blood levels cannot be measured rapidly to confirm diagnosis prior to treatment. Toxic exposure can be inhalational, dermal, or intestinal. Exposure to moderate to high concentrations causes symptoms to develop within seconds to minutes. Early acute toxicity causes neurologic and cardiorespiratory stimulation, and patients develop headache, vertigo, dizziness, hyperventilation, tachycardia, nausea, and vomiting. Neurologic, respiratory, and cardiovascular depression eventually occurs and manifests as coma, seizures, bradycardia, hypotension, and cardiorespiratory arrest. HCN can also cause anoxic brain injury leading to permanent neurologic deficits.
Cyanide toxicity can be treated with an antidote such as hydroxocobalamin or sodium thiosulfate, which directly binds cyanide molecules. An alternate treatment is induction of methemoglobinemia with nitrites to increase ferric iron (Fe3+) in circulating hemoglobin. Cyanide binds avidly to Fe3+, and so methemoglobinemia provides an alternate binding site.
AIN
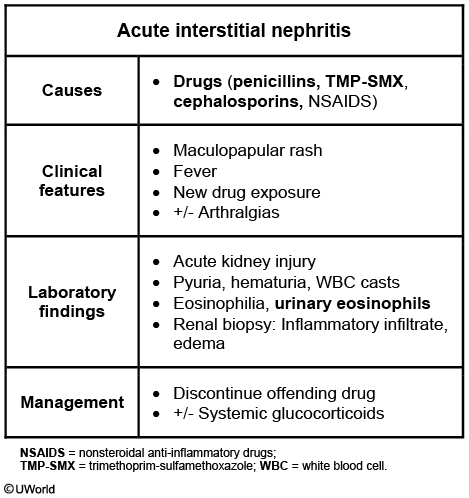
The clinical presentation is typical of allergic interstitial nephritis (AIN): acute renal failure, fever, rash, a recent history of para-aminobenzoic acid analogue antibiotic (sulfonamide) ingestion, and white blood cell (WBC) casts on urinalysis. Patients may also have arthralgias and eosinophiluria. Symptoms usually appear 5 days to several weeks after use of an offending agent. Drugs cause the majority of AIN cases; examples include antibiotics (eg, penicillins, cephalosporins, trimethoprim, rifampin), nonsteroidal anti-inflammatory drugs, and diuretics. Less commonly, AIN may be caused by infectious agents (eg, Legionella, Mycobacterium tuberculosis, Streptococcus).
Metabolic Alkalosis
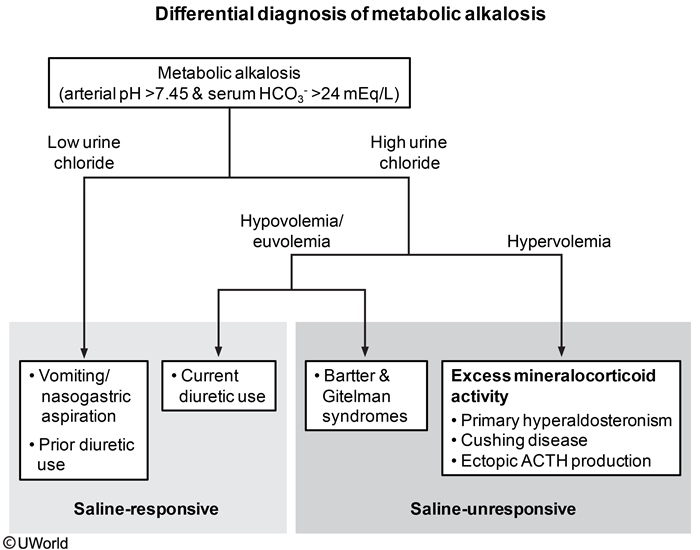
This patient's presentation is consistent with metabolic alkalosis, defined as arterial pH >7.45 and serum bicarbonate level >24 mEq/L. Metabolic alkalosis can be further classified as saline-responsive and saline-unresponsive. It can also be classified according to low (<20 mEq/L) or higher levels of urinary chloride. Saline-unresponsive metabolic alkalosis typically presents with a higher level of urinary chloride (>20 mEq/L). Patients can have expanded extracellular fluid (ECF) with hypervolemia (eg, primary hyperaldosteronism, Cushing syndrome, excessive black licorice ingestion) or appear hypo/euvolemic (eg, Bartter syndrome, Gitelman syndrome). These conditions require treatment of the underlying disorder; the metabolic alkalosis is not corrected by saline infusion alone.
Saline-responsive metabolic alkalosis is commonly due to loss of gastric secretions (eg, self-induced or spontaneous vomiting, nasogastric suctioning) that results in ECF loss. Patients typically develop volume depletion (eg, hypotension, orthostasis) and low serum Cl- due to chloride loss in the gastric secretions. The ECF loss leads to increased renal mineralocorticoid levels, increased renal sodium and chloride reabsorption, and increased urinary H+ and K+ excretion. The end result is decreased urine chloride, hypokalemia, and metabolic alkalosis. Prior use of thiazide or loop diuretics will also lower urine chloride, but current diuretic use increases urine chloride. Low serum Cl- also impairs renal HCO3- excretion and further worsens the alkalosis. Saline-responsive metabolic alkalosis usually corrects with isotonic saline infusion alone and restores both ECF volume and low serum Cl-.
Felty syndrome
This triad of clinical findings is characteristic of Felty syndrome (FS).
Dermatofibroma

This patient's skin lesion is consistent with a dermatofibroma (DF), which is due to fibroblast proliferation causing isolated or multiple lesions, most commonly on the lower extremities. The etiology is unknown, but some patients may develop lesions after trauma or insect bites. Typical lesions are nontender and appear as discrete, firm, hyperpigmented nodules that are usually <1 cm in diameter. The lesions have a fibrous component that may cause dimpling in the center when the area is pinched ("dimple" or "buttonhole" sign).
Diagnosis of DF is made clinically based on the appearance of the lesion. Treatment (cryosurgery or shave excision) is usually not required unless the lesion is symptomatic, bleeds, or changes in color or size. Patients may also request treatment for cosmetic reasons or because of recurrent cuts when shaving the legs.
Pyogenic granuloma is a benign vascular skin tumor that presents as a small red papule that grows rapidly over weeks or months to a pedunculated or sessile shiny mass. The lesions most commonly occur on the lip and oral mucosa and can bleed with minor trauma.

Keratoacanthoma


Keratoacanthoma is a rapidly growing, "volcano-like" nodule with a central keratotic plug. Although these lesions may regress spontaneously, many are treated as well-differentiated squamous cell carcinomas. Early treatment is indicated if the lesion is near an important structure, such as the eye.
Transfusion Reaction



This patient most likely has febrile nonhemolytic transfusion reaction, the most common adverse reaction that occurs within 1-6 hours of transfusion. When red cells and plasma are separated from whole blood, small amounts of residual plasma and/or leukocyte debris may remain in the red cell concentrate. During blood storage, these leukocytes release cytokines, which when transfused can cause transient fevers, chills, and malaise, without hemolysis.
Management includes stopping the transfusion to exclude other serious reactions, administering antipyretics, and using leukoreduced blood products for future transfusions. Leukoreduction involves reducing the number of transfused leukocytes through filtering or other methods such as saline washing, freezing and deglycerolizing, or buffy coat removal. It also reduces the risk of human leukocyte antigen (HLA) alloimmunization and transmission of cytomegalovirus (which typically resides in leukocytes). Premedication with antipyretics and antihistamines has not been shown to significantly reduce transfusion reactions.
Thyroid
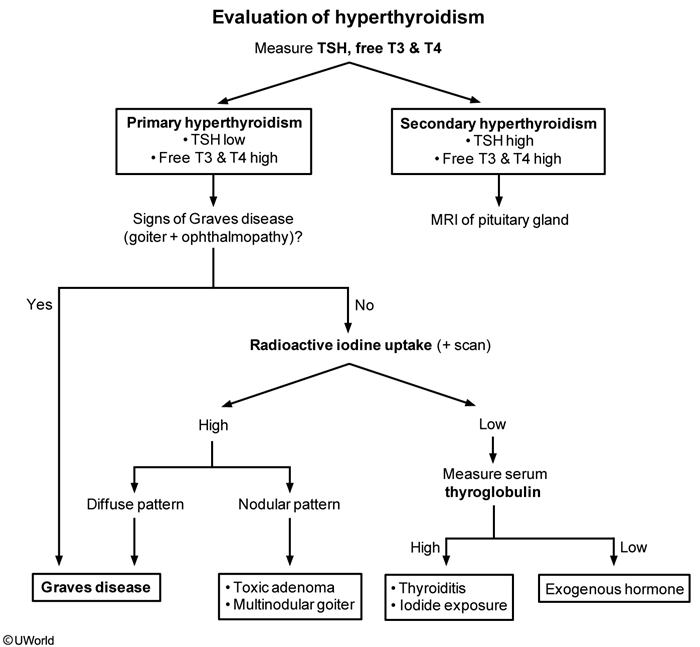
This patient, with fatigue, sweating, palpitations, and weight loss, has features of hyperthyroidism. The first step in evaluating hyperthyroidism is to measure serum TSH and free T4 levels. In the absence of a TSH-secreting pituitary adenoma (secondary hyperthyroidism), patients with hyperthyroidism will have an elevated T4 and suppressed TSH. The most common cause of hyperthyroidism is Graves' disease, which is caused by an autoantibody to the TSH receptor and is characterized by a diffuse goiter and ocular abnormalities (proptosis, periorbital edema). Patients with clear features of Graves' disease may be managed accordingly, but those without require further investigation.
Patients with undiagnosed hyperthyroidism may be evaluated further with radioactive iodine uptake (RAIU), usually with scan. A high RAIU suggests de novo hormone synthesis due to Graves' disease (diffusely increased uptake) or toxic nodular disease (nodular uptake). In contrast, a low RAIU suggests either release of preformed thyroid hormone (ie, thyroiditis) or exogenous thyroid hormone intake. In such cases, the serum thyroglobulin level can make the distinction: elevated thyroglobulin is consistent with endogenous thyroid hormone release whereas decreased thyroglobulin suggests exogenous or factitious thyrotoxicosis. In this patient, it is likely that her weight loss supplement contains thyroid hormone derived from porcine or other animal sources.
Febrile Neutropenia
Neutropenia is defined as an absolute neutrophil count (ANC) <1500/µL (severe neutropenia is ANC <500/µL). Patients with ANC <1000/µL are at higher risk for overwhelming bacterial infection due to an absent or blunted neutrophil-mediated inflammatory response. Chemotherapy may also lead to disruption of the skin and mucosal barrier of the mouth and gastrointestinal tract, resulting in mucositis and subsequent translocation of the bacteria into the bloodstream. Gram-negative organisms, particularly Pseudomonas aeruginosa, are most frequently identified. Gram-positive infections are also common and increasing in frequency.
Febrile neutropenia is a medical emergency, and starting early empiric antibiotic therapy can avoid progression of infection to severe sepsis and life-threatening complications. Initial evaluation includes blood and urine cultures, followed by immediate intravenous broad-spectrum antibiotics. Monotherapy with an anti-pseudomonal beta-lactam agent (eg, cefepime, meropenem, piperacillin-tazobactam) provides both gram-negative and gram-positive coverage and is recommended initially.
CML

Patients with CML may present asymptomatically, although fatigue, night sweats, weight loss, and abdominal fullness (due to splenomegaly) are not uncommon. Patients may experience weight loss and early satiety from splenomegaly. Peripheral blood smear in CML reveals dramatic leukocytosis (often >100,000/mm3) with absolute basophilia and a shift toward very early neutrophil precursors (promyelocytes, myelocytes).
Antipsychotics
Second-generation antipsychotic side effects
Weight gain/metabolic syndrome
Extrapyramidalside effects
Prolonged QTc
Aripiprazole
Low
Low
Low
Olanzapine
Very high
Low
Low
Risperidone
High
High
High
Ziprasidone
Low
Low
High
Clozapine
Very high
Low
Low
Quetiapine
High
Low
Low
Serotonin

C Different
Treatment of Clostridium difficile infection
Initial episode
Vancomycin PO ORFidaxomicin
Recurrence
First recurrence Vancomycin PO in a prolonged pulse/taper course OR Fidaxomicin if vancomycin was used in initial episode Multiple recurrences Vancomycin PO followed by rifaximin (or above regimens) Fecal microbiota transplant
Fulminant (eg, hypotension/shock, ileus, megacolon)
Metronidazole IV plus high-dose vancomycin PO (or PR if ileus is present) Surgical evaluation
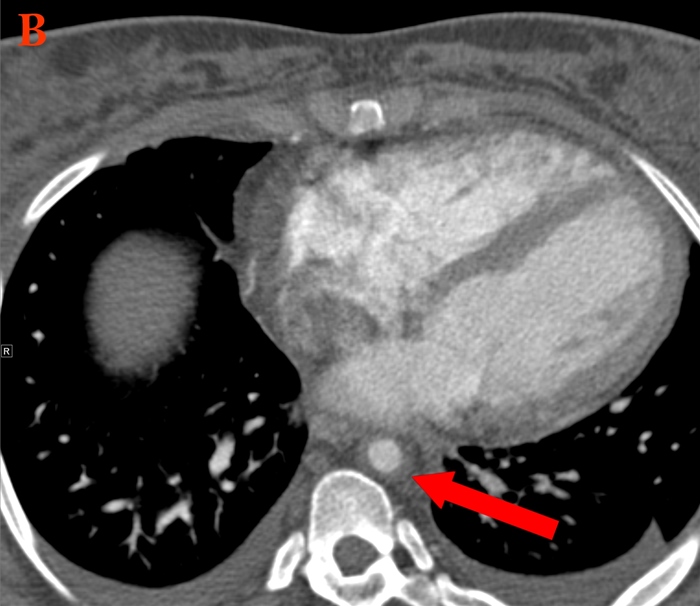
Esophageal Perforation
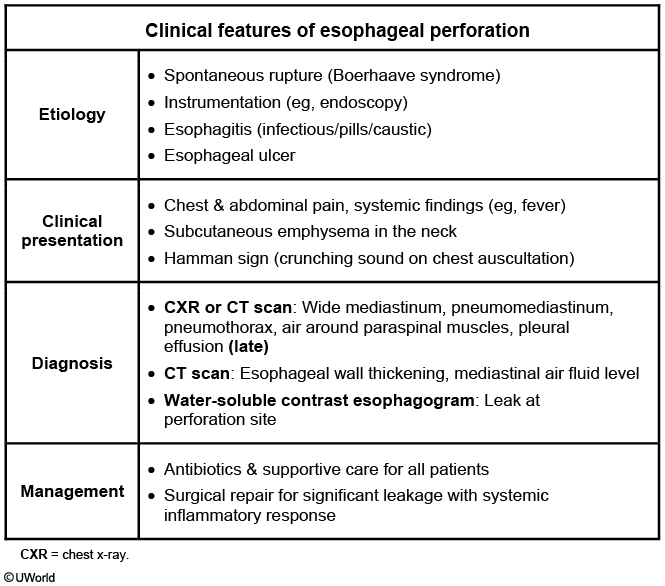
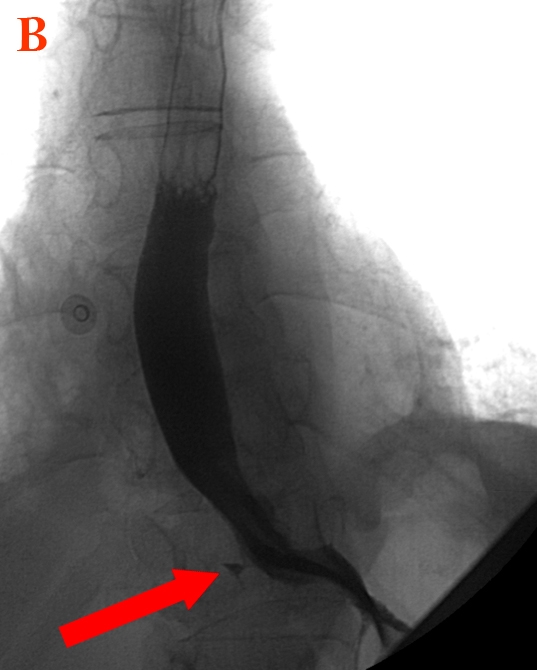
This patient has features of acute esophageal rupture, including acute chest pain, tachypnea, and pleural effusion (often left-sided). Patients also frequently have subcutaneous emphysema. Endoscopy is the most common cause of esophageal rupture (especially when performed with additional interventions, such as dilation of strictures), although rupture can also be due to severe retching (Boerhaave syndrome) or penetrating trauma.
Esophageal rupture is a life-threatening condition that requires emergent evaluation. A contrast esophagram is recommended to confirm the diagnosis and can demonstrate contrast extravasation through the tear. Water-soluble contrast is preferred (less inflammatory to tissues), but a barium study has higher sensitivity and would be advised if the initial water-soluble contrast study is nondiagnostic. If perforation is confirmed, primary closure of esophagus and drainage of mediastinum must be attempted urgently to prevent the development of mediastinitis.
Medication Induced Esophagitis
Medication-induced esophagitis
Drug class
Drug
Antibiotics
Tetracyclines
Anti-inflammatory agents
Aspirin & many nonsteroidal anti-inflammatory drugs
Bisphosphonates
Alendronate, risedronate
Others
Potassium chloride, iron
This patient has abrupt-onset retrosternal pain and severe odynophagia, suggestive of medication-induced esophagitis (pill esophagitis). Pill esophagitis is due to a direct effect of certain medications on esophageal mucosa. Mucosal injury in pill esophagitis can be due to acid effect (eg, tetracyclines), osmotic tissue injury (eg, potassium chloride), or disruption of normal gastroesophageal protection (eg, nonsteroidal anti-inflammatory drugs). Patients usually do not have prior esophageal disease, although pill esophagitis can be worse in those with concurrent gastroesophageal reflux.
Typical symptoms of pill esophagitis include sudden-onset odynophagia and retrosternal pain that can sometimes cause difficulty swallowing. It is most common in the mid-esophagus due to compression by the aortic arch or an enlarged left atrium. The diagnosis is usually made clinically but can be confirmed on endoscopy, which shows discrete ulcers with relatively normal-appearing surrounding mucosa. Treatment includes primarily stopping the offending medication to prevent future injury.
Hematuria

Gross (ie, visible or macroscopic) hematuria can be classified based on the stage of voiding at which bleeding predominates:
Initial hematuria is characterized by blood at the beginning of the voiding cycle.
Total hematuria is characterized by blood during the entire voiding cycle.
Terminal hematuria is characterized by blood at the end of voiding cycle.
Terminal hematuria often suggests bleeding from the prostate, bladder neck or trigone, or posterior urethra. In this patient, the presence of terminal hematuria with clots suggests bleeding within the bladder or ureters and is concerning for urothelial cancer, particularly given his risk factors of age (>40), sex, and smoking. He should be evaluated for bladder cancer by cystoscopy.
PSC

Thalassemia

Cardiac Myxoma
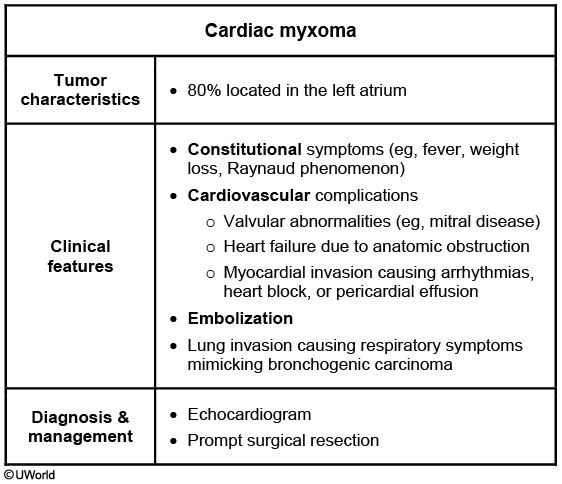
This patient's presentation of chronic systemic symptoms (eg, fever, weight loss, fatigue), embolic phenomenon (left-sided weakness), and echocardiogram findings is suggestive of cardiac myxoma. Myxomas are the most common benign primary cardiac tumors with approximately 80% located in the left atrium.
Left atrial myxomas can cause obstruction of blood flow across the mitral valve, mimicking mitral valve disease and producing early diastolic sound ("tumor plop"). Patients often present with fatigue, cough, dyspnea, orthopnea, pulmonary edema, or hemoptysis. Left atrial tumors can also cause systemic embolization(eg, transient ischemic attack, stroke, splenic infarcts). About 50% of patients report constitutional symptoms (due to overproduction of interleukin-6) such as fever, weight loss, or Raynaud phenomenon.
Although transesophageal echocardiography is the most sensitive test for diagnosis, transthoracic echocardiography is usually adequate. Once diagnosis is established, prompt surgical resection is recommended to avoid complications of embolization and risk of sudden death.
Statistical Comparison
The two-sample t test is commonly employed to compare two means. Several statistical approaches can be used, but the basic requirements needed to perform this test are the two mean values, the sample variances, and the sample size. The t statistic is then obtained to calculate the p value. If the 'p' value is less than 0.05, the null hypothesis (that there is no difference between two groups) is rejected, and the two means are assumed to be statistically different. If the 'p' value is large, the null hypothesis is retained.
The two-sample z test can also be used to compare two means, but population (not sample) variances are employed in the calculations. Because population variances are not usually known, the test has limited applicability.
The ANOVA (i.e analysis of variance) is used to compare three or more means.
The chi-square test is appropriate for categorical data and proportions.
Meta-analysis is an epidemiologic method of pooling the data from several studies to do an analysis having a relatively big statistical power.
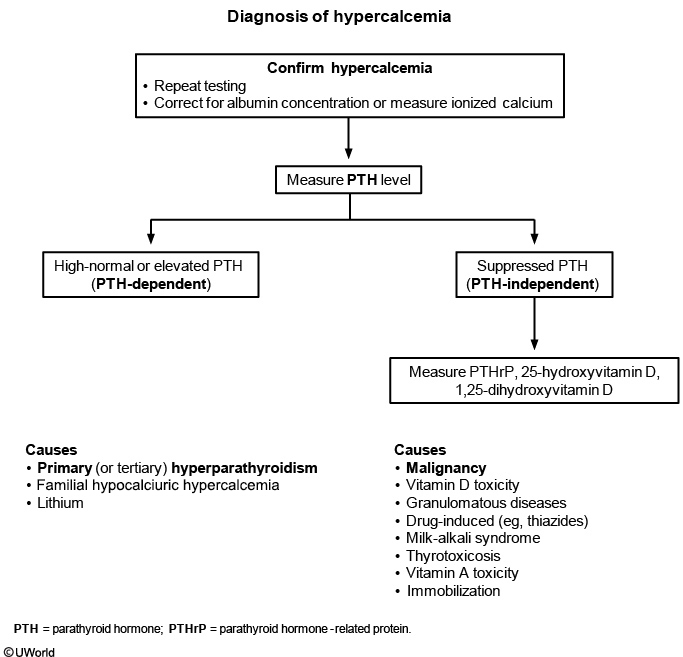
Hypercalcemia
HSV

This patient's presentation is consistent with viral encephalitis. The majority of acute viral encephalitis cases are due to unknown causes. However, herpes viruses (eg, herpes simplex, varicella, Epstein-Barr) most commonly cause encephalitis in immunocompetent adults. Patients typically present with fever, altered mental status, agitation, headaches, and seizures that can rapidly progress to complete unresponsiveness or coma. Examination can show neurologic abnormalities, including hemiparesis, cranial nerve palsies, and exaggerated deep-tendon reflexes. Clinical signs of meningeal irritation (eg, photophobia, nuchal rigidity) are usually absent in patients with pure encephalitis.
Lumbar puncture usually shows cerebrospinal fluid (CSF) findings of elevated white blood cell count with lymphocytic predominance, normal glucose, and normal to slightly elevated protein concentration (generally 100 mg/dL). Most patients have an increased red blood cell count as well. Diagnosis is usually confirmed by detecting viral DNA by polymerase chain reaction (PCR) in the CSF. Empiric treatment with intravenous acyclovir should be started while awaiting PCR results as encephalitis is often associated with significant morbidity and mortality.
CSF
Cerebrospinal fluid analysis
Diagnosis
WBC count(cells/µL)
Glucose(mg/dL)
Protein(mg/dL)
Normal
0-5
40-70
<40
Bacterial meningitis
>1,000
<40
>250
Tuberculous meningitis
100-500
<45
100-500
Viral meningitis
10-500
40-70
<150
Guillain-Barré
0-5
40-70
45-1,000
cryptococcus: elevated opening pressure, high ICP symptoms
Pancreatic Pseudocyst
In patients with minimal or no symptoms and without complications (eg, pseudoaneurysm), expectant management (eg, symptomatic therapy, nothing by mouth) is preferred initially. Endoscopic drainage is typically reserved for those (such as this patient) with significant symptoms (eg, abdominal pain, vomiting), infected pseudocyst, or evidence of pseudoaneurysm (usually embolized before drainage procedure).
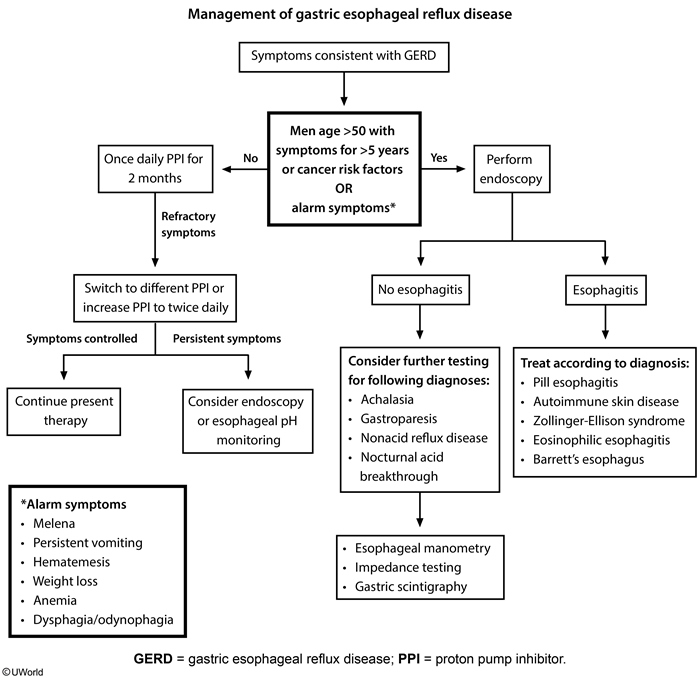
GERD
Fragile X

Fragile X syndrome (FXS) is an X-linked disorder that is the most common cause of inherited intellectual disability. Expansion of CGG' trinucleotide repeats in the fragile X mental retardation 1 gene of the X chromosome leads to the classic phenotype in affected males: large head, long face, prominent forehead, protruding ears, and macroorchidism. Female patients with the full mutation may have normal intellect, but many have mild intellectual disability and behavioral problems.
In addition to the physical features, patients with FXS often have speech and motor delays in early childhood and display features of attention-deficit hyperactivity disorder and autism spectrum disorder. Early diagnosis is crucial for appropriate developmental and behavioral services to be instituted at a young age.
Trinucleotide
CGG.,
CTG.,
GAA.,
CAG.,
Alcohol Use
First-line treatment options include naltrexone, a mu-opioid receptor antagonist, and acamprosate, a glutamate modulator.
Naltrexone has been shown to decrease alcohol craving, reduce heavy drinking days (defined as >5 drinks for men and >4 for women), and increase days of abstinence. It can be initiated while the patient is still drinking. It is contraindicated in patients taking opioids as it can precipitate withdrawal, and in those with acute hepatitis or liver failure. Acamprosate, which is primarily used to maintain abstinence, should be avoided in patients with significant renal impairment.
The aldehyde dehydrogenase inhibitor disulfiram is an aversive agent that causes an unpleasant physiologic reaction (tachycardia, flushed skin, headache, nausea, vomiting) when alcohol is consumed. It can be used only in abstinent patients and would not be preferred in this patient who is actively drinking. Candidates for disulfiram must be highly motivated or take the medication in a supervised setting as a patient may skip a dose to avoid the medication's aversive reaction when alcohol is desired. It is considered a second-line agent that is used when naltrexone and acamprosate are either ineffective or contraindicated.
Arsenic Poisoning
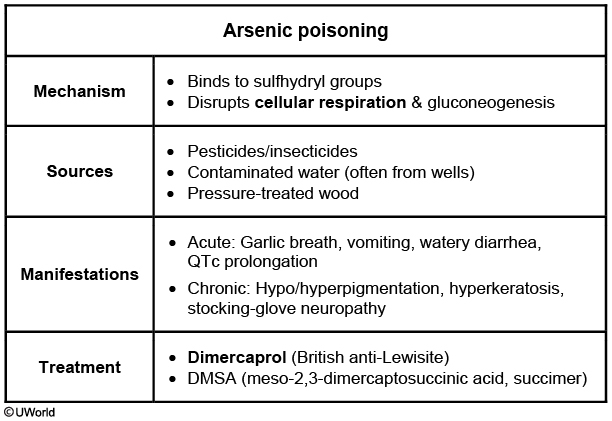
This patient, who is routinely exposed to antique wood, has polyneuropathy, pancytopenia, mild transaminase elevation, and a variety of skin lesions characteristic of chronic arsenic toxicity.
Arsenic is a metalloid element that exists in numerous forms, including both natural and manmade compounds. Although humans are often exposed to low levels through diet and water, toxic exposure is more likely through mining, pesticide manufacturing, metalworking, and working with antique pressure-treated wood preserved with arsenic. Arsenic binding to sulfhydryl groups and interfering with various enzymes is likely responsible for the clinical manifestations of acute and chronic arsenic toxicity.
Patients chronically exposed to arsenic develop a sensorimotor neuropathy in a stocking-glove distribution with burning, painful hypersensitivity, distal weakness, and hyporeflexia. Hypo- and hyperpigmentation of the skin occurs early in arsenic toxicity, and hyperkeratosis and scaling of the soles and palms is often seen later. Mees lines (horizontal striation of fingernails) are characteristic. Acute, severe arsenic toxicity can lead to profound pancytopenia and hepatitis, and chronic exposure leads to these manifestations to a smaller degree. Diagnosis is made through history, physical examination, and measurement of urine arsenic levels. Chelation (eg, dimercaprol, dimercaptosuccinic acid) is the treatment of choice for severe toxicity.
HACEK
This patient has developed infective endocarditis (IE) of the mitral valve due to infection with Eikenella corrodens. E corrodens belongs to the HACEK group of organisms, which includes *Haemophilus aphrophilus, **\Aggregatibacteractinomycetemcomitans (previously Actinobacillus actinomycetemcomitans), **\Cardiobacterium hominis*, *E corrodens*, and *K*ingella kingae. These organisms are responsible for only a minority (approximately 3%) of cases of IE. E corrodens is a Gram-negative anaerobe and a common constituent of normal human oral flora. IE due to E corrodens is usually seen in the setting of poor dentition and/or periodontal infection, along with dental procedures that involve manipulation of the gingival or oral mucosa.
Seborrheic Dermatitis
This patient with dandruff and a scaly rash involving the nasolabial folds has seborrheic dermatitis (SD). SD is a common inflammatory disease that affects the scalp (dandruff), face (eyebrows, nasolabial folds, and external ear canal/posterior ear), chest, and intertriginous areas. SD occurs in all ages but is most common in the first year of life and again at age 30-60. It is also associated with central nervous system disorders (especially Parkinson disease) and HIV.
The diagnosis of SD is clinical, with typical findings characterized by pruritic, erythematous plaques with fine, loose, yellow, and greasy-looking scales. SD primarily affects areas with numerous sebaceous glands, although sebum production in affected patients is typically normal. Malassezia species may play a role in the pathogenesis of SD, and topical antifungal agents (eg, ketoconazole, selenium sulfide) are effective in treating this condition.
Diverticulitis
Uncomplicated diverticulitis in stable patients can be managed in the outpatient setting with bowel rest, oral antibiotics, and observation (Choice D). However, hospitalization and intravenous antibiotics are recommended for patients who are elderly, immunosuppressed, have high fever or significant leukocytosis, or have significant comorbidities.
(Choices A, B, and C) Complicated diverticulitis refers to diverticulitis associated with an abscess (as seen in this patient), perforation, obstruction, or fistula formation. A fluid collection less than 3 cm can be treated with intravenous antibiotics and observation, with surgery reserved for patients with worsening symptoms. However, a fluid collection >3 cm should have CT-guided percutaneous drainage. If the symptoms are not controlled by the fifth day, surgical drainage and debridement are recommended. Sigmoid resection is generally reserved for patients with fistulas, perforation with peritonitis, obstruction, or recurrent attacks of diverticulitis.
Bipolar
Maintenance treatment typically involves continuation of mood stabilizers to treat the acute mood episode. Evidence-based monotherapy options include lithium, valproate, quetiapine, and lamotrigine.
Patients with inadequate response to monotherapy, severe episodes (eg, psychosis, aggression, suicidal behavior, hospitalization), and/or frequent episodes often require combination therapy. Lithium or valproate combined with a second-generation antipsychotic (eg, quetiapine) is recommended as first-line combination therapy.
Antidepressants (eg, fluoxetine, sertraline, venlafaxine) should generally be avoided in the maintenance treatment of bipolar I disorder due to the risk of mood destabilization. If an antidepressant is used to treat an acute depressive episode, it should be slowly tapered and discontinued during maintenance treatment. The anticonvulsant carbamazepine has been used in bipolar maintenance; however, it increases metabolism of both itself and other medications, making stable blood levels difficult to achieve.
Wilson's
Chelators (eg, D-penicillamine, trientine)
Zinc (interferes with copper absorption)
Last updated