Uworld
PVD
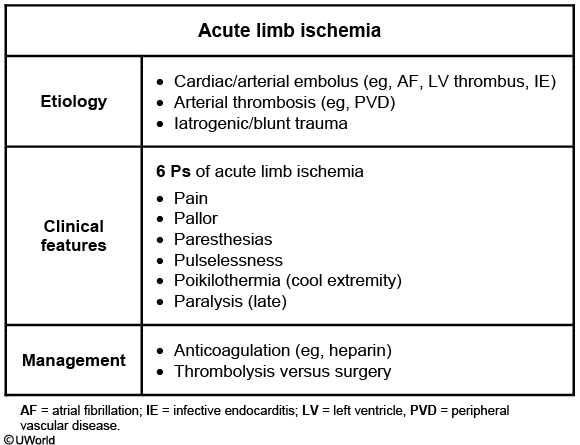
PVD: pulselessness, paresthesia, weak muscle
nerve compression: paresthesia, weak muscle, but no pulselessness
DVT: dull pain as opposed to sharp pain, no pulselessness
PAD
PAD is a coronary artery disease risk equivalent, and the medical therapy for such patients should include aggressive risk factor modification with counseling for smoking cessation, lipid-lowering therapy, and evaluation and treatment for hypertension and diabetes mellitus.
This patient is started appropriately on low-dose aspirin and statin therapy. The next step is to enroll the patient in a supervised exercise program. Exercise therapy for a minimum of 12 weeks, with 30-45 minutes of exercise at least 3 times a week, is recommended for all patients with claudication. The goal is to reproduce the claudication symptoms during each session. Supervised exercise programs have been shown in multiple clinical trials to reduce symptoms and improve the maximum walking distance in these patients.
Cardiac Emboli
Potential cardiac sources of emboli include left atrial thrombus due to atrial fibrillation, left ventricular thrombus following an anterior myocardial infarction (as is likely in this patient), infective endocarditis (ie, septic emboli), and thrombus from prosthetic valves.
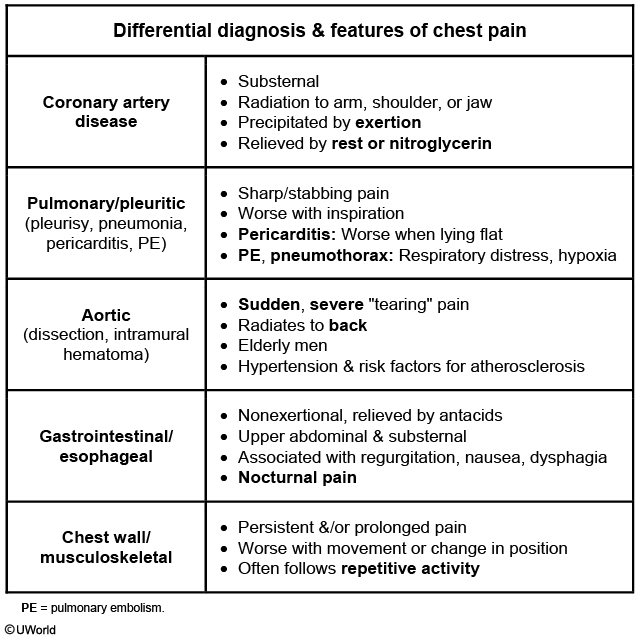
Pericarditis
myocarditis: audible S3 with pulmonary congestions
GERD Chest Pain
This patient's chest pain is most likely due to gastroesophageal reflux disease (GERD). Chest pain due to GERD can closely resemble anginal chest pain; however, the former is usually prolonged, occurs at rest or after meals, often awakens patients from sleep, and is typically relieved with antacids. In addition, patients with GERD will often have other associated symptoms (eg, cough, hoarseness) caused by reflux of gastric secretions into the larynx or upper pharynx.
The initial management of GERD in patients with fewer than 2 episodes of symptoms per week includes lifestyle changes (eg, weight loss, head-of-bed elevation) and histamine 2 receptor antagonists (eg, famotidine, ranitidine) as needed. Patients with more frequent or severe symptoms, evidence of erosive esophagitis, or laryngopharyngeal involvement should be managed with an 8-week course of a proton pump inhibitor (eg, omeprazole, pantoprazole).
Tamponade s/p CABG
echo to evaluate tamponade
Drug induced nephritis
Drug-induced interstitial nephritis can also present with acute kidney injury; however, urinalysis shows white blood cell casts and eosinophiluria. Patients may also have fever, rash, and eosinophilia. Thrombocytopenia and erythrocyte casts are not common.
Meningococcal vaccine
Meningococcal vaccination
Regular schedule (vaccinate at age 11-18)
Primary vaccination preferably at age 11-12 Booster at age 16-21 (if primary vaccination at age <16)
High-risk patients (vaccinate even if age >18)
Complement deficiency, asplenia College students in residential housing (age less than 21), military recruits Travel to endemic area, exposure to community outbreaks
Meningococcal vaccination with a quadrivalent (serotypes A, C, Y, W135) conjugate vaccine is recommended for all adolescents. This patient received primary vaccination at the recommended age (age 11-18; preferred age 11-12). However, he would benefit from a booster vaccine for several reasons:
In general, a booster vaccine should be provided at age 16 (up to age 21) if the primary vaccine was at age <16.
Meningococcal vaccination is also recommended before travel to highly endemic environments, such as most of sub-Saharan Africa and the Muslim hajj pilgrimage to Mecca, Saudi Arabia.
In addition, an increased risk of meningococcal meningitis is found among young adults in large groups living in close proximity, such as military recruits and first-year college students residing in dormitories (although the details of this patient's arrangements are unknown).
Primary vaccination can also be given to adults age >18 who are at increased risk for invasive meningococcal disease (eg, complement deficiency, functional or anatomic asplenia).
B19
Adults most commonly develop a polyarticular, symmetric arthritis (60% of cases) involving peripheral joints, including the hands (metacarpophalangeal [MCP], proximal interphalangeal [PIP], and wrist), knees, and ankles. Arthritis due to parvovirus B19 typically does not cause joint destruction or chronic arthritis. Other possible nonspecific findings include fever, fatigue, and diarrhea. Parvovirus B19 infection is diagnosed by detecting anti-B19 IgM antibodies in the serum, which develop within 10-15 days of infection and usually remain positive for 1-6 months. The symptoms typically resolve spontaneously in 2-3 weeks without the need for specific treatment.
Mono Diagnosis
Heterophile antibodies are specific, but test results may be negative early in the course of illness, especially during the first week. Repeating the test after several days may be helpful in establishing the diagnosis. For this reason, a negative antibody test does not exclude the diagnosis of IM.
Mono lymphocytes
Lymphoproliferation is a hallmark, and hematological studies reveal leukocytosis and variant lymphocytes with a large, vacuolated cytoplasm (atypical lymphocytes).
Liver Mets Diagnosis
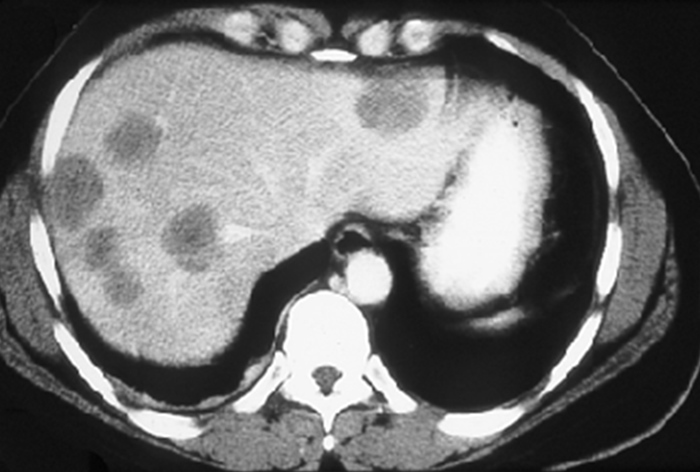
This patient with weight loss and fatigue has multiple liver lesions on CT scan, suggesting metastatic disease to the liver rather than primary liver cancer. Colorectal cancer is the most common source of liver metastases (as blood from the colon moves through the portal circulation directly to the liver) and should be excluded in this patient, even in the absence of specific symptoms (eg, alteration in bowel habits, gastrointestinal bleeding). Abdominal CT is a useful screening test but can often miss primary intraluminal tumors. Colonoscopy is the most appropriate next diagnostic step as it both localizes the tumor and provides a tissue diagnosis.
MI management
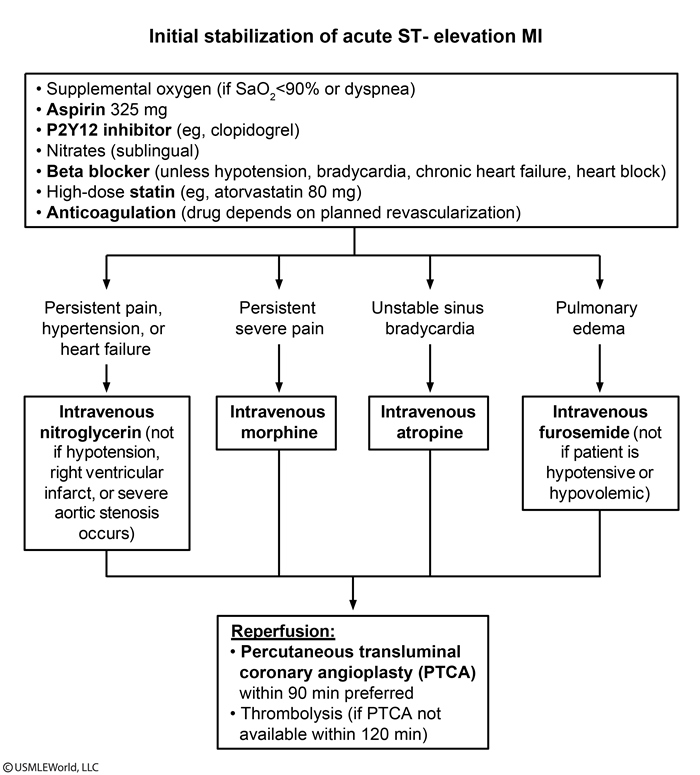
don't give beta blocker if pulmonary edema
Shock
Hemodynamic measurements in shock
Parameter
Normal
Hypovolemic shock
Cardiogenic shock
Septic shock
RA pressure (preload)
Mean 4 mm Hg
↓
↑
Normal or ↓
PCWP (preload)
Mean 9 mm Hg
↓
↑
Normal or ↓
Cardiac index (pump function)
2.8-4.2L/min/m2
↓
↓↓
↑
SVR (afterload)
1,150 dyne-sec/cm5
↑
↑
↓
MvO2
60%-80%
↓
↓
↑
ARDS: CI and PCWP normal
PE: low/normal PCWP and low CI due to decreased blood to LA
Pulmonary parenchymal hemorrhage describes diffuse alveolar hemorrhage, which results in hypoxemia and a responsive elevation (rather than depression) in CI
Tension pneumothorax results in obstruction of the vena cava and decreased venous return to the right atrium. Volume depletion (eg, massive hemorrhage) also leads to decreased venous return to the right atrium. In the setting of decreased right ventricular preload, PCWP and CI are both low.
Sarcoidosis
Glucocorticoids
Outlier
The mean (mathematical average) is extremely sensitive to outliers and easily shifts toward them, especially with a small sample size.
The median tends to be more resistant to outliers because it is splits an ordered dataset in its middle, where the observations usually do not differ much from one another.
The mode (the most frequently observed value) is less likely to be affected by outliers.
Catheter UTI
Catheter-associated urinary tract infection (CA-UTI) is a common complication of urinary catheter use and can be caused by:
Extraluminal ascent of microorganisms due to the ability of some pathogens (eg,Escherichia coli, Enterococcus spp, Candida spp, Pseudomonas aeruginosa) to form biofilm (slime-enclosed bacterial aggregates) along the catheter wall, allowing them to reach the bladder within 24 hours of catheter insertion
Intraluminal infection (less common) due to impaired urinary catheter drainage or contamination of a urinary collection bag
CA-UTI is most effectively prevented by avoiding unnecessary catheter use and minimizing the duration of catheterization. However, in patients with neurogenic bladder, long-term catheter use is required. In these patients, clean intermittent catheterization (CIC), which involves periodic insertion and removal (eg, every 4-6 hours) of a clean urinary catheter and can often be performed by the patient, is usually the initial treatment. CIC interrupts the extraluminal and intraluminal mechanisms of infection and, compared with the use of indwelling catheters, is associated with a significantly lower risk of CA-UTI. Indwelling catheters (changed monthly) can be considered if patients or their caregivers cannot perform CIC but are associated with an increased risk of UTI, stricture, and bladder spasm; suprapubic tube placement is another option.
Sleep Disorders
Delayed sleep phase syndrome, a circadian rhythm sleep-wake disorder characterized by sleep-onset insomnia and excessive morning sleepiness. Circadian rhythm sleep-wake disorders occur when the internal clock regulating sleep and wakefulness is misaligned with a person's desired sleep time or social/professional schedule.
Patients with delayed sleep phase syndrome commonly describe themselves as "night owls" and have chronic problems going to sleep at a societally accepted time (ie, prior to midnight). They sleep normally when allowed to set their own schedule. The onset of the condition occurs in adolescence and may respond to treatments such as light or behavioral therapy.
Advanced sleep phase syndrome is another circadian rhythm disorder characterized by the inability to stay awake in the evening (usually after 7:00 PM), making social functioning difficult. These patients frequently have early-morning insomnia due to their early bedtime.
Shift work sleep disorder involves a recurrent pattern of sleep interruption due to shift work, causing difficulty in initiating and maintaining sleep and daytime sleepiness. This disorder is due to a work schedule that is incongruent with a normal circadian clock.
PAC
Treatment is required only when symptoms cause distress or when there is supraventricular tachycardia. Even in asymptomatic patients, precipitating factors such as tobacco, alcohol, caffeine, and stress should be identified and avoided.
In the absence of obvious precipitants (eg, caffeine, alcohol), a transthoracic echocardiogram is useful in patients with documented PACs to assess for any cardiac/valvular structural and/or functional abnormality.
Patients with persistent symptomatic PACs can be managed with low-dose beta blockers.
Screening Test

Giant cell Arthritis
Giant cell arteritis - clinical manifestations
Systemic symptoms
Fever, fatigue, malaise, weight loss
Localized symptoms
Headaches: Located in temporal areas Jaw claudication: Most specific symptom of GCA PMR Arm claudication: Associated bruits in subclavian or axillary areas Aortic wall thickening or aneurysms CNS: TIAs/stroke, vertigo, hearing loss
Visual symptoms
Amaurosis fugax: Transient vision field defect progressing to monocular blindness AION: Most common ocular manifestation
Laboratory results
Normochromic anemia Elevated ESR & CRP Temporal artery biopsy
Treatment
PMR only: Low-dose oral glucocorticoids (eg, prednisone 10-20 mg daily) GCA: Intermediate- to high-dose oral glucocorticoids (eg, prednisone 40-60 mg daily) GCA with vision loss: Pulse high-dose IV glucocorticoids (eg, methylprednisolone 1,000 mg daily) for 3 days followed by intermediate- to high-dose oral glucocorticoids
AION = anterior ischemic optic neuropathy; CNS = central nervous system; CRP = C-reactive protein;ESR= erythrocyte sedimentation rate; GCA = giant cell arteritis; PMR = polymyalgia rheumatica; TIA = transient ischemic attack.
Vertigo
Common causes of vertigo
Ménière disease
Recurrent episodes lasting 20 minutes to several hours Sensorineural hearing loss Tinnitus and/or feeling of fullness in the ear
BPPV
Brief episodes triggered by head movement Dix-Hallpike maneuver causes nystagmus
Vestibular neuritis
Acute, single episode that can last days Often follows viral syndrome Abnormal head-thrust test
Migraine
Vertigo associated with headache or other migrainous phenomenon (eg, visual aura) Symptoms resolve completely between episodes
Brainstem/cerebellar stroke
Sudden-onset, persistent vertigo Usually other neurologic symptoms
Multiple Myeloma vs Waldenstrom
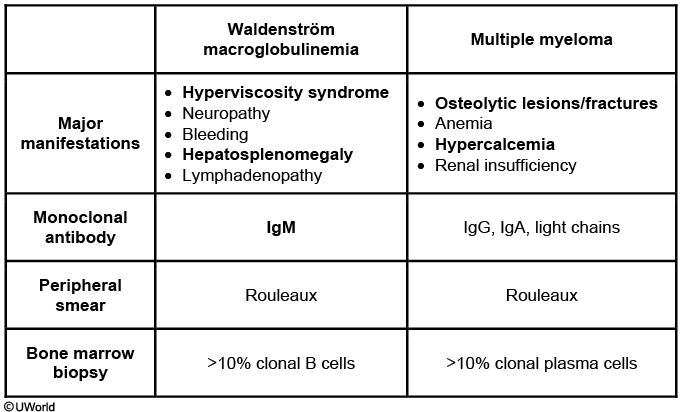
Patients with monoclonal gammopathy of undetermined significance (MGUS) also have M spikes, but they are most commonly due to IgA, IgG, or IgD (IgM is seen in 15% of cases). MGUS is marked by smaller M spikes (<3 g/dL), bone marrow biopsy with <10% monoclonal plasma cells, and, unlike this patient, no end-organ effects (no anemia, hepatosplenomegaly, lymphadenopathy, or systemic symptoms).
AFIb
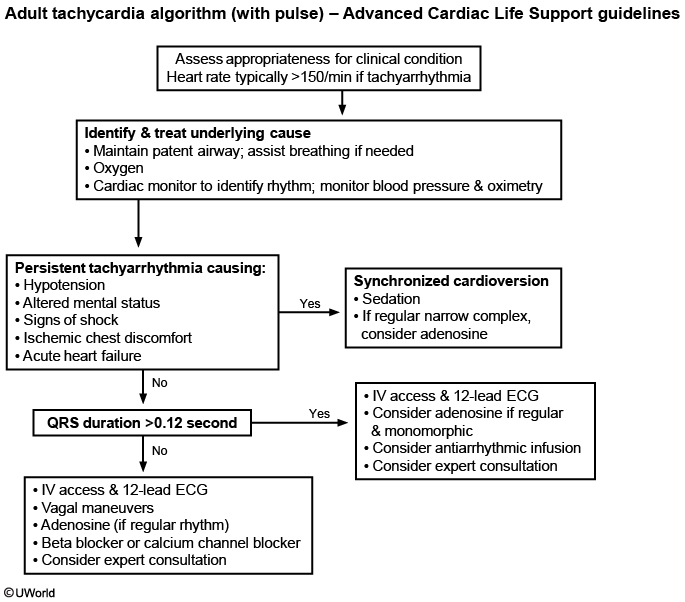
With cardioversion, energy delivery is synchronized to the QRS complex to minimize the likelihood of the shock occurring during repolarization, which can precipitate ventricular fibrillation.
By contrast, immediate defibrillation (as opposed to cardioversion) provides a high-energy shock at a random point in the cardiac cycle (unsynchronized shock) and is indicated in patients with ventricular fibrillation or pulseless ventricular tachycardia.
Hepatic Hydrothorax
Patients with cirrhosis and portal hypertension frequently have abdominal ascites and peripheral edema due to low albumin levels and abnormal extracellular fluid volume regulation. A small number of these patients may also develop hepatic hydrothorax, a pleural effusion not due to underlying cardiac or pulmonary abnormalities.
Hepatic hydrothorax generally results in transudative pleural effusions and is thought to occur due to small defects in the diaphragm. These defects permit peritoneal fluid to pass into the pleural space, which occurs much more commonly on the right side due to the less muscular hemidiaphragm. Patients have dyspnea, cough, pleuritic chest pain, and hypoxemia. Diagnosis involves documentation of the effusion (eg, chest x-ray) and testing to exclude other causes (eg, thoracentesis, echocardiogram).
Treatment involves salt restriction and diuretic administration. Therapeutic thoracentesis could be attempted in patients with prominent symptoms. Chest tube placement should be avoided as it can result in large-volume protein, fluid, and electrolyte losses as well as other severe complications (eg, renal failure). The definitive option for treatment is liver transplantation, although this may not be appropriate for all patients depending on other factors.
Cardiac Myxoma
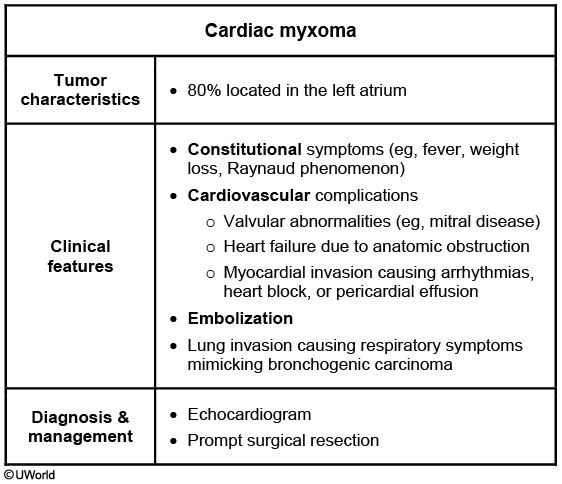
Myxomas are the most common benign primary cardiac tumors with approximately 80% located in the left atrium.
Left atrial myxomas can cause obstruction of blood flow across the mitral valve, mimicking mitral valve disease and producing early diastolic sound ("tumor plop"). Patients often present with fatigue, cough, dyspnea, orthopnea, pulmonary edema, or hemoptysis. Left atrial tumors can also cause systemic embolization (eg, transient ischemic attack, stroke, splenic infarcts). About 50% of patients report constitutional symptoms (due to overproduction of interleukin-6) such as fever, weight loss, or Raynaud phenomenon.
Although transesophageal echocardiography is the most sensitive test for diagnosis, transthoracic echocardiography is usually adequate. Once diagnosis is established, prompt surgical resection is recommended to avoid complications of embolization and risk of sudden death.
Heat Stroke vs Low volume
Heat stroke is categorized as exertional or nonexertional. Nonexertional heat stroke occurs in patients with chronic medical conditions, often because they cannot remove themselves from the inciting stimulus and/or have impaired thermoregulation due to medications and underlying illness. Exertional heat stroke occurs in otherwise healthy individuals undergoing conditioning in extreme heat and humidity. The body loses its ability to dissipate heat when the humidity is over 75% and the temperature is elevated.
This patient, who collapsed while running for military training in hot, humid weather, provides a typical history for exertional heat stroke. Signs and symptoms of heat stroke include temperature > 40°C (105°F), altered mental status, hypotension, tachycardia, and tachypnea. Patients may have moist or dry skin and often are not volume-depleted, depending on underlying medical conditions, original hydration status, and rapidity of onset.
A body temperature of 41°C (105.8°F) may cause rhabdomyolysis and organ system damage. Large blood on dipstick with no red blood cells by microscopy on urinalysis suggests rhabdomyolysis, the result of muscle breakdown. Under normal conditions, body temperature is typically maintained at 36-37.5°C (96.8-99.5°F) by dissipation of heat, primarily in the form of sweat. In heat stroke, the thermoregulatory center fails to dissipate heat at the rate necessary to maintain a euthermic state. Although inadequate fluid and salt replacement may contribute to heat stroke, it does not cause it.
Inadequate sodium and water replacement during physical activity can lead to heat exhaustion because of the body’s inability to maintain adequate cardiac output. Core body temperature is usually < 40°C (104°F). Significant CNS dysfunction (eg, seizure, delirium) is not present.
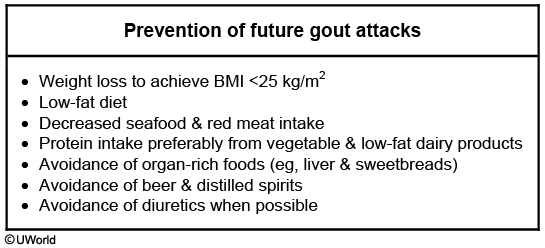
Gout Prevention
Endocarditis causes
Microbiology & clinical associations of infective endocarditis
Staphylococcus aureus
Prosthetic valves Intravascular catheters Implanted devices (eg, pacemaker/defibrillator) Intravenous drug users
Viridans group streptococci
Gingival manipulation Respiratory tract incision or biopsy
Staphylococcus epidermidis
Prosthetic valves Intravascular catheters Implanted devices
Enterococci
Nosocomial urinary tract infections
Streptococcus gallolyticus (S bovis)
Colon carcinoma Inflammatory bowel disease
Fungi (eg, Candida species)
Immunocompromised host Intravascular catheters Prolonged antibiotic therapy
Streptococcus sanguinis belongs to the viridans group of streptococci, which also includes S mitis, S oralis, S mutans, S sobrinus, and the S milleri group. IE with viridans group streptococci is commonly encountered after dental procedures involving manipulation of the gingival tissue or oral mucosa and procedures involving incision and biopsy of the respiratory tract.
Charcot joint

Septic Joints
Normal
Noninflammatory (eg, OA)
Inflammatory (eg, crystals, RA)
Septic joint
Appearance
Clear
Clear
Translucent or Opaque
Opaque
WBCs (mm3)
<200
200-2,000
2,000-100,000
50,000-150,000
PMNs
<25%
25%
Often >50%
>80%-90%
Gonococcal infection
Disseminated gonococcal infection:
Clinical presentation
Purulent monoarthritis (one sided) &/OR Triad of tenosynovitis, dermatitis (erythematous papules & pustules), asymmetric migratory polyarthralgias (arm, then ankle, then knee)
Diagnosis
Blood cultures (may be negative) Synovial fluid analysis: Inflammatory effusion with neutrophil predominance; Gram stain & culture or NAAT Culture or NAAT of urethra, cervix, pharynx, rectum
Treatment
Intravenous ceftriaxone, switch to oral (cefixime) when clinically improved Empiric azithromycin OR doxycycline for concomitant chlamydial infection Joint drainage for purulent arthritis
Chlamydia
Reactive arthritis is a type of seronegative spondyloarthropathy. Classic reactive arthritis consists of a triad of nongonococcal urethritis, asymmetric oligoarthritis and conjunctivitis. The arthritis often involves the knee and sacroiliac spine, which explains this patient’s back pain. In addition to the classic triad, mucocutaneous lesions and enthesitis (Achilles tendon pain) are common findings in reactive arthritis. Because not all symptoms are always present, there should be a high suspicion for reactive arthritis in the case of any asymmetric oligoarthritis associated with urethritis, conjunctivitis or mouth ulcers. Synovial fluid analysis is usually sterile. Nonsteroidal anti-inflammatory agents (NSAIDs) are the first line therapy during the acute phase of this condition.
Besides peripheral oligoarthritis, common manifestations include enthesitis, conjunctivitis, urethritis, oral ulcers, and keratoderma blennorrhagicum:

Lung
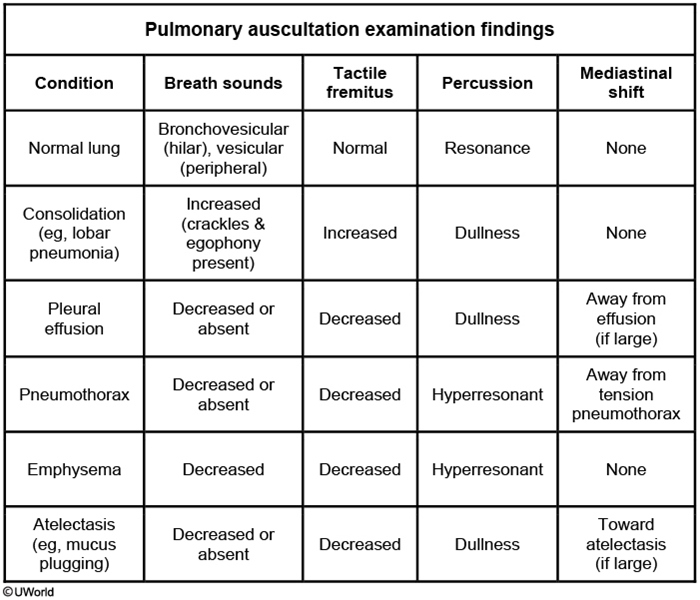
In general, sound travels faster in solids or liquids than in air, which results in increased intensity of breath sounds and increased tactile fremitus in patients with a consolidative process inside the lung (eg, bacterial pneumonia). However, if fluid (pleural effusion) or air (pneumothorax) are present just outside the lung in the thoracic cavity, they can act to insulate sounds and vibrations originating from the lung, which leads to decreased breath sounds and decreased tactile fremitus.
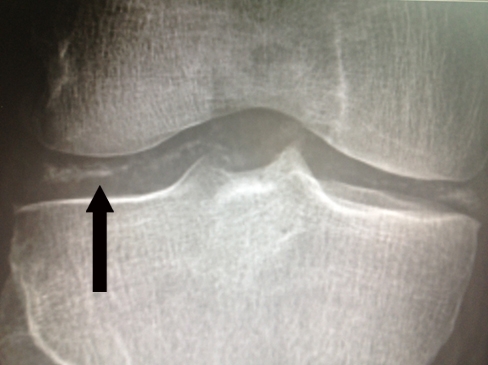
Pseudogout
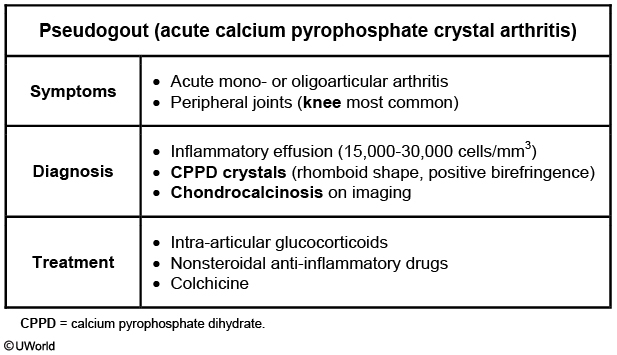
This patient has characteristic findings of acute calcium pyrophosphate dihydrate (CPPD) crystal arthritis (pseudogout), including onset at age >65, monoarticular arthritis, and chondrocalcinosis (calcification of articular cartilage). Synovial CPPD deposition can also cause a chronic inflammatory arthritis resembling rheumatoid arthritis and a noninflammatory degenerative process resembling osteoarthritis. Pseudogout commonly affects the knees and ankles, where it may be difficult to distinguish from urate gout, but it also frequently affects the large joints of the upper extremity and may involve multiple joints concurrently. Attacks of pseudogout often occur in the setting of trauma/overuse, surgery, or medical illness.
Associations: Patients with pseudogout should be evaluated for secondary causes such as hyperparathyroidism, hypothyroidism, and hemochromatosis. Hypercalcemia if hyperparathyroidism.
The finding of chondrocalcinosis in a joint with a typical acute inflammatory arthritis establishes a diagnosis of probable CPPD crystal arthritis. Synovial fluid analysis will show an inflammatory effusion (15,000-30,000 cells/mm3) along with rhomboid-shaped, weakly positively birefringent CPPD crystals. Arthrocentesis for synovial fluid analysis is advised to exclude urate gout (up to 50,000 cells/mm3, needle-shaped negatively birefringent urate crystals) and septic arthritis (>50,000 cells/mm3, visible organisms on Gram stain).
Trouseau Sign
unexplained superficial venous thrombosis at unusual sites (eg, arm, chest area)
red, itchy streaks; cord like veins
Vitiligo
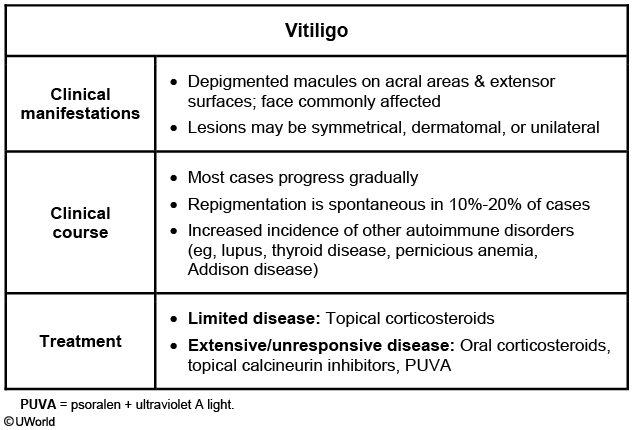
Vitiligo can occur as an isolated disorder but is often associated with other autoimmune conditions (eg, pernicious anemia, primary adrenal insufficiency, alopecia areata, rheumatoid arthritis, Sjogren syndrome). Autoimmune thyroid disease (eg, chronic lymphocytic [Hashimoto] thyroiditis, Graves disease) is especially common, and many experts advise patients with vitiligo be assessed for thyroid function.
Hypertrophic osteoarthropathy
Hypertrophic osteoarthropathy (HOA) is a condition where digital clubbing is accompanied by sudden-onset arthropathy, commonly affecting the wrist and hand joints. Hypertrophic pulmonary osteoarthropathy (HPOA) is a subset of HOA where the clubbing and arthropathy are attributable to underlying lung disease like lung cancer, tuberculosis, bronchiectasis, or emphysema. Given this patient's smoking history, lung cancer should be of particular concern.
Lower back pain
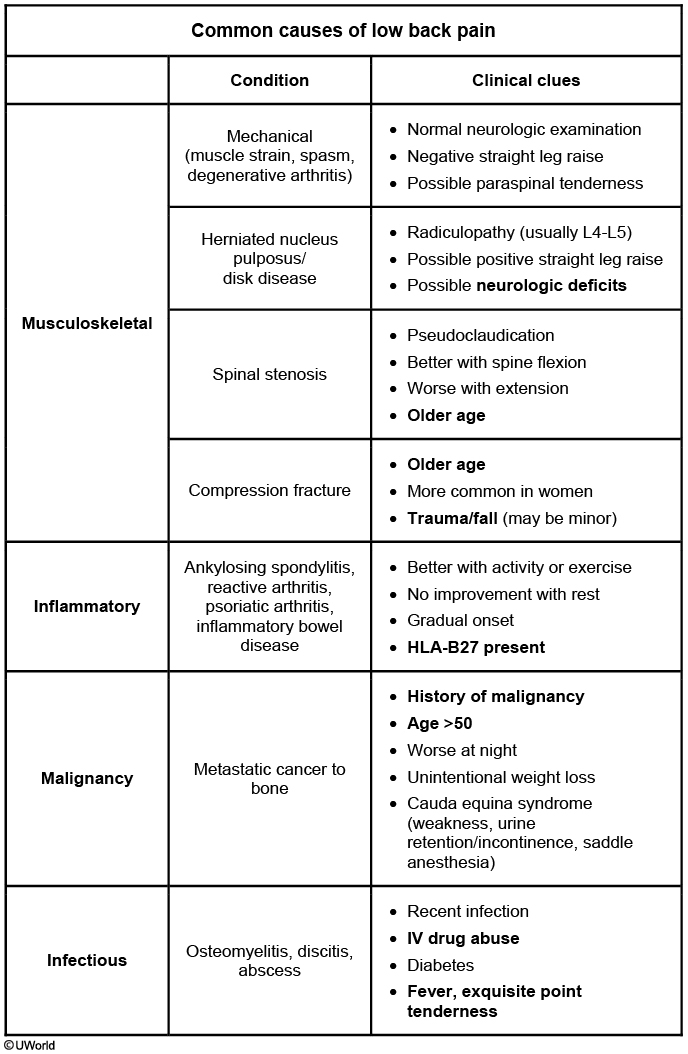
Bony metastases typically cause pain that is constant and worse at night, with point tenderness on examination. In contrast, the pain caused by degenerative disease is typically exacerbated by exercise and relieved by rest.
Vertebral osteomyelitis may cause chronic progressive pain with point tenderness over the affected vertebrae. However, it is typically accompanied by a low-grade fever and generally occurs in patients with recent overlying soft tissue infection or bacteremia. The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels are usually elevated.
Lumbar strain usually occurs acutely following twisting of the back while lifting heavy weights. It is typically exacerbated by activity and relieved by rest, and there is usually no point tenderness.
Iliac artery thrombosis can cause low back pain associated with claudication of the hip muscles and possibly impotence.
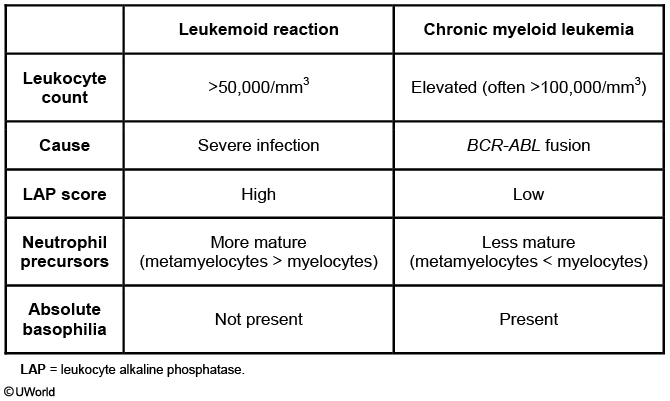
Leukemoid Reaction
Senile Purpura
This patient's skin fragility, ecchymosis, and normal laboratory studies (blood counts and coagulation studies) are consistent with senile purpura. Senile purpura (solar or actinic purpura) is a noninflammatory disorder that is most common in the elderly but can also be seen in middle-aged patients with extensive sunlight exposure. It is caused by loss of elastic fibers in perivascular connective tissue. Minor abrasions that would merely stretch the skin in younger patients can rupture superficial blood vessels in the elderly. The subsequent extravasation of blood leads to ecchymosis over vulnerable areas, such as the dorsum of the hands and forearms. Patients can have residual brownish discoloration from hemosiderin deposition. The incidence and severity are also increased in patients taking anticoagulants, corticosteroids, or nonsteroidal anti-inflammatory drugs.
Senile purpura is usually not a dangerous condition and requires no further investigation. However, many older patients with severe skin fragility may require careful wound care measures following even minor lacerations.

Polymyalgia Rheumatica
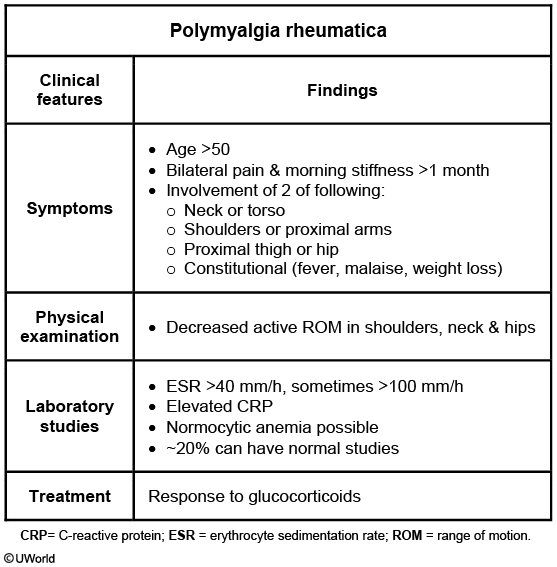
Morning stiffness lasting >1 hour
In PMR, the physical examination is frequently unremarkable with patients having no focal tenderness or pain with active or passive range of motion. Signs of inflammation in the joints are absent. When asked to identify the location of their pain, patients typically indicate the soft tissues and not the joints.
OTE
This patient's presentation is most consistent with malignant otitis externa (MOE), which is a severe infection typically seen in elderly diabetic patients that is most commonly caused by Pseudomonas aeruginosa. Patients typically present with ear pain and ear drainage that is not responsive to topical medications. The granulation tissue seen within the ear canal in this patient is a characteristic manifestation of MOE, and her history of poorly controlled diabetes is also a diagnostic clue. Progression of the infection can lead to osteomyelitis of the skull base and cranial nerve damage. This patient's facial drooping, which is likely causing food to drop out of her mouth, is a result of damage to the left facial nerve. CT or MRI can be used to confirm the diagnosis.
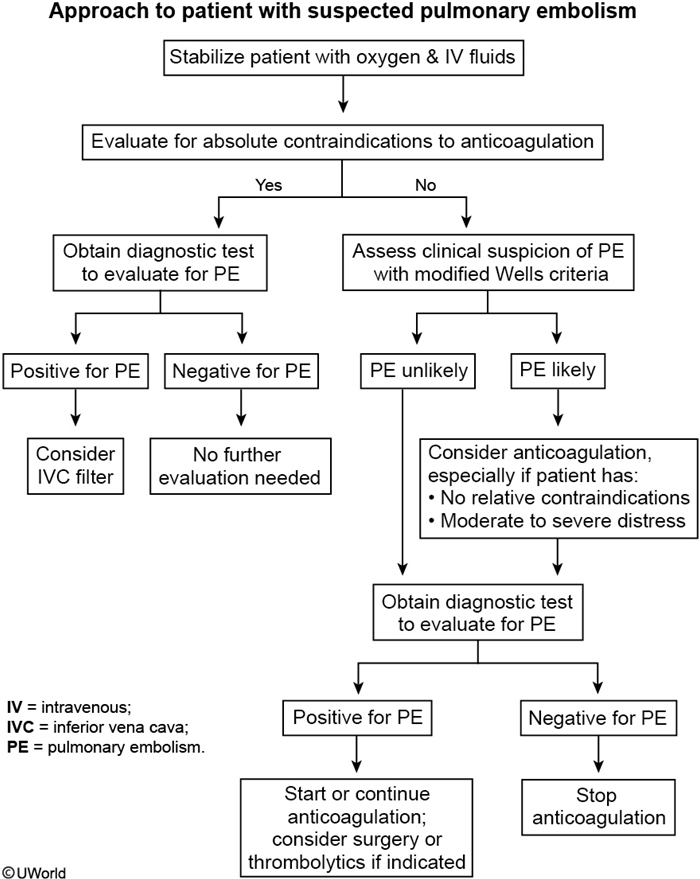
PE
Osteomalacia
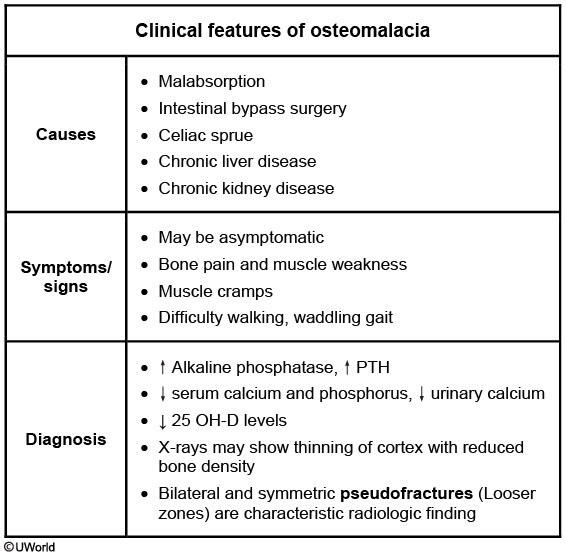
This patient's presentation suggests osteomalacia. Vitamin D deficiency most commonly causes osteomalacia and can be due to malabsorption, intestinal bypass surgery, celiac sprue, or chronic liver or kidney disease. Patients can be asymptomatic or present with bone pain, muscle weakness or cramps, and difficulty walking.
Cystoscopy
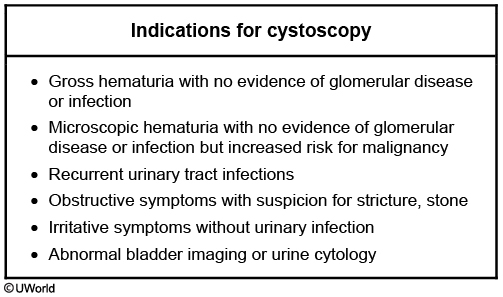
even in BPH with hematuria
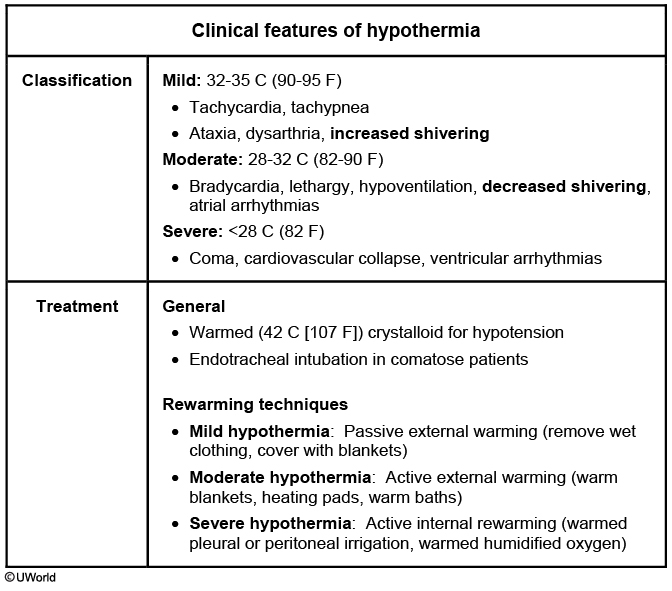
Hypothermia
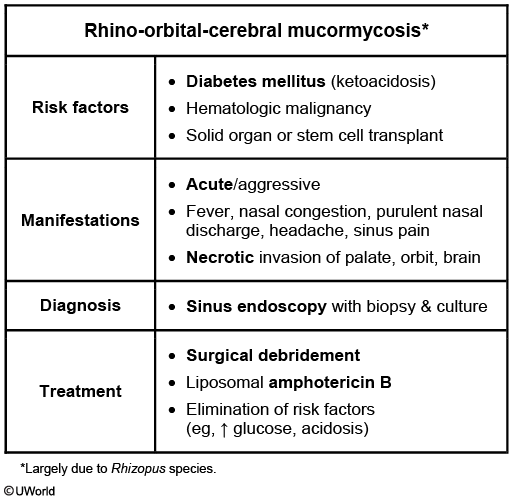
Mucormycosis
Gastrinoma
PTU agranulocytosis
The antithyroid drugs propylthiouracil (PTU) and methimazole (MMI) are associated with a number of minor, as well as potentially life-threatening, side effects. Agranulocytosis is the most feared side effect, and is seen in approximately 0.3% of patients treated with antithyroid drugs. It is caused by immune destruction of granulocytes, and most cases occur within 90 days of treatment. Routine monitoring of the granulocyte count is not cost effective and not advocated. Current recommendations state that once the patient complains of fever and sore throat, the antithyroid drug should be discontinued promptly and the WBC count measured. A total WBC count less than 1,000/cubic mm warrants permanent discontinuation of the drug. If the total WBC count is more than 1,500 per cubic mm, antithyroid drug toxicity is unlikely to be the cause of the sore throat and fever.
Lyme
no pregnant: doxy
pregnant: amoxicillin
children < 8 yo: amoxicillin
De Quervain
The patient described most likely has De Quervain tenosynovitis, a condition that classically affects new mothers who hold their infants with the thumb outstretched (abducted / extended). This condition is caused by inflammation of the abductor pollicis longus and extensor pollicis brevis tendons as they pass through a fibrous sheath at the radial styloid process. Tenderness can typically be elicited with direct palpation of the radial side of the wrist at the base of the hand. Additionally, the Finkelstein test, which is conducted by passively stretching the affected tendons by grasping the flexed thumb into the palm with the fingers, elicits pain.
Fibromuscular Dysplasia
FMD is a systemic noninflammatory disease that typically affects the renal and internal carotid arteries and leads to arterial stenosis, aneurysm, or dissection. Less commonly, the vertebral, iliac, or mesenteric arteries can be affected.
In adults, approximately 90% of FMD cases occur in women. Recurrent headache caused by carotid artery stenosis or aneurysm is the most common presenting symptom. Pulsatile tinnitus, neck pain, or flank pain are also common, and symptoms of transient ischemic attack (eg, focal weakness, vision loss) may occur. Hypertension results from renal artery stenosis (RAS) leading to secondary hyperaldosteronism. An abdominal bruit may be present. In young patients, a subauricular systolic bruit is highly suggestive of FMD as carotid atherosclerosis should not be present. Even in older patients, such a bruit suggests FMD as the subauricular location indicates involvement of the internal carotid artery, which, in contrast with the carotid bulb, is not commonly affected by atherosclerosis.
Diagnosis of FMD is typically made by vascular imaging (eg, duplex ultrasonography, CT or magnetic resonance angiography). For patients with hypertension, treatment involves antihypertensive medication (eg, ACE inhibitor) and definitive management of RAS with either percutaneous transluminal angioplasty or surgery.
Sympathetic ophthalmia
Sympathetic ophthalmia is also known as "spared eye injury." It is characterized by an immune-mediated inflammation of one eye (the sympathetic eye) after a penetrating injury to the other eye. The typical manifestation is anterior uveitis, but panuveitis, papillary edema, and blindness may develop. The pathophysiological mechanism is believed to be the uncovering of 'hidden' antigens. Some antigens contained within the eye are protected from immunologic recognition by natural barriers. Breaking these barriers results in the uncovering of 'hidden' antigens. An immune response against these antigens can involve autoantibodies as well as a cell-mediated reaction.
case: A 30-year-old man is concerned about "floating spots" and blurred vision in his right eye. He had a penetrating injury to his left eye several weeks ago, which eventually led to vision loss in that eye. Inspection reveals a moderate perilimbal flush. What is the most probable cause of this patient's condition?
Cutaneous Larva Migrans
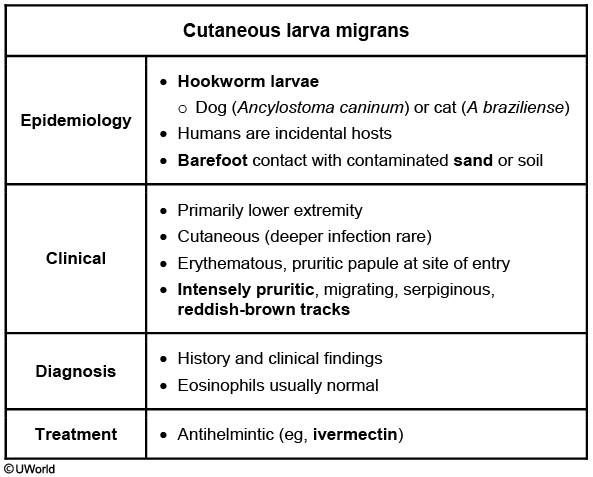
Cutaneous larva migrans (CLM) is a creeping cutaneous eruption caused by dog (Ancylostoma caninum) or cat (A braziliense) hookworm larvae. Most infections are acquired from walking barefoot on contaminated sand (beaches) or soil. Humans are incidental hosts, and larvae are typically unable to penetrate the dermal basement membrane. As a result, cutaneous infection without deeper penetration is the norm.
Most infections occur in the lower extremities (70%), and symptoms usually start with a pruritic, erythematous papule at the site of larvae penetration (which may go unnoticed). Within a few days, patients develop symptoms related to larvae migration: intensely pruritic, serpiginous, reddish-brown cutaneous tracks. Although most cases resolve spontaneously after a few weeks, antihelmintics (eg, ivermectin) are usually given to aid clearance.

Rabies
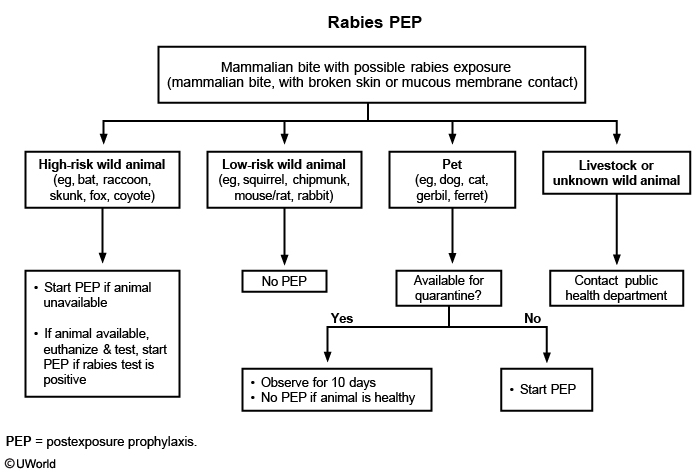
Rabies usually presents with motor weakness, paresthesias, and encephalitis that progress to coma and death. Rabies is transmitted following a bite from an infected mammal. In developing countries, dogs account for >90% of transmission due to inadequate rabies control programs. In contrast, rabies in domesticated animals is very rare in the United States due to effective rabies vaccination. Most cases of rabies in the United States are due to bites from wild animals (eg, bats, raccoons, foxes, skunks).
Postexposure prophylaxis (PEP) consists of a series of rabies immunizations as well as rabies immune globulin. However, not all patients require PEP:
Patients exposed to high-risk wild animals (eg, bats, raccoons, foxes, skunks) should receive PEP for rabies if the animal is unavailable for testing. In particular, bat bites can go unrecognized, so PEP is recommended following direct exposure to bats (unless the patient is constantly aware of the bats and is certain a bite was not inflicted). In the rare situation that the high-risk wild animal is available for testing, PEP can be withheld until the animal is euthanized, its brain has been tested for rabies, and the test results are available.
Patients bitten by domestic animals (ie, pets) in the United States do not require PEP if the pet is available for testing. The incubation period for rabies is usually 1-3 months, but animals that are contagious (ie, have rabies virus in their saliva) will be symptomatic 5-10 days after becoming contagious. Therefore, pets available for quarantine can be observed for 10 days for signs of rabies. However, if the pet is unavailable for quarantine (or is symptomatic), PEP should be administered.
Patients bitten by low-risk animals (eg, squirrels, chipmunks) do not need PEP.
Cholesterol Emboli
His pancreatitis is likely due to cholesterol emboli. Patients with risk factors for aortic atherosclerosis (eg, hypercholesterolemia, diabetes, peripheral vascular disease) who undergo cardiac catheterization or a vascular procedure are at increased risk for cholesterol emboli as a result of vascular manipulation. These emboli can occlude blood vessels and cause the following:
Skin manifestations: Livedo reticularis (reticulated, mottled, discolored skin), blue toe syndrome
Kidney manifestations: Acute kidney injury
Gastrointestinal manifestations: Pancreatitis, mesenteric ischemia

treat the pancreatitis via supportive care
Paget disease
Paget
Clinical features
Most patients are asymptomatic Bone pain & deformity Skull: Headache, hearing loss Spine: Spinal stenosis, radiculopathy Long bones: Bowing, fracture, arthritis of adjacent joints Giant cell tumor, osteosarcoma
Pathogenesis
Osteoclast dysfunction Increased bone turnover
Laboratory testing
Elevated alkaline phosphatase Elevated bone turnover markers (eg, PINP, urine hydroxyproline) Calcium & phosphorus are usually normal
Imaging
X-ray: Osteolytic or mixed lytic/sclerotic lesions Bone scan: Focal increase in uptake
Treatment
Bisphosphonates
The most common cause of an isolated, asymptomatic elevation of alkaline phosphatase in an elderly patient is Paget disease of bone (osteitis deformans). Paget disease is frequently discovered incidentally on routine blood tests, and alkaline phosphatase levels can be strikingly elevated, often >10 times the upper limit of normal. Fractionation of alkaline phosphatase would show a predominance of bone rather than liver isoenzymes.
Colon Cancer Screening
Colon cancer screening in patients at increased risk
Indication
Colonoscopy recommendations
Family history of adenomatous polyps or CRC 1 first-degree relative age less than 60 2 or more first-degree relatives at any age
Age 40 or 10 years before the age of diagnosis in affected relative *Repeat every 5 years
Inflammatory bowel disease Ulcerative colitis Crohn disease with colonic involvement
8-10 years postdiagnosis (12-15 years if disease only in left colon) Repeat every 1-3 years
Classic familial adenomatous polyposis
Age 10-12 Repeat annually
HNPCC (Lynch syndrome)
Age 20-25 Repeat every 1-2 years
CRC screening with colonoscopy and mucosal sampling should be offered to patients with ulcerative colitis, beginning 8 years after the initial diagnosis (Choices D and E) (patients with disease limited to the rectum and left colon may begin 12-15 years post diagnosis). Repeat colonoscopy should be performed every 1-2 years thereafter.
A screening colonoscopy interval of 5 years is appropriate for patients without inflammatory bowel disease who are found to have 1 or 2 small adenomatous polyps. Five years is also an appropriate interval for patients with a first-degree family history of CRC or adenomatous polyps.
CVID
Common variable immunodeficiency
Manifestations
Recurrent respiratory (eg, pneumonia, sinusitis, otitis) & GI (eg, Salmonella, Campylobacter) infections Autoimmune disease (eg, RA, thyroid disease) Chronic lung disease (eg, bronchiectasis) GI disorders (eg, chronic diarrhea, IBD-like conditions, bloody diarrhea)
Diagnosis
↓↓ IgG, ↓ IgA/IgM No response to vaccination
Management
Immunoglobulin replacement therapy
This patient with evidence of acute pneumonia (cough, shortness of breath, leukocytosis, right lower lobe infiltrate) and recent history of recurrent pneumonia, sinusitis, and bloody diarrhea likely has common variable immunodeficiency (CVID). CVID is a collective diagnosis that includes a number of genetic defects resulting in impaired B cell differentiation and hypogammaglobulinemia.
CVID is one of the most common primary immunodeficiencies in adults and is characterized mainly by increased susceptibility to bacterial infection. Recurrent respiratory infections (eg, pneumonia, sinusitis, otitis) and gastrointestinal infections (eg, Salmonella, Campylobacter) are common, and the latter may lead to episodes of bloody diarrhea. Chronic giardiasis may occur, but opportunistic infections (eg, Candida, Pneumocystis jirovecii) are rare. Other characteristics of CVID include concomitant autoimmune disease (eg, hemolytic anemia, rheumatoid arthritis, pernicious anemia), inflammatory bowel-like disease, granuloma development, and increased risk for non-Hodgkin lymphoma. Enteropathy (eg, sprue-like illness) is common, and affected patients may present with malabsorption and weight loss.
Most cases of CVID are due to sporadic mutation, and family history of the disease is typically absent (as in this patient). The majority of patients are diagnosed in adulthood (age 20-45) due to a combination of variable presentation and diagnostic delay. Diagnosis is made by quantitative measurement of immunoglobulin levels (significantly reduced serum IgG with low levels of IgA and/or IgM) as well as by markedly reduced or absent immune response to vaccination.
Cancer related cachexia
Cancer-related anorexia/cachexia syndrome (CACS) is a hypercatabolic state associated with weight loss, anorexia, and an excessive reduction in skeletal muscle. Weight loss is multifactorial and thought to be a result of systemic inflammation in addition to caloric reduction. Nutritional counseling and supplementation with enteral or parenteral feeding do little to reverse CACS. Pharmacologic intervention with progesterone analogues (eg, megestrol acetate) or corticosteroids is effective at increasing appetite, causing weight gain, and improving well-being. In patients with longer life expectancies, progesterone analogues are preferred over corticosteroids due to their decreased incidence of side effects.
Although synthetic cannabinoids like dronabinol are useful in advanced HIV cachexia, large studies have demonstrated little benefit in anorexia and weight gain in CACS. The reasons for this remain unclear, but the cachexia in HIV may operate somewhat differently than that due to cancer. Although cannabinoids are mildly better than placebo in cancer-related cachexia, progesterone analogues are far superior.
Pemphigoid Vulgaris
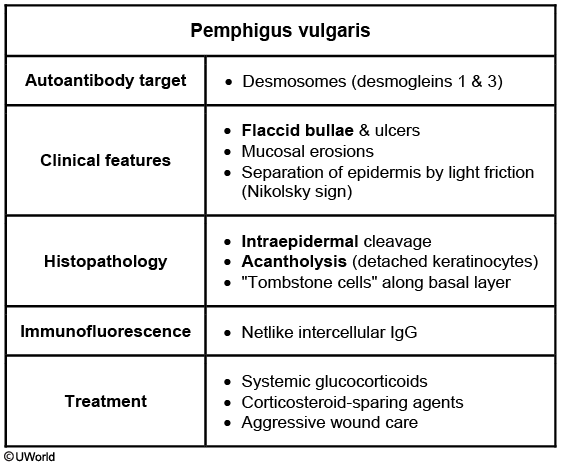


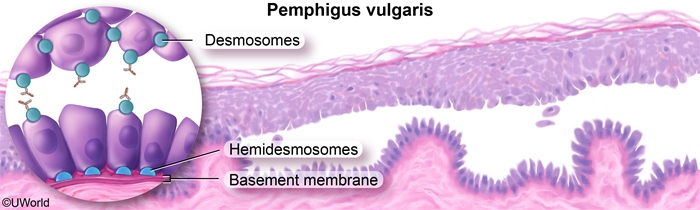
This patient has typical features of pemphigus vulgaris (PV), including painful, flaccid bullae, mucosal erosions, and separation of epidermis from dermis by light friction (Nikolsky sign). The roof of the bullous lesions is fragile and rapidly desquamates, leaving raw ulcers. PV is an autoimmune disorder caused by antibodies directed against desmogleins 1 and 3, which are components of desmosomes normally involved in adherence between epidermal keratinocytes.
Light microscopy of a biopsy specimen from a lesion edge shows intraepithelial cleavage with detached keratinocytes (acantholysis). Because the attachment of keratinocytes to the basement membrane is mediated by hemidesmosomes (which are immunologically distinct from desmosomes), a single cell layer remains along the basement membrane with an appearance described as a "row of tombstones." Immunofluorescence microscopy reveals IgG and C3 deposits in a netlike or "chicken wire" pattern. Serology for antibodies to desmoglein 1 and 3 can further support the diagnosis.
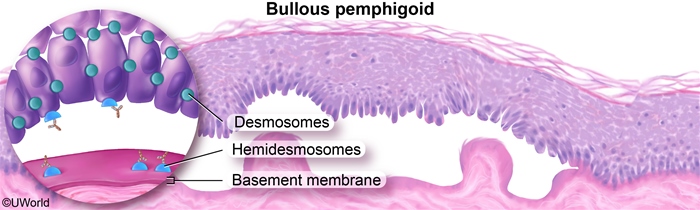
Bullous pemphigoid is an autoimmune blistering disease that causes pruritic, tense bullae in the flexural surfaces, groin, and axilla. Mucosal lesions occur in only a minority of patients. Biopsy shows subepidermal cleavage, with linear IgG deposits at the basement membrane on immunofluorescence studies.
Bullous Pemphigoid
Bullous pemphigoid is an autoimmune disorder characterized by severe pruritus and tense bullae on an erythematous base. It is most common in patients age >65 and has an increased incidence in those with malignancy or neurological disorders (eg, Parkinson disease, multiple sclerosis). The extent of involvement may range from just a few lesions to hundreds covering a large portion of the body, although mucous membrane involvement occurs only in a minority of patients. A pre-bullous prodrome is common and can present as urticarial or eczematous lesions.
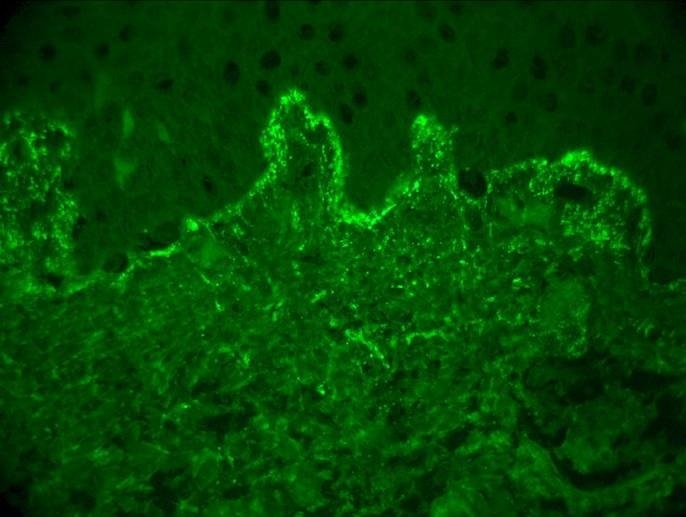
Bullous pemphigoid is caused by IgG autoantibodies against the hemidesmosome and basement membrane zone. Antibody binding activates complement and inflammatory mediators, and the resultant inflammation leads to blister formation. The diagnosis is made by skin biopsy; light microscopy shows subepidermal cleavage, and direct immunofluorescence microscopy shows linear IgG and C3 deposits along the basement membrane. First-line treatment for bullous pemphigoid is a high-potency topical glucocorticoid (eg, clobetasol), which is effective even for extensive disease. Systemic glucocorticoids are not more effective and are associated with an increased incidence of treatment-related complications, but these can be used when topical agents are not practical.

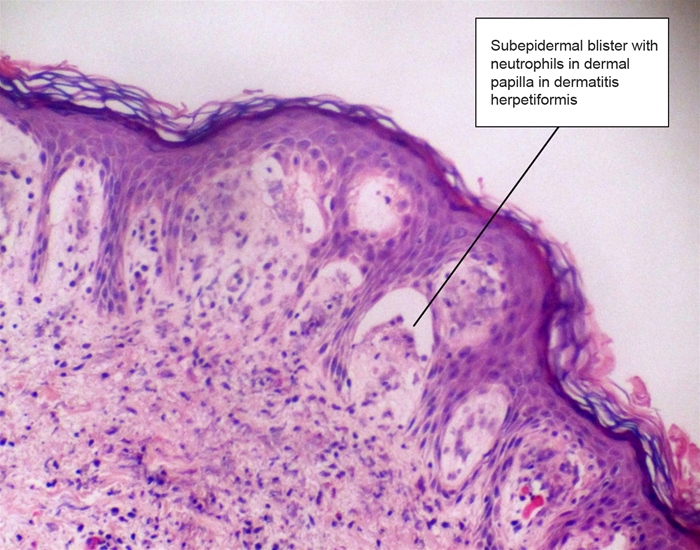
Dermatitis herpetiformis
Dermatitis herpetiformis is characterized by grouped pruritic vesicles on the buttocks and extensor surfaces of the limbs. It represents an autoimmune dermal reaction due to dietary gluten, and biopsy shows microabscesses at the tips of the dermal papillae with deposits of IgA antibodies against epidermal transglutaminase in the dermis. Treatment includes oral dapsone and elimination of dietary gluten.

PSA screening
Due to the current controversy, screening decisions are left up to the individual and the physician and best determined with a discussion of the risks and benefits of screening with PSA and/or digital rectal examination.
Herpes vs Cox
Coxsackievirus causes hand-foot-and-mouth disease and usually manifests with oral lesions and a bilateral macular, maculopapular, or vesicular rash of the hands and feet. This patient with a localized, unilateral rash on a small section of the hand is unlikely to have coxsackievirus.
cox:

herpes:

Autoimmune adrenitis
The most common cause of primary adrenal insufficiency in developed countries is autoimmune adrenalitis (responsible for more than 80% of patients with primary adrenal cortical insufficiency). The presence of autoantibodies against one or more adrenal steroidogenic enzymes has been postulated to be a cause of autoimmune adrenal destruction. In addition, approximately 50% of patients with autoimmune primary adrenal insufficiency (Addison's disease) have autoimmune diseases involving other endocrine glands, such as the thyroid, parathyroid, and ovaries. Other non-endocrine autoimmune conditions, such as pernicious anemia and vitiligo, are also common.
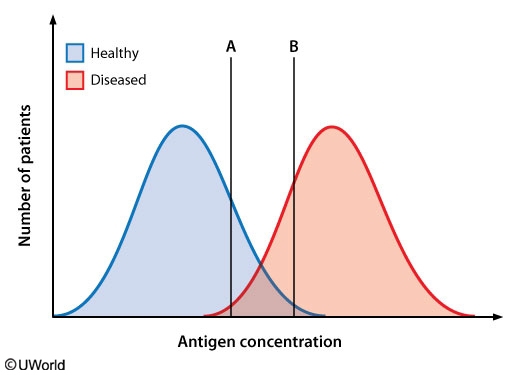
Sensitivity
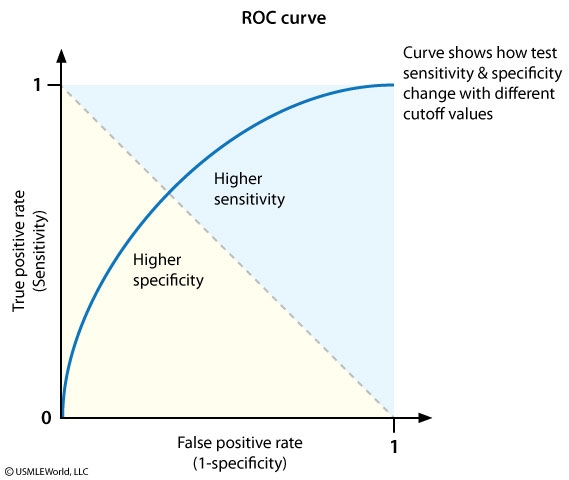
At any particular cutoff point, there is a trade-off between sensitivity and specificity. Changing the cutoff point to increase the number of patients with the disease who test positive will increase the true-positive rate (which is directly proportional to sensitivity), but it will also increase the number of patients without the disease who test positive (increasing the false-positive rate, which is inversely proportional to specificity). As a result, specificity usually decreases as sensitivity increases and vice-versa.
PPV
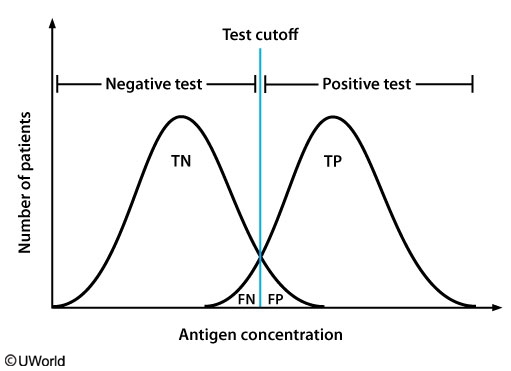
Positive predictive value (PPV) - The number of patients correctly testing positive divided by the total number of patients testing positive (TP / [TP + FP]). Higher PPV means that a positive test result is more likely to be true. It is related to both sensitivity and specificity, but also depends on disease prevalence since it is calculated using both diseased patients (TPs) and healthy patients (FPs).
Negative predictive value (NPV) - The number of patients correctly testing negative divided by the total number of patients testing negative (TN / [TN + FN]). Higher NPV means that a negative test result is more likely to be true. It is related to both sensitivity and specificity, but also depends on disease prevalence since it is calculated using both diseased patients (FNs) and healthy patients (TNs).
In this example, disease prevalence is approximately 50% since the graph shows that the diseased and healthy groups contain an equal amount of patients. Moving the cutoff point from B to A will cause more patients with the disease to test positive (more TPs) and at the same time cause more patients without the disease to test positive (more FPs). (In this example, the increase in TPs happens to be the same as the increase in FPs). As a result, PPV will decrease because PPV = (TP / [TP + FP]).
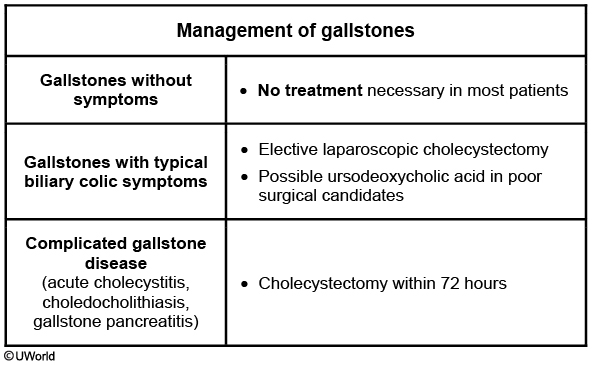
Gallstones
AAA
nonsmoker: no screening
smoker: 65-75, use US
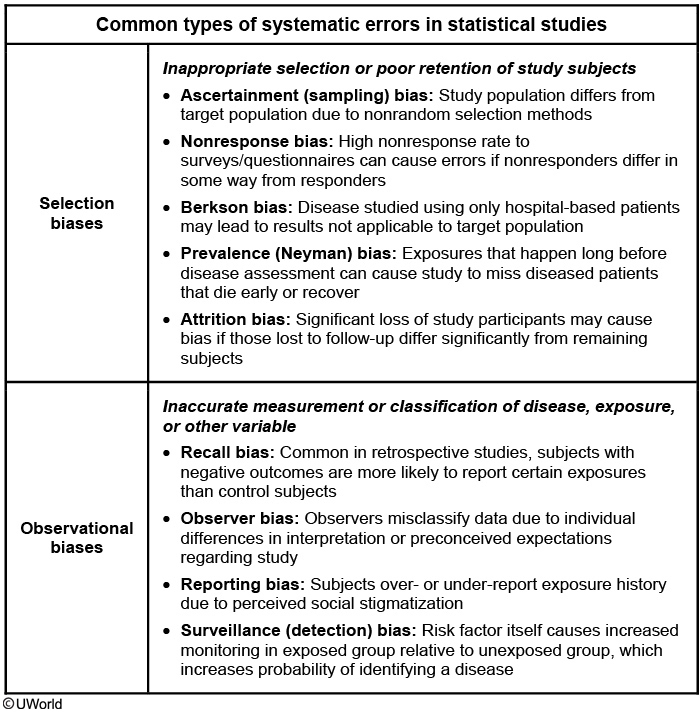
Bias
Hawthorne: subjects change behavior because they are being observed
Myopathy
Myopathy
Disorder
Clinical features
ESR
CK
Glucocorticoid-induced myopathy
Progressive proximal muscle weakness & atrophy without pain or tenderness Lower extremity muscles are more involved
Normal
Normal
Polymyalgia rheumatica
Muscle pain & stiffness in the shoulder & pelvic girdle Tenderness with decreased range of motion at shoulder, neck & hip Responds rapidly to glucocorticoids
↑
Normal
Inflammatory myopathies
Muscle pain, tenderness & proximal muscle weakness Skin rash & inflammatory arthritis may be present
↑
↑
Statin-induced myopathy
Prominent muscle pain/tenderness with or without weakness Rare rhabdomyolysis
Normal
↑
Hypothyroid myopathy
Muscle pain, cramps & weakness involving the proximal muscles Delayed tendon reflexes & myoedema Occasional rhabdomyolysis Features of hypothyroidism are present
Normal
↑
Legionella
sputum shows many neutrophils but no organisms.,
Vaccines
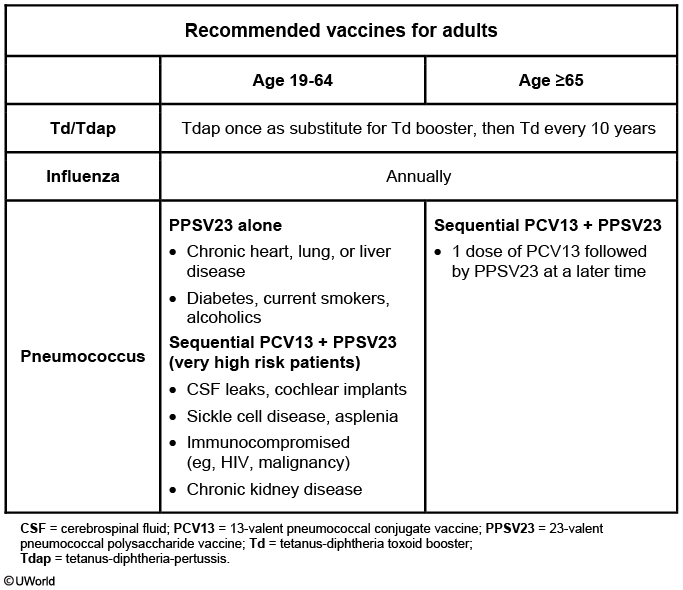
The 13-valent pneumococcal conjugate vaccine (PCV13) is recommended for all adults age >65 followed by the 23-valent pneumococcal polysaccharide vaccine (PPSV23) at least 6-12 months later. Sequential PCV13 and PPSV23 are also recommended for adults age <65 with certain very high risk comorbidities (eg, cerebrospinal fluid leaks, sickle cell disease, cochlear implants, congenital or acquired asplenia, immunocompromised patients). PPSV23 alone is recommended as a one-time vaccine for adults age <65 who are current smokers or have other chronic medical conditions, including heart or lung disease, diabetes, and chronic liver disease (Choices A and B). They should then receive sequential PCV13 and PPSV23 at age 65.
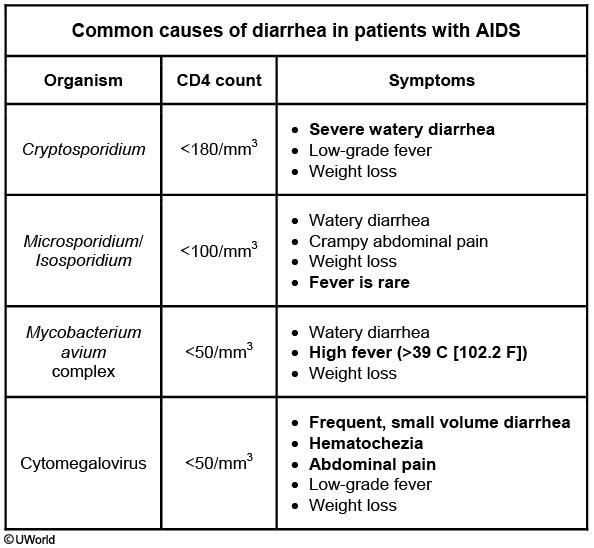
HIV Diarrhea
Sarcoidosis
sarcoidosis
Epidemiology
Young adults African Americans
Clinical
Constitutional symptoms Cough, dyspnea & chest pain Extrapulmonary findings Skin lesions Anterior/posterior uveitis Löfgren syndrome
Imaging
Bilateral hilar adenopathy Pulmonary reticular infiltrates
Laboratory
Hypercalcemia/hypercalciuria Elevated serum ACE level
Pathology
Biopsy showing noncaseating granulomas that stain negative for fungi & acid-fast bacilli
The initial workup includes basic laboratory tests (complete blood count, liver function, renal function), antistreptolysin-O antibodies, and TB skin testing. In addition, a chest x-ray should be obtained to assess for findings consistent with sarcoidosis (eg, bilateral hilar lymphadenopathy, reticular opacities) or with TB (unlikely in the absence of symptoms).
Biopsy only for atypical nodes
Hypercalcemia and Immobilization
Hypercalcemia of immobilization is likely due to increased osteoclastic bone resorption. The risk is increased in patients with a pre-existing high rate of bone turnover (eg, younger individuals, Paget disease). The onset of hypercalcemia is usually around 4 weeks after immobilization, although patients with chronic renal insufficiency may develop hypercalcemia in as little as 3 days.
The onset of hypercalcemia due to immobilization is often insidious, and the presenting symptoms can be nonspecific. Bisphosphonates inhibit osteoclastic bone resorption and are effective in treating hypercalcemia of immobilization and reducing the associated bone loss.
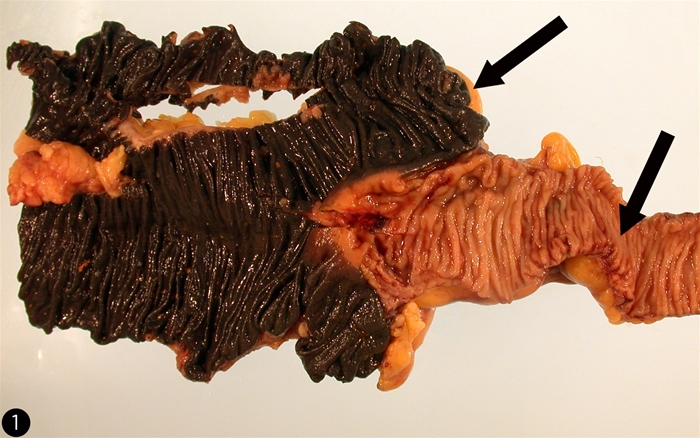
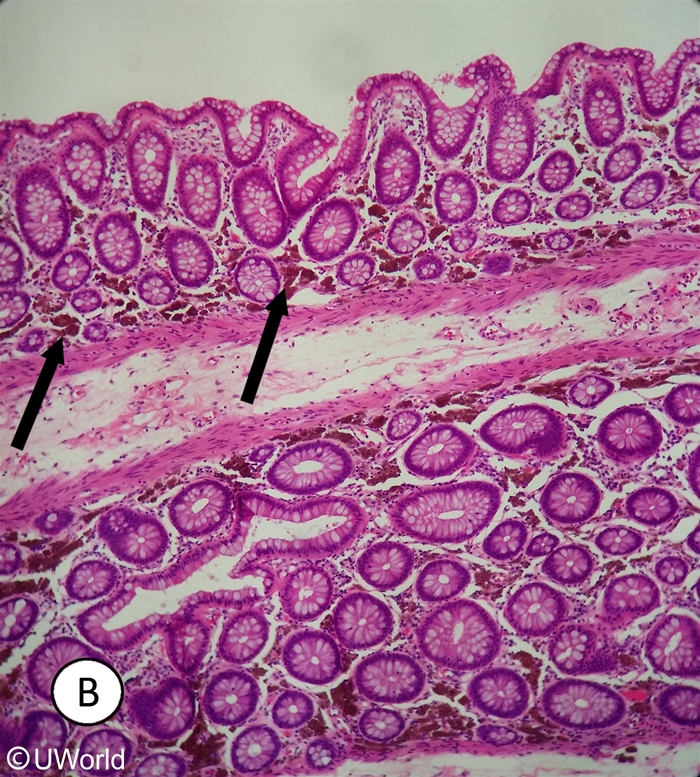
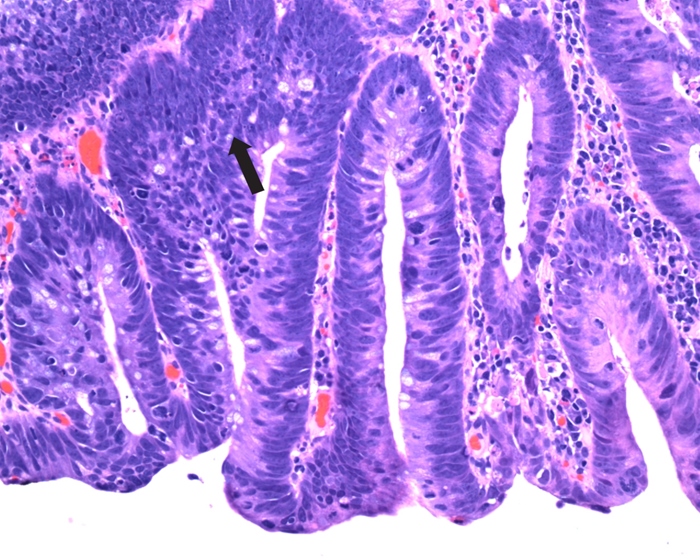
Melanosis Coli
Melanosis coli can develop within a few months of the onset of regular laxative ingestion and can similarly disappear if laxative use is discontinued. If melanosis coli is not seen on gross inspection, histological examination may demonstrate the pigment in the macrophages of the lamina propria.
Diagnosis is supported by a positive stool screen for diphenolic (eg, bisacodyl) or polyethylene-containing laxatives.
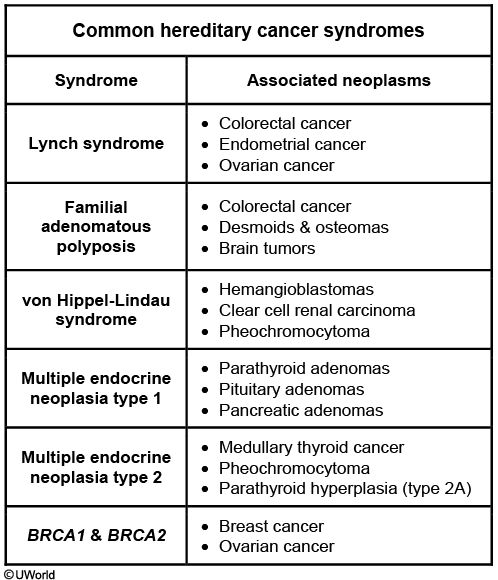
Lynch
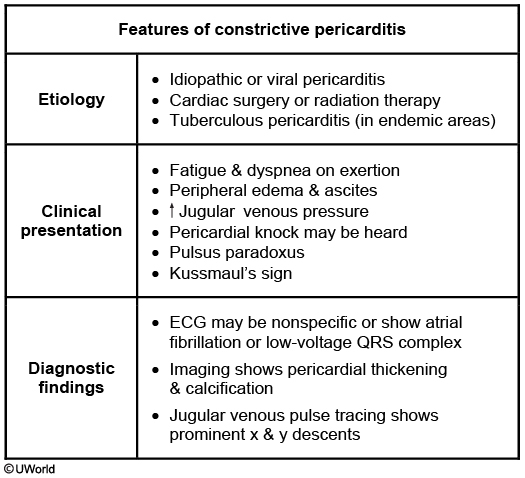
Constrictive Percarditis
Uremia induced platelet dysfunction
The pathogenesis is multifactorial, but the major defect involves platelet-vessel wall and platelet-platelet interaction. Several uremic toxins have been implicated in the pathogenesis of platelet dysfunction seen in chronic renal failure (CRF), the chief among which is guanidinosuccinic acid. Activated partial thromboplastin (aPTT), prothrombin (PT), and thrombin times (TT) are generally normal. Bleeding time (BT) is reflective of platelet function, and is usually prolonged. The platelet count is normal, but there is platelet dysfunction that causes bleeding.
A number of agents such as desmopressin (DDAVP), cryoprecipitate, and conjugated estrogens have been used to correct the coagulopathy in uremic patients. DDAVP increases the release of factor VIII:von Willebrand factor multimers from endothelial storage sites.
Running Injuries

Plantar fasciitis causes focal pain in the plantar area of the rearfoot. It usually worsens with the first steps in the morning, decreases with activity during the day, and often worsens again later in the day with prolonged weight bearing. Examination will show point tenderness at the plantar surface of the heel.
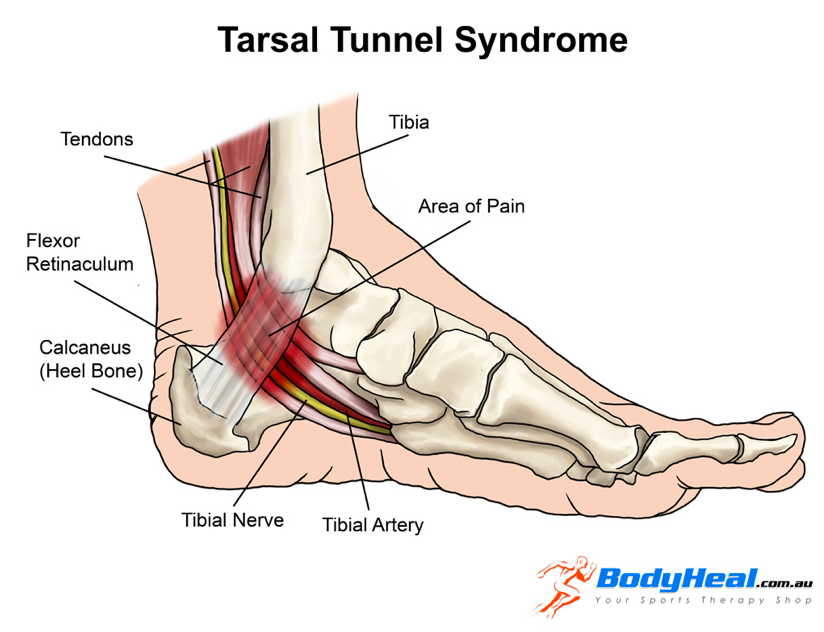
Tarsal tunnel syndrome is due to compression of the tibial nerve as it passes through the ankle and is usually caused by a fracture of the bones around the ankle. Patients have burning, numbness, and aching of the distal plantar surface of the foot or toes that sometimes radiate up to the calf.
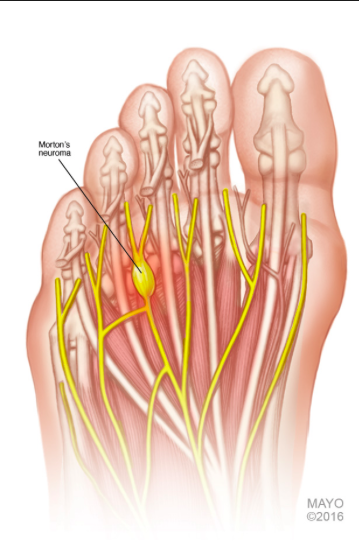
Morton Neuroma
This patient's presentation suggests an interdigital (Morton) neuroma, which commonly occurs in runners. The disorder is not a true neuroma but is a mechanically induced neuropathic degeneration of the interdigital nerves that causes numbness, aching, and burning in the distal forefoot from the metatarsal heads to the third and fourth toes. The symptoms are worsened by walking on hard surfaces and wearing tight or high-heeled shoes.
The diagnosis of Morton neuroma is primarily made clinically. On examination, squeezing the metatarsal joints will cause pain on the plantar surface of the foot along with crepitus between the third and fourth toes (Mulder sign). Treatment involves metatarsal support with a bar or padded shoe inserts to decrease pressure on the metatarsal heads. Surgery is usually reserved for patients who fail conservative treatment.
Aphthous Stomatitis
Refers to localized, shallow, painful ulcers with a gray base. Recurrent aphthous stomatitis is the most common cause of oral ulcers.

Rare Disease Assumption
If the disease is rare (low disease prevalence), disease incidence (number of new cases) is typically low, and the OR generally approximates the RR. This is called the "rare disease assumption."
In addition to the "rare disease assumption," OR also approximates RR (regardless of disease incidence) when the cases and controls used in a study are representative of individuals with and without the disease in the overall population (with regard to the exposure of interest).
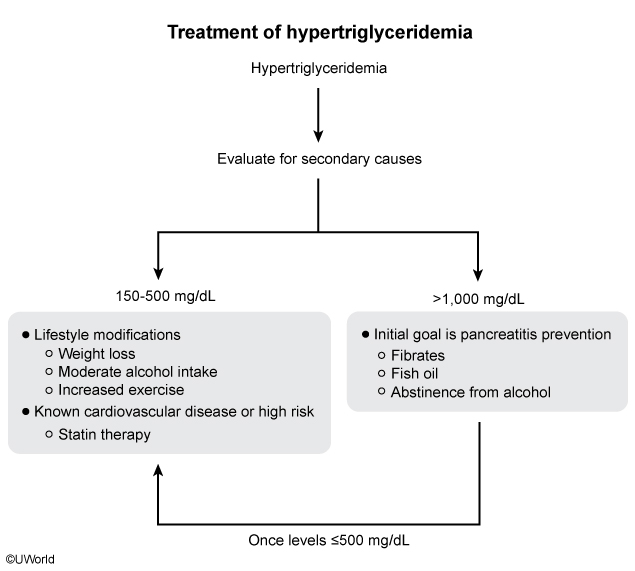
Hypertriglyceride
Lower Back Pain

Nephrotic syndrome
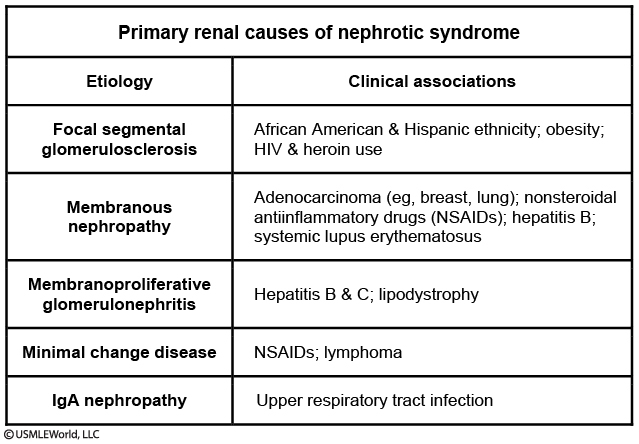
membranoproliferative glomerulonephritis is associated with hepatitis B and C infections, chronic bacterial infections (eg, endocarditis), and some autoimmune conditions. It is uncommonly associated with leukemias (chronic lymphocytic leukemia) or lymphomas (non-Hodgkin lymphoma, B-cell lymphoma) and is not typically seen in Hodgkin lymphoma.
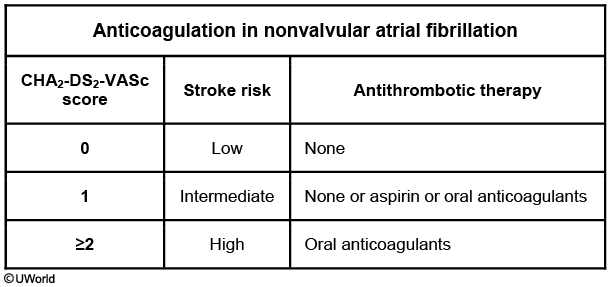
ChadVasc
Chad
Risk criteria
Score
C
Congestive heart failure
1
H
Hypertension
1
A2
Age ≥75*
2
D
Diabetes mellitus
1
S2
Stroke/TIA/thromboembolism
2
V
Vascular disease (prior myocardial infarction, peripheral artery disease, or aortic plaque)
1
A
Age 65-74*
1
Sc
Sex category (ie, female)
1
Maximum score
9
Venous Insufficiency
This patient's lower extremity (LE) swelling is likely due to chronic venous insufficiency (CVI), which is most commonly caused by incompetence of venous valves leading to venous hypertension in the deep venous system of the legs. Patients may present with leg discomfort, pain, or swelling that is typically worse in the evening or following prolonged standing and improves after walking or leg elevation. Pitting edema is the most common physical examination finding. In relatively severe cases, redirection of blood from the deep venous system to the superficial venous system may lead to other physical examination findings, including abnormal venous dilation (eg, telangiectasia, varicose veins), skin discoloration, lipodermatosclerosis, or skin ulceration (characteristically on the medial aspect of the lower leg). Risk factors for CVI include advancing age, obesity, family history, pregnancy, sedentary lifestyle, previous LE trauma, and previous LE venous thrombosis.


The diagnosis of CVI is usually based on history and physical examination, and initial treatment includes leg elevation, exercise, and compression stockings. Patients who do not respond to initial conservative measures should undergo venous duplex ultrasound to confirm the diagnosis of CVI by identification of venous reflux (retrograde venous blood flow) in the deep venous system.
Stent Thrombosis
Stent thrombosis is a potentially fatal complication of coronary artery stenting, and long-term dual antiplatelet therapy with aspirin and platelet P2Y12 receptor blocker (clopidogrel, prasugrel, ticagrelor) is recommended to reduce the risk of stent thrombosis after intracoronary drug-eluting stent placement. Premature discontinuation of antiplatelet therapy is the strongest predictor of stent thrombosis within the first 12 months, and all patients should be screened for, and counseled regarding, medication compliance to reduce the risk of stent thrombosis.
Ankylosing Spondylitis
Ankylosing spondylitis
Inflammatory back pain
Insidious onset at age less than 40 Symptoms >3 months Relieved with exercise but not rest Nocturnal pain
Examination findings
Arthritis (sacroiliitis) Reduced chest expansion & spinal mobility Enthesitis (tenderness at tendon insertion sites) Dactylitis (swelling of fingers & toes) Uveitis
Complications
Osteoporosis/vertebral fractures Aortic regurgitation Cauda equina
Laboratory
Elevated ESR & CRP HLA-B27 association
Imaging
X-ray of sacroiliac joints sMRI of sacroiliac joints
This patient has typical features of ankylosing spondylitis (AS), including chronic, progressive back pain and stiffness; pain relief with activity; lumbosacral tenderness; and reduced spinal range of motion. The incidence peaks in individuals age 20-30. Although AS has a male:female ratio of 2:1, it should be considered in any young patient with progressive low back pain and stiffness lasting >3 months.
In young patients with characteristic inflammatory back pain, plain x-rays of the pelvis showing sacroiliitis can confirm the diagnosis of AS. However, x-rays may be negative in early stages; MRI can confirm sacroiliitis in such cases. Fusion of the vertebral bodies with ossification of intervertebral discs (bamboo spine) also suggests the diagnosis. There is a strong association between HLA-B27 and AS, but whereas >90% of patients with AS have HLA-B27, only 5% of patients with HLA-B27 have AS. Therefore, HLA-B27 is not specific for AS and testing for it is not necessary for diagnosis. On the other hand, demonstrating radiographic changes of the axial skeleton is necessary for diagnosis.

Polymyalgia rheumatica (PMR) is characterized by achy pain in the shoulders and hips associated with elevated acute phase markers. A trial of glucocorticoids can help establish the diagnosis as patients with PMR will have prompt relief of symptoms. However, PMR is not seen before age 50 and does not affect spinal range of motion.
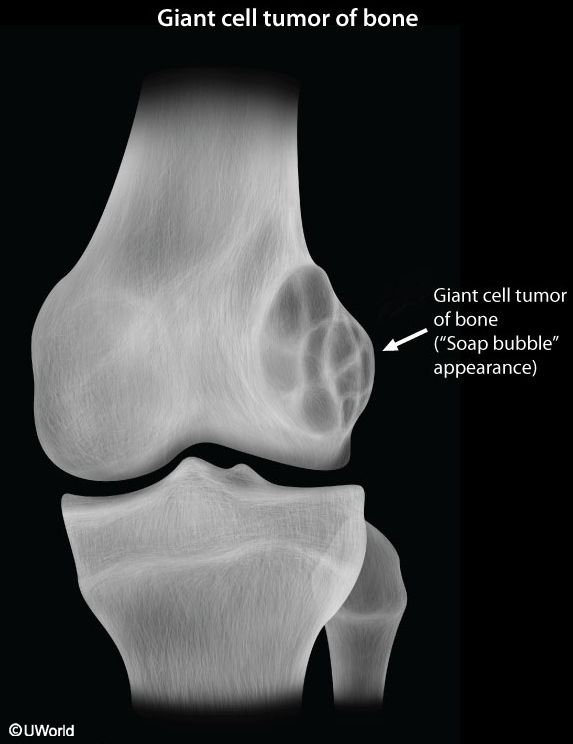
Giant Cell Tumor
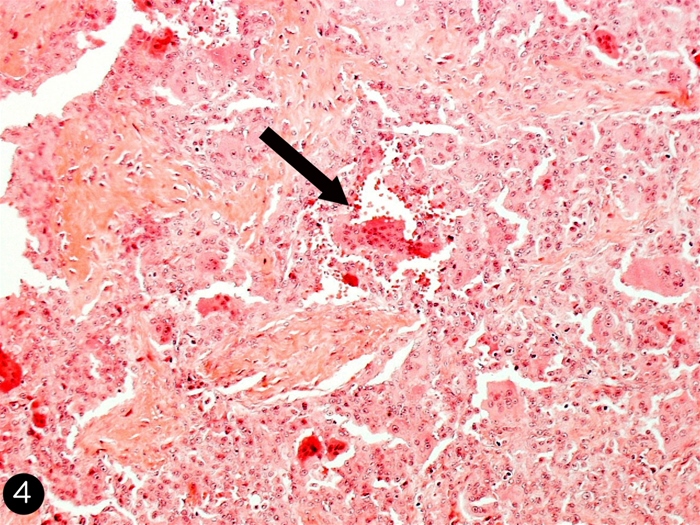
This patient's x-ray findings of an expansile and eccentric lytic area ("soap-bubble" appearance) are highly suggestive of giant cell tumor of bone (GCTB). GCTB is a benign and locally aggressive skeletal neoplasm seen in young adults. Patients usually present with pain, swelling, and decreased range of joint motion at the involved site. Nearly 10%-35% of affected patients experience pathologic fractures due to thinning of the bone cortex in weight-bearing areas.
GCTB typically presents on x-ray of the epiphyseal regions of the long bones, most commonly the distal femur and proximal tibia around the knee joint. Magnetic resonance imaging can show the tumor containing both cystic and hemorrhagic regions. Pathology typically shows sheets of interspersed large osteoclast giant cells that appear as round-to-oval polygonal or elongated mononuclear cells. Surgery (eg, intralesional curettage with or without bone grafting) is first-line treatment for GCTB.
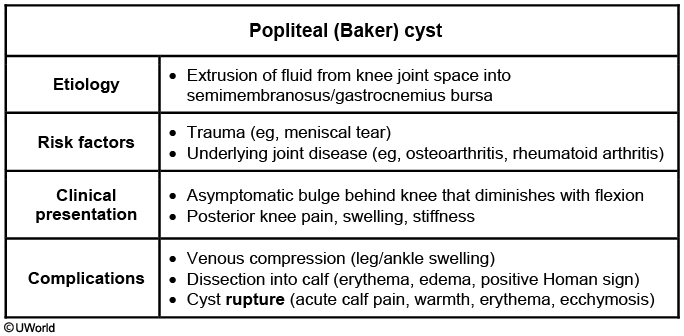
Baker's cyst
Osgood Schlatter

.,
X-ray of the knee typically shows avulsion of the apophysis of the tibial tubercle.
Osteoarthritis
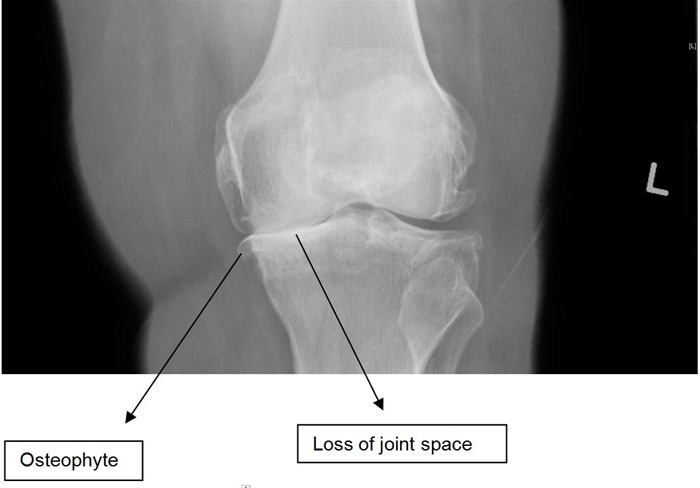
.,
Knee x-ray findings in patients with osteoarthritis include joint space narrowing, subchondral sclerosis, osteophyte formation, and subchondral cysts.
Osteoid Osteoma

.,
appears as a sclerotic, cortical lesion on imaging with a central nidus of lucency. It typically causes pain that is worse at night and unrelated to activity. However, the pain is quickly relieved by nonsteroidal anti-inflammatory medications.
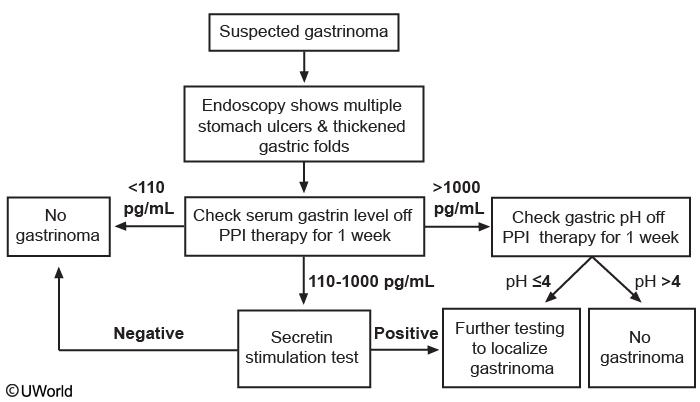
Gastrinoma
The excess gastric acid in the small intestine can cause diarrhea and steatorrhea due to inactivation of pancreatic enzymes and injury to the mucosal brush border.
Toxic ingestion
Caustic: conscious, alert. GI damage and severe pain. Dysphagia, heavy salivation, white tongue, GI ulceration
Cyanide is highly lethal and toxicity presents with headache, vomiting, abdominal pain and flushed skin. Inhalational exposure causes a bitter almond odor.
Otosclerosis
Otosclerosis is a common cause of conductive hearing loss in adults, especially those in their 20s and 30s, with a slight female predominance. The disorder involves an abnormal remodeling of the otic capsule thought to be a possible autoimmune process in genetically susceptible individuals. The stapes footplate becomes fixed to the oval window, resulting in loss of its piston action. This disorder is sometimes referred to as otospongiosis as CT scan may show a lucent (as opposed to sclerotic) focus in the temporal bone near the oval window. Conductive hearing loss. Treatment involves hearing amplification or surgical stapedectomy.
Peritonsilar abscess
This patient's symptoms are most likely secondary to a peritonsillar abscess. Although the three-day history of fever, chills, and sore throat were most likely secondary to tonsillitis, his muffled or "hot potato voice" and deviation of the uvula suggest that a peritonsillar abscess has developed as a complication of his tonsillitis. Patients with a peritonsillar abscess typically have prominent unilateral lymphadenopathy, as seen in this patient. This condition can be fatal secondary to either airway obstruction or spread of the infection into the parapharyngeal space, which may lead to involvement of the carotid sheath. Initial treatment consists of aspiration of the peritonsillar abscess and initiation of intravenous antibiotics. Surgical intervention may be necessary if the purulent material cannot be removed with aspiration alone.
Diffused Esophageal spasm
Diffuse esophageal spasm
Pathophysiology
Uncoordinated, simultaneouscontractions of esophageal body
Symptoms
Intermittent chest pain Dysphagia for solids & liquids
Diagnosis
Manometry: Intermittent peristalsis,multiple simultaneous contractions Esophagram: "Corkscrew" pattern
Treatment
Calcium channel blockers Alternates: Nitrates or tricyclics
This patient with intermittent non-cardiac chest pain and dysphagia has typical symptoms of diffuse esophageal spasm (DES). DES is characterized byuncoordinated, simultaneous contractions of the esophageal body, likely related to impaired inhibitory innervation in the esophagus. DES is frequently seen in association with emotional factors and functional gastrointestinal disorders. Symptoms often resemble those in achalasia (impaired esophageal motility with incomplete relaxation at the lower esophageal sphincter) and nutcracker esophagus (excessive tone at the lower esophageal sphincter).
The diagnosis of DES is challenging due to the episodic nature of clinical features. Esophageal manometry reveals intermittent peristalsis and multiple simultaneous contractions of the middle and lower esophagus. The lower esophageal sphincter usually shows normal relaxation. Esophagram may show nonperistaltic contractions producing a "corkscrew esophagus" pattern, although this is neither sensitive nor specific. Endoscopy is usually normal. First-line treatment includes calcium channel blockers (eg, diltiazem), which relieve pain and reduce dysphagia.

Costochondritis
Costosternal syndrome (costochondritis) usually occurs after repetitive activity. It is characterized by pain that is reproducible with palpation and worsened with movement or position changes. It would not cause dysphagia.
Eosinophilic esophagitis
Eosinophilic esophagitis is characterized by food impaction, dysphagia, or heartburn that does not respond to standard medications. Endoscopy usually reveals esophageal rings or strictures.
Globus Sensation
Globus sensation is a functional disorder of the esophagus characterized by the sensation of a foreign body in the throat. It is often worse when swallowing saliva and is frequently associated with anxiety. Pain, dysphagia, dysphonia, or systemic symptoms are not typical for globus and suggest another condition.
Transfusion reaction

IgA deficiency: Future transfusions should include IgA-deficient plasma and washed red cell products.
Febrile nonhemolytic transfusion reaction, the most common adverse reaction to transfusion, occurs within 1-6 hours of transfusion. During blood storage, leukocytes release cytokines that, when transfused, cause transient fevers, chills, and malaise. Respiratory distress and shock are not features of this reaction.
Transfusion-related acute lung injury presents with respiratory distress within 6 hours of transfusion. Patients have signs of noncardiogenic pulmonary edema, and chest x-ray shows bilateral interstitial infiltrates.
An anamnestic antibody response against a minor red blood cell antigen can lead to delayed mild hemolysis 2-10 days after transfusion
ABO mismatching is now rare, but it can still occur due to clerical errors and cause acute hemolytic transfusion reaction. Patients often present with fever, chills, flank pain, and hemoglobinuria within an hour of transfusion. This can progress to renal failure and disseminated intravascular coagulation (DIC).
TACO: Transfusion-associated circulatory overload (TACO) is a common transfusion reaction in which pulmonary edema develops primarily due to volume excess or circulatory overload. TACO typically occurs in patients who receive a large volume of a transfused product over a short period of time, or in those with underlying cardiovascular or renal disease.
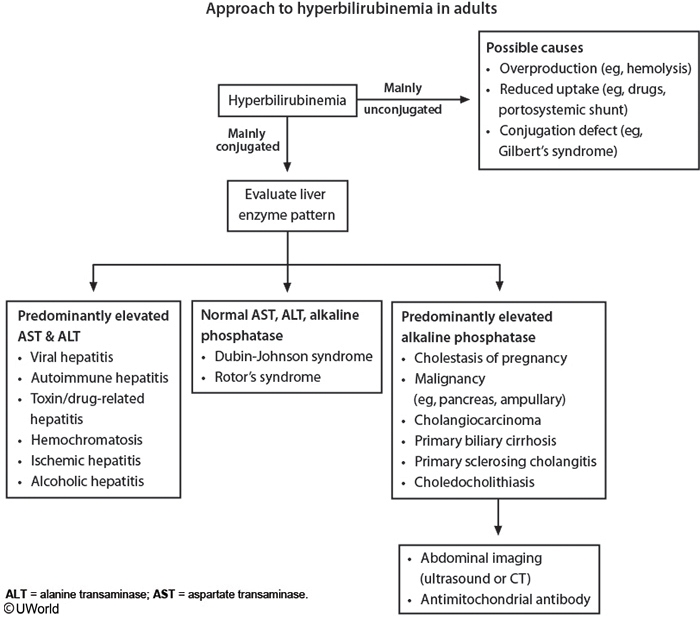
Hyperbilirubinemia
HIV esophagitis
The most common cause of esophagitis in patients with HIV is Candida albicans (>60% of cases); however, in patients whose predominant symptom is severe odynophagia (pain with swallowing) without dysphagia (difficulty swallowing) or thrush, viral esophagitis is more likely than candidal esophagitis. The most commonly implicated viruses include herpes simplex virus (HSV) and cytomegalovirus (CMV).
Hepatorenal syndrome
Hepatorenal syndrome
Risk factors
Advanced cirrhosis with portal hypertension & edema
Precipitating factors
Reduced renal perfusion GI bleed, vomiting, sepsis, excessive diuretic use, SBP Reduced glomerular pressure & GFR NSAID use (constricts afferent arterioles)
Diagnosis
Renal hypoperfusion FeNa less than1% (or urine Na less than10 mEq/L) Absence of tubular injury No RBC, protein, or granular casts in urine No improvement in renal function with fluids
Treatment
Address precipitating factors (eg, hypovolemia, anemia, infection) Splanchnic vasoconstrictors (midodrine, octreotide, norepinephrine) Liver transplantation
Hepatorenal syndrome (HRS) is an important complication of end-stage liver disease. It is characterized by a significant decrease in glomerular filtration in the absence of another clear cause of renal dysfunction, minimal hematuria (<50 erythrocytes/hpf), and lack of improvement with volume resuscitation.
HRS occurs as cirrhosis progresses and patients develop splanchnic arterial dilation and an overall decrease in vascular resistance. This, in turn, activates the renin-angiotensin system and results in local renal vasoconstriction withdecreased perfusion and glomerular filtration. The most common inciting factors of HRS include spontaneous bacterial peritonitis and gastrointestinal bleeding.
Definitive therapy involves return of liver function through either hepatic recovery (eg, abstinence from alcohol) or transplantation. For patients who are unlikely to have a quick recovery and are not candidates for liver transplantation, other temporizing options to increase renal perfusion include splanchnic vasoconstrictors (eg, midodrine, octreotide, norepinephrine) and albumin. Dialysis is of limited benefit but may be attempted to help bridge to liver transplantation.
Poly
Ddx
Clinical features
Diagnosis
Fibromyalgia
Young to middle-aged women Chronic widespread pain Fatigue, impaired concentration Tenderness at trigger points (eg, mid trapezius, costochondral junction)
>3 months of symptoms with widespread pain index or symptom severity score Normal laboratory studies
Polymyositis
Proximal muscle weakness (eg, increasing difficulty climbing up stairs) Pain mild/absent
Elevated muscle enzymes (eg, creatine kinase, aldolase, AST) Autoantibodies (ANA, anti-Jo-1) Biopsy: Endomysial infiltrate, patchy necrosis
Polymyalgia rheumatica
Age >50 Systemic signs & symptoms Stiffness > pain in shoulders, hip girdle, neck Association with giant cell (temporal) arteritis
Elevated ESR, C-reactive protein Rapid improvement with glucocorticoids
Polymyositis: Involvement of upper esophageal musculature can cause dysphagia with regurgitation and aspiration. Initial remission can be induced with glucocorticoids (eg, prednisone), and most patients also receive a glucocorticoid-sparing agent (eg, methotrexate, azathioprine) to minimize the long-term adverse effects of treatment.
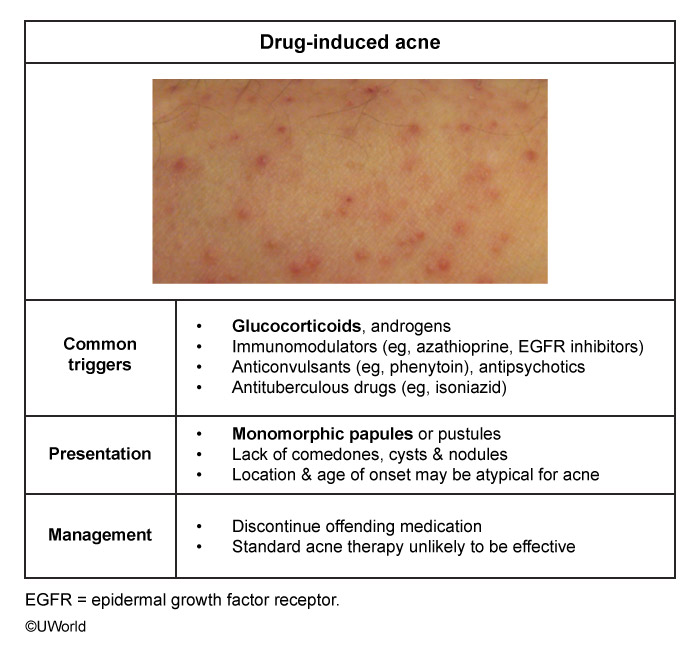
Drug Induced Acne
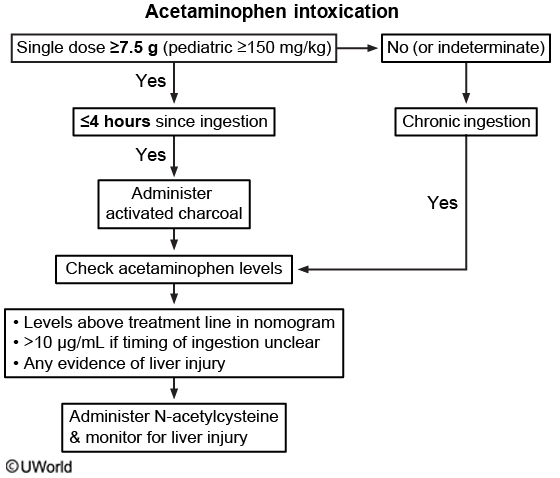
Acetaminophen toxicity
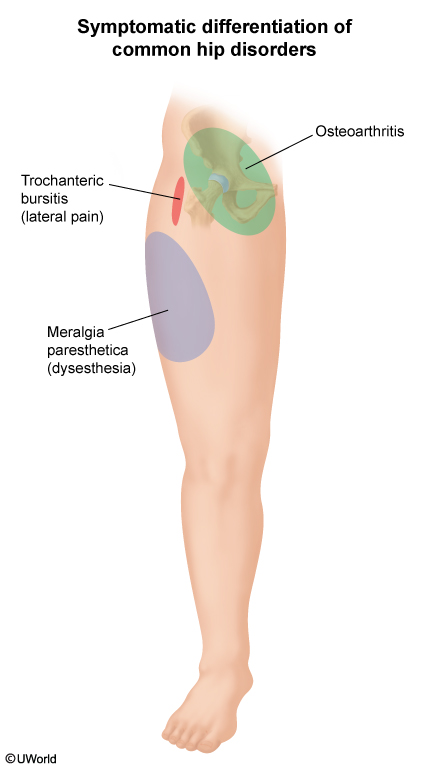
Common Hip pain
Polyp
Predominance of villous features (long glands on histologic examination, particularly in the presence of high-grade dysplasia
Large size (eg, >1 cm)
High number (eg, >3 concurrent adenomas)
In addition, sessile (nonpedunculated) adenomatous polyps are associated with an increased risk of synchronous advanced neoplasia and often require careful follow-up to ensure complete removal.
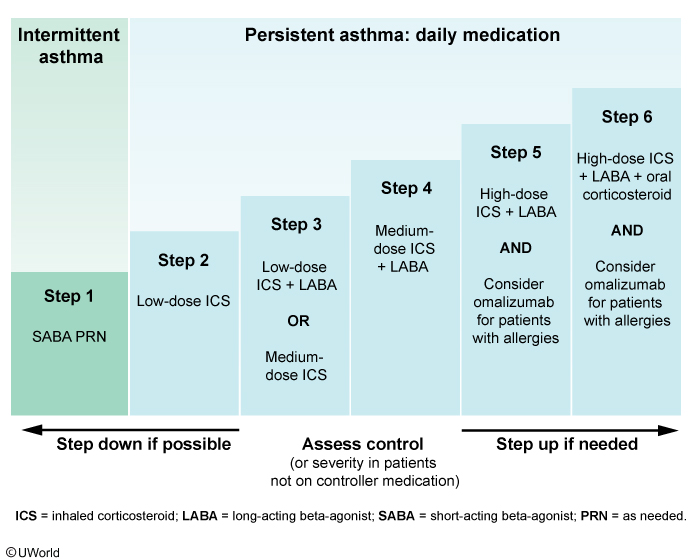
Asthma
Asthma severity for patients not on controller medication
Asthma severity
Symptom frequency/SABA use
Nighttime awakenings
Indicated therapy initiation
Intermittent
<2 days a week
<2 times a month
Step 1
Mild persistent
>2 days a week but not daily
3-4 times a month
Step 2
Moderate persistent
Daily
>1 time a week but not nightly
Step 3
Severe persistent
Throughout the day
4-7 times a week
Step 4 or 5
Hyperthyroidism
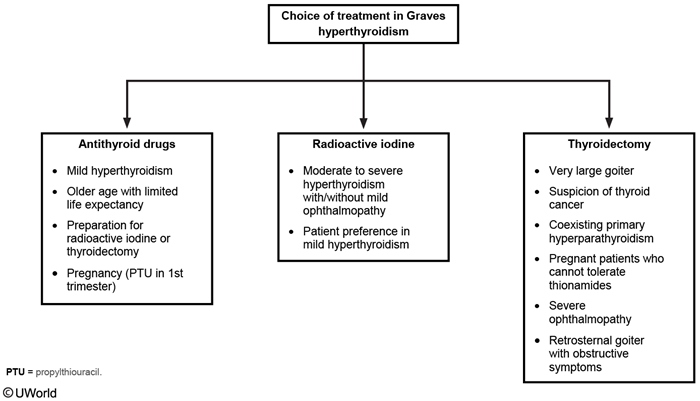
The 3 modalities for treatment of Graves disease include antithyroid drugs (ATDs) (eg, propylthiouracil, methimazole), radioactive iodine (RAI), and thyroidectomy. Most patients will require RAI or thyroidectomy.
Patients with mild disease, small goiters, and low TSH receptor antibody titers can be managed with an ATD alone and have a 50% likelihood of permanent remission. ATD therapy alone is also used in pregnant women or older patients with limited life expectancy.
In patients who have significant symptoms and thyroid hormone levels >2-3 times normal, an ATD with a beta blocker is initially recommended to stabilize the patient before definitive treatment with RAI or thyroidectomy. Pretreatment with ATDs is also recommended for patients at increased risk (eg, elderly, significant comorbidities) for complications due to the transient worsening of hyperthyroidism following RAI treatment. In light of this patient's age and severe thyrotoxicosis, treatment with an ATD is recommended prior to definitive treatment with RAI.
Panhypopituitarism
This patient's presentation suggests panhypopituitarism with inadequate production of multiple anterior pituitary hormones. Potential features include:
Central adrenal insufficiency (low cortisol and ACTH) - fatigue, anorexia, hypoglycemia, eosinophilia. Skin may be pale due to decreased production of ACTH and melanocyte-stimulating hormone
Hypogonadotropic hypogonadism (low FSH, LH, and testosterone) - low libido, erectile dysfunction, testicular atrophy
Central hypothyroidism (low or inappropriately normal TSH, low free T4) - cold intolerance, constipation, bradycardia
Patients may have mild hyponatremia (due to antidiuretic hormone release) and mild hypotension (due to decreased peripheral arterial resistance). Unlike cortisol, adrenal aldosterone secretion is regulated primarily by the renin-angiotensin system and is not affected in hypopituitarism. In contrast, in primary adrenal insufficiency, aldosterone production is lost, leading to hyperkalemia and severe hypotension, and ACTH production is increased, with associated hyperpigmentation.
Hypopituitarism is often due to compression by pituitary or extrapituitary tumors and may be associated with mass-effect symptoms (eg, headache, visual field defects). Other causes include infiltrative diseases (eg, sarcoidosis, hemochromatosis), trauma, and vascular insults (apoplexy, Sheehan syndrome).
Alkalosis
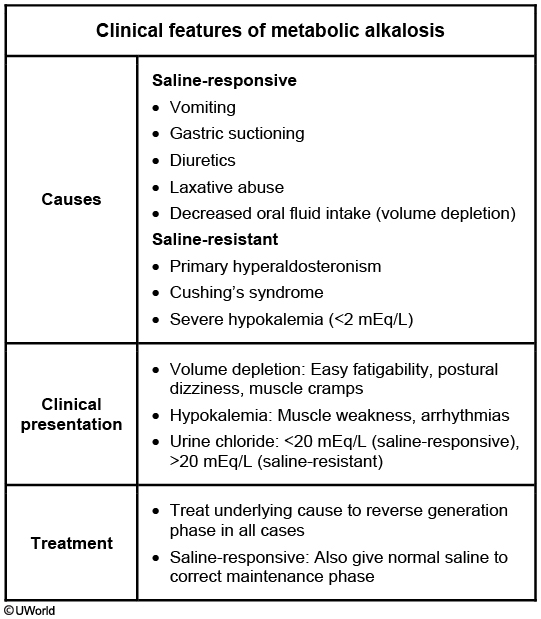
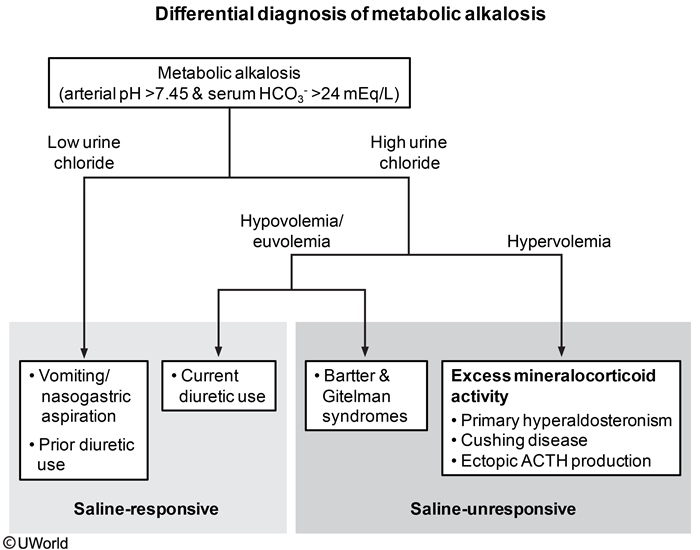
MA is due to an underlying disorder producing excess bicarbonate (generation phase) combined with a process preventing renal bicarbonate excretion (maintenance phase). MA is further classified as saline responsive or resistant. The generation phase in saline-responsive MA can be due to urinary or gastrointestinal hydrogen loss (eg, diuretics, vomiting) or decreased oral intake. The maintenance phase (eg, hypovolemia) prevents the normal kidney from excreting the excess bicarbonate in the urine. The kidneys perceive a decreased effective arterial blood volume from the underlying etiology (eg, vomiting with volume depletion) and increase renin and aldosterone release. This leads to sodium reabsorption, potassium excretion, and hydrogen excretion. There is also decreased bicarbonate excretion.
If the history cannot provide the etiology, urine chloride can differentiate between saline-resistant and saline-responsive MA. Saline-resistant MA has excess mineralocorticoid causing hydrogen and potassium loss and increased sodium retention leading to increased extracellular volume. The kidneys respond by excreting both sodium and chloride to result in high urine chloride. Saline-responsive MA has low urine chloride (<20 mEq/L) due to hypovolemia and hypochloremia. Treatment for both types focuses on the underlying cause to reverse generation and increase renal bicarbonate excretion. In saline-responsive MA, normal saline administration restores arterial volume, corrects hypochloremia, and increases urinary bicarbonate excretion.
Chronic pancreatitis

CP typically presents with chronic epigastric abdominal pain that can radiate to the back and is partially relieved by sitting upright or leaning forward.
Patients with CP develop progressive pancreatic inflammation that causes nonreversible exocrine and endocrine functional damage. Diarrhea, steatorrhea,and weight loss can develop due to fat malabsorption from reduced levels of exocrine pancreatic enzymes (eg, amylase, protease, lipase). CP eventually causes pancreatic endocrine failure with glucose intolerance or overt diabetes. Pancreatic calcifications seen on abdominal plain films or CT scan are helpful for establishing the diagnosis. In addition, CT scan helps exclude other etiologies (eg, pancreatic cancer, pseudocyst).
Mono
Rare but dangerous complications of infectious mononucleosis include splenic rupture, airway compromise, and autoimmune hemolytic anemia and thrombocytopenia. Anemia and thrombocytopenia are a result of the cross-reactivity of EBV-induced antibodies against red blood cells and platelets. These antibodies are IgM cold-agglutinin antibodies that cause complement-mediated destruction of red blood cells. Hemolysis likely explains the elevations in bilirubin and transaminase levels seen in this patient. Coombs test is generally positive, and reticulocyte count is elevated (also seen in this patient). The onset of the hemolytic anemia can be 2-3 weeks after the onset of symptoms.
TPN and gallstones
Gallbladder stasis is the most likely cause of gallstone formation in this patient. The presence of proteins and fatty acids in the duodenum acts as a stimulus for release of cholecystokinin (CCK), which in turn stimulates the contraction of the gallbladder. In patients on total parenteral nutrition or prolonged fasting, the normal stimulus for CCK release and gallbladder contraction is absent. This leads to biliary stasis and promotes the formation of bile sludge and gallstones.
ARDS
Most patients with ARDS require mechanical ventilation with the following goals:
Avoiding complications of mechanical ventilation by using lung-protective strategies such as low tidal volume ventilation (LTVV): LTVV (6 mL/kg of ideal body weight) decreases the likelihood of overdistending alveoli and provoking barotrauma due to high plateau pressures (pressure applied to small airways and alveoli). LTVV improves mortality in patients with ARDS. In contrast, higher tidal volumes in ARDS may result in elevated pulmonary pressures due to the work of forcing larger volumes into stiff lungs (decreased compliance), leading to increased alveolar distension.
Providing adequate oxygenation: Increasing the fraction of inspired oxygen (FiO2) administered by the ventilator improves oxygenation; however, prolonged FiO2 levels >0.6 are associated with oxygen toxicity. Increasing positive end-expiratory pressure (PEEP) also improves oxygenation by preventing alveolar collapse at the end of expiration, thereby decreasing shunting and the work of breathing. Given the severe hypoxemia seen in ARDS, PEEP levels up to 15-20 cm H2O may be necessary to maintain oxygenation. The goal is arterial partial pressure of oxygen (PaO2) at 55-80 mm Hg or peripheral saturation (SpO2) at 88%-95% (ie, preventing SpO2 <88%, not <92%).
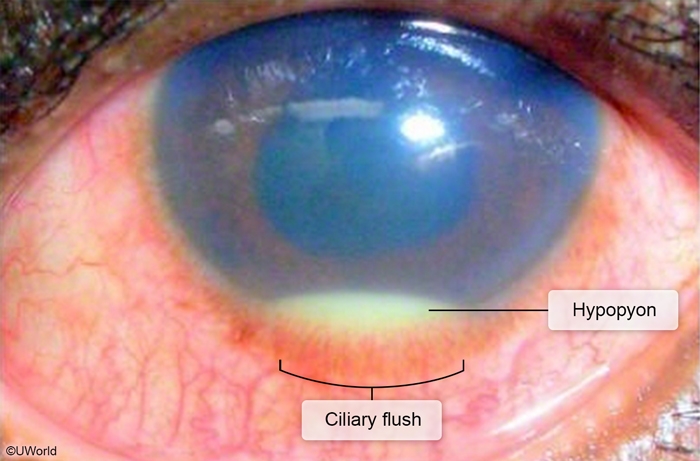
Uveitis
Examination findings in anterior uveitis can include hyperemia concentrated at the junction of the sclera and cornea (ciliary flush), pupillary constriction, a hazy "flare" in the aqueous humor, and layering of white cells in the anterior chamber (hypopyon).
Sjogren
Sjögren syndrome (SS) is an autoimmune disorder characterized by inflammation of exocrine glands, with a greatest incidence in middle-aged women. Patients can have severe dry mouth (xerostomia) with dysphagia (difficulty swallowing), thrush, and dental caries. Involvement of lacrimal glands causes keratoconjunctivitis sicca (eg, dry eyes). Extraglandular features include arthritis, Raynaud phenomenon, cutaneous vasculitis, interstitial lung disease, and increased risk for non-Hodgkin lymphoma.
The diagnosis of SS is made in patients with ocular or oral dryness when there is:
Evidence of dry mouth and eyes. In the Schirmer test, a sterile strip of filter paper is placed under the lower eyelid, and the area moistened by the absorbed fluid is measured after 5 minutes.
Either histologic evidence of lymphocytic infiltration of the salivary glands or presence of serum autoantibodies directed against SSA (Ro) and/or SSB (La).
Antinuclear antibodies and rheumatoid factor are less specific but helpful when positive.
Scabies
Scabies
Pathogenesis
Sarcoptes scabiei mite infestation Spread by direct person-to-person contact
Clinical features
Extremely pruritic pathognomonic burrows & small, erythematous papules Rash located on interdigital web spaces, flexor wrists, extensor elbows, axillae, umbilicus & genitalia
Treatment
Topical 5% permethrin OR Oral ivermectin
Scabies is due to infestation by Sarcoptes scabiei mites, which spread through person-to-person contact. The mites burrow into the skin, leading to a delayed type IV hypersensitivity reaction to the mite, feces, and eggs. Scabies presents with anintensely pruritic rash with small, crusted, red papules and linear burrows. Patients can also develop vesicles, pustules, and wheals with extensiveexcoriations. The most common locations include the flexor surface of the wrist, lateral surfaces of the fingers, and the finger webs. Scabies can affect exposed and unexposed skin.
Diagnosis is confirmed by light microscopy of skin scrapings revealing mites, ova, and feces. Topical permethrin or oral ivermectin can eliminate the infestation. Bedding and clothing should be cleaned or placed in a plastic bag for >3 days as mites can live away from human skin for only 2-3 days.

Bed Bugs
However, bed bug bites most often cause small, punctate lesions with surrounding erythema, classically in linear tracks or clusters ("breakfast, lunch, and dinner" bites). Bites on the palms and soles are uncommon due to the thickness of the skin. Intense pruritus that is worse at night, pustules, finger web involvement, and excoriations (due to mites digging burrows) are all more suggestive of scabies.
Cyanide
This patient is the victim of a house fire and most likely has a smoke inhalation injury; such injuries are estimated to cause 60%-80% of deaths during fire incidents. Smoke injury results in glottic edema from heat and airway irritation due to particulate matter found in smoke. Smoke also contains multiple toxins that are absorbed systemically. Hydrogen cyanide (HCN) and carbon monoxide (CO) are the 2 major products of combustion in closed spaces. HCN is produced from the combustion of nitrogen-containing synthetic polymers (eg, foam, cotton, paint, silk).
HCN is a potent and fast-acting poison, and blood levels cannot be measured rapidly to confirm diagnosis prior to treatment. Toxic exposure can be inhalational, dermal, or intestinal. Exposure to moderate to high concentrations causes symptoms to develop within seconds to minutes. Early acute toxicity causes neurologic and cardiorespiratory stimulation, and patients develop headache, vertigo, dizziness, hyperventilation, tachycardia, nausea, and vomiting. Neurologic, respiratory, and cardiovascular depression eventually occurs and manifests as coma, seizures, bradycardia, hypotension, and cardiorespiratory arrest. HCN can also cause anoxic brain injury leading to permanent neurologic deficits.
Cyanide toxicity can be treated with an antidote such as hydroxocobalamin or sodium thiosulfate, which directly binds cyanide molecules. An alternate treatment is induction of methemoglobinemia with nitrites to increase ferric iron (Fe3+) in circulating hemoglobin. Cyanide binds avidly to Fe3+, and so methemoglobinemia provides an alternate binding site.
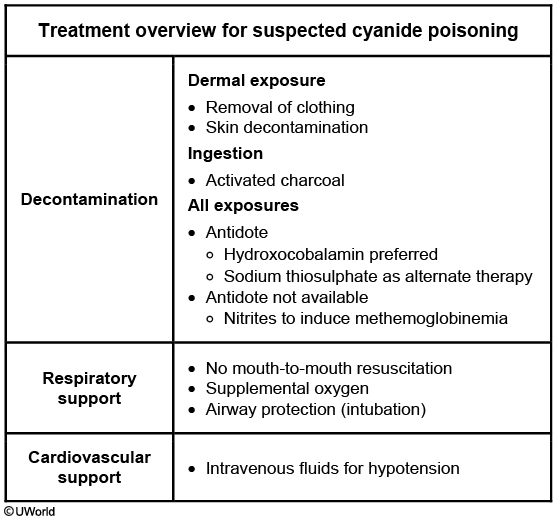
Cyanide is a potent inhibitor of cytochrome oxidase a3 in the mitochondrial electron transport chain. It binds to ferric iron (Fe3+), inhibiting its reduction to ferrous iron (Fe2+) and blocking production of ATP from oxidative phosphorylation. Cells then switch to anaerobic metabolism, leading to lactic acid formation and causing metabolic acidosis. Serum bicarbonate levels fall in an attempt to buffer excess acid. Metabolic acidosis also triggers central and peripheral chemoreceptors, increasing alveolar ventilation and then presenting as tachypnea. This leads to a fall in arterial PCO2 (PaCO2).
Papillary Thyroid Cancer
surgery
Duputren
Dupuytren contracture is due to progressive fibrosis of the palmar fascia and presents with a palmar nodule or thickening (usually at the fourth and fifth digits), with possible nodule formation along the flexor tendons near the distal palmar crease. Progressive disease leads to decreased extension of the digits.

PTH
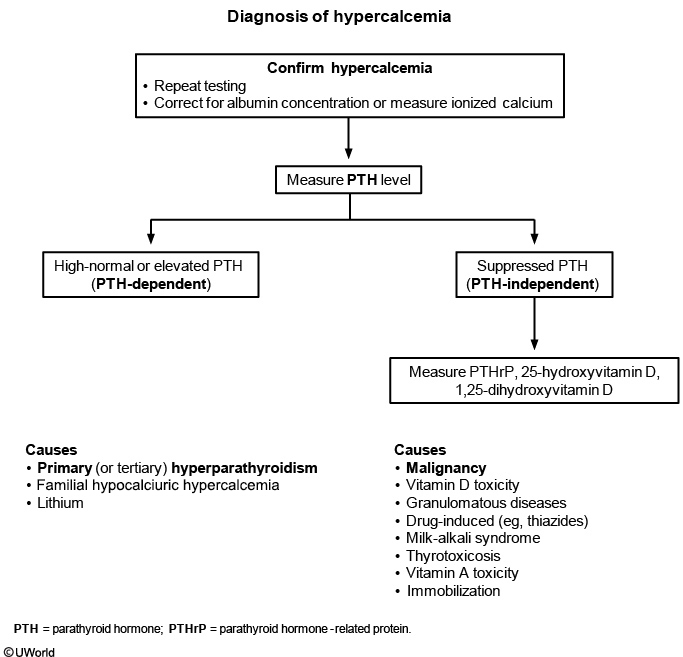
Lyme disease prophylaxis
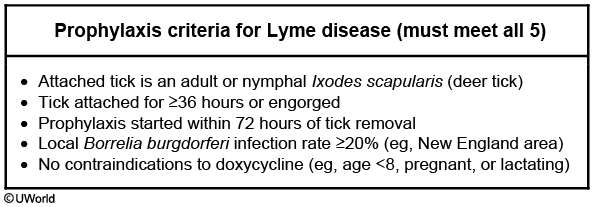
Although anaplasmosis and babesiosis are typically transmitted soon after tick attachment, B burgdorferi resides in the gut of the tick and requires 48-72 hours of feeding before salivary gland migration. As such, patients with a tick attached for <36 hours are extremely unlikely to acquire Lyme disease and do not require antimicrobial prophylaxis. Ticks should be removed with tweezers as close to the skin surface as possible.
Cardiac Stress Test
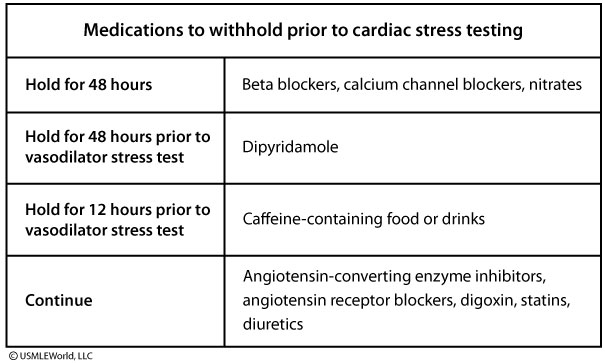
Interstitial Cystitis
Epidemiology
More common in women Associated with psychiatric disorders (anxiety) & pain syndromes (fibromyalgia)
Clinical presentation
Bladder pain with filling, relief with voiding ↑ Frequency, urgency Dyspareunia
Diagnosis
Bladder pain with no other attributable cause for >6 weeks Normal urinalysis
Treatment
Not curative; focus is on quality of life Behavioral modification & trigger avoidance Amitriptyline Analgesics for exacerbations
Interstitial cystitis (also known as painful bladder syndrome) is a chronic, painful bladder condition of uncertain etiology. The pelvic pain in interstitial cystitis is classically exacerbated by bladder filling and relieved by voiding. The onset of the symptoms is typically gradual, and the symptoms worsen over a period of months. Other characteristic symptoms include urinary urgency and frequency, and chronic pelvic pain. The pain can be exacerbated by exercise, sexual intercourse (dyspareunia), and alcohol consumption.
The diagnosis of interstitial cystitis is primarily clinical. Urinalysis is obtained to exclude other causes of bladder pain (eg, urinary tract infection, sexually transmitted disease, cancer); results are normal in interstitial cystitis. Treatment is palliative and includes trigger avoidance, amitriptyline, and analgesics for pain flares.
Condyloma vs Kaposi
condyloma: has no lymphadema
kaposi: has lymphedema: prominent lymphedema (due to vascular obstruction by KS lesion or to cytokine production), which can manifest as extremity swelling, can sometimes be seen.
Dermatitis Herpetiformis
Dermatitis herpetiformis (DH) causes intensely pruritic erythematous papules, vesicles, and bullae that occur symmetrically in grouped ("herpetiform") clusters on the extensor surfaces of the elbows, knees, back, and buttocks. DH represents an autoimmune dermal reaction due to dietary gluten and is commonly associated withceliac disease (the likely cause of this patient's diarrhea and weight loss), although it may precede the gastrointestinal manifestations.
Skin biopsy in DH shows subepidermal microabscesses (blisters) at the tips of the dermal papillae; immunofluorescence studies show deposits of anti-epidermal transglutaminase IgA in the dermis. Initial treatment includes dapsone, which has anti-inflammatory and immunomodulatory properties and provides rapid relief of symptoms. Long-term management requires a gluten-free diet.
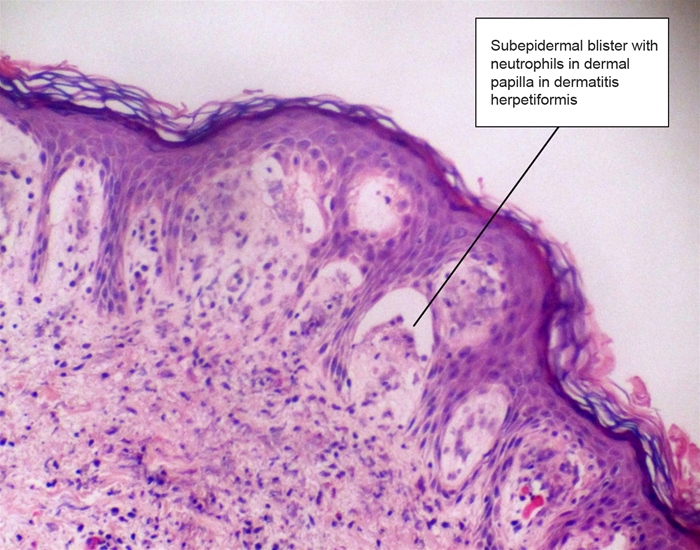
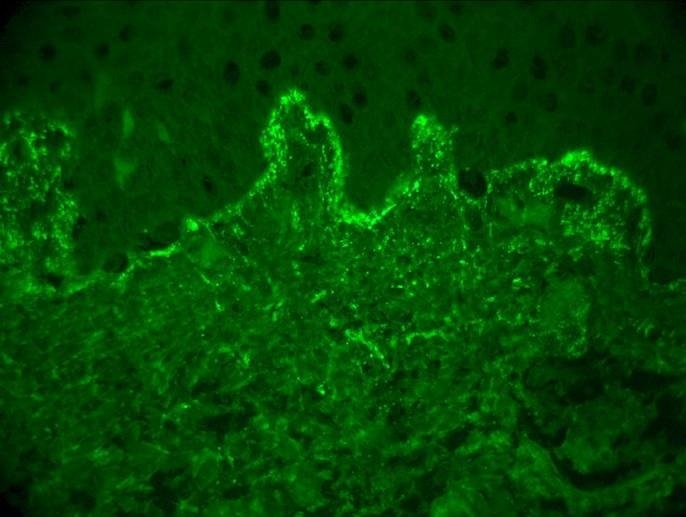
HIV associated neurocognitive
symptoms
Impaired memory & attention/concentration
Personality & behavior changes
Motor symptoms (eg, ataxia, slowed movement)
HIV:
Long-standing HIV disease
Age >50
CD4 count <200/mm3
This patient has personality changes, forgetfulness, and signs of impaired neurocognitive function. Given his long-standing HIV disease, this presentation is most likely due to HIV-associated neurocognitive disorder (HAND). HAND is characterized by a chronic decline in multiple cognitive domains (eg, memory, attention, calculation, executive function). Mood and behavior disturbances are common. The diagnosis is based primarily on clinical features and neuropsychological testing, but MRI may also be helpful and shows a diffuse increase in intensity in the white matter.
Progressive multifocal leukoencephalopathy is caused by reactivation of the JC virus and has an increased incidence in patients with chronic HIV disease. Symptoms include altered mental status, motor deficits, ataxia, and vision abnormalities. MRI shows focal, asymmetric (rather than diffuse) lesions.
Oliguria
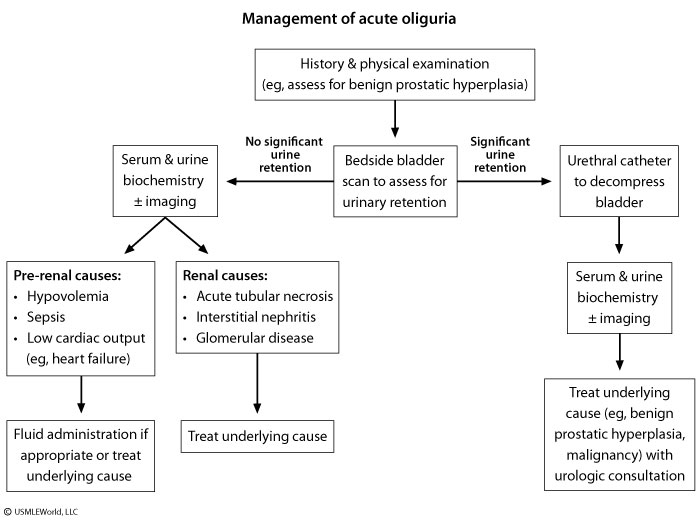
Pyuria
wbc on UA but negative clx
Sterile pyuria — Whereas true infection without pyuria is unusual, pyuria can occur in the absence of apparent bacterial infection, particularly in patients who have already taken antimicrobials (often due to self-medication). Other causes of sterile pyuria include:
Contamination of the urine sample
Chronic interstitial nephritis (NSAIDS use)
Nephrolithiasis
Uroepithelial tumor
Inflammation (Alport)
Infection: prostatitis, epididymidis
Infection with atypical organisms, such as Chlamydia/Gonorrhea, Ureaplasma urealyticum, or tuberculosis.
In the case of uroepithelial tumors, both malignant cells and leukocytes are shed. The tumor can cause inflammation that results in the appearance or exacerbation of sterile pyuria. Malignant cells are difficult to distinguish from leukocytes on routine urinalysis.
Also, some women with UTI may have low bacterial counts in their midstream urine. If the clinical laboratory does not quantify bacterial counts below a certain threshold, they may not be identified as having bacteriuria despite consistent symptoms and pyuria.
Pulmonary contusion
Pulmonary contusion results in intraalveolar hemorrhage.
CO Poisoning
Manifestations of mild to moderate toxicity include headache, nausea, dyspnea, malaise, altered mentation, seizures, and dizziness.,
Post cholecystectomy
This patient's presentation is concerning for postcholecystectomy syndrome (PCS). PCS refers to persistent abdominal pain or dyspepsia (eg, nausea) that occurs either postoperatively (early) or months to years (late) after a cholecystectomy. PCS can be due to biliary (eg, retained common bile duct or cystic duct stone, biliary dyskinesia) or extra-biliary (eg, pancreatitis, peptic ulcer disease, coronary artery disease) causes. Patients usually notice the same pain they had prior to surgery, new pain just after surgery, or the same pain that never went away.
Laboratory findings can include elevated alkaline phosphatase, mildly abnormal serum aminotransferases, and dilated common bile duct on abdominal ultrasound. These findings usually suggest common bile duct stones or biliary sphincter of Oddi dysfunction. The next step involves endoscopic ultrasound, endoscopic retrograde cholangiopancreatography (ERCP), or magnetic resonance cholangiopancreatography for final diagnosis and guiding therapy. Treatment for PCS is directed at the causative factor.
Aortic Dissection
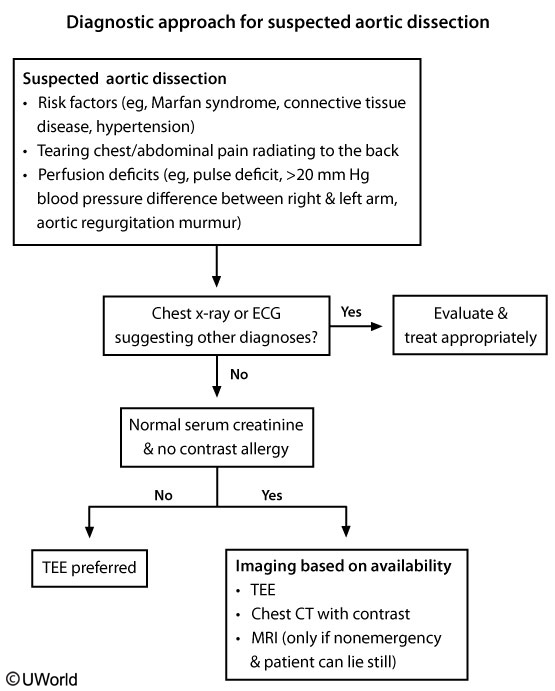
elevated creatinine of 2.1 mg/dL (possibly due to distal extension into the renal arteries)
Transesophageal echocardiography has excellent sensitivity and specificity and is the preferred diagnostic study in patients with renal insufficiency (such as this patient) or hemodynamic instability.
CT angiography is the preferred diagnostic study in hemodynamically stable patients; however, it requires the use of iodinated contrast agents and should be avoided in patients with renal insufficiency.
MR angiography is more time consuming and requires the administration of gadolinium-containing contrast agents for contrast enhancement; it should also be avoided in patients with moderate to severe kidney disease due to the risk of nephrogenic systemic fibrosis
Flu vs viral vs strep
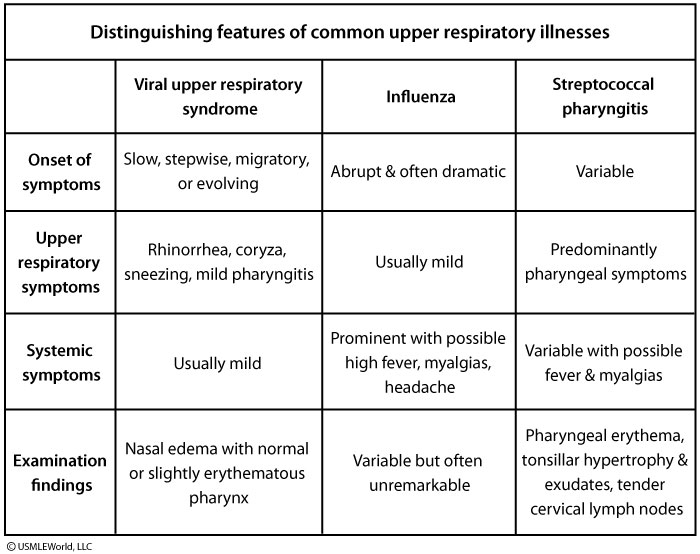
Takayasu
This patient with exertional arm pain (likely claudication), systemic symptoms, and pulse deficits has typical features of Takayasu arteritis, a chronic large artery vasculitis that predominantly affects Asian women age <40. It primarily involves the aorta and its branches and is characterized by mononuclear infiltrates and granulomatous inflammation of the vascular media, leading to arterial wall thickening with aneurysmal dilation or narrowing and occlusion.
Initial symptoms are nonspecific (eg, fever, arthralgias, weight loss). As the disease progresses, vascular involvement with arterio-occlusive manifestations (eg, claudication, distal ulcers) may develop, particularly in the upper extremities. Examination findings include blood pressure discrepancies, pulse deficits, and bruits. Patients commonly have anemia and elevated inflammatory markers (eg, erythrocyte sedimentation rate, C-reactive protein). Chest x-ray can reveal aortic dilation and a widened mediastinum, and CT and MRI may reveal thickening of large artery walls and lumenal narrowing. Initial treatment includes systemic glucocorticoids.
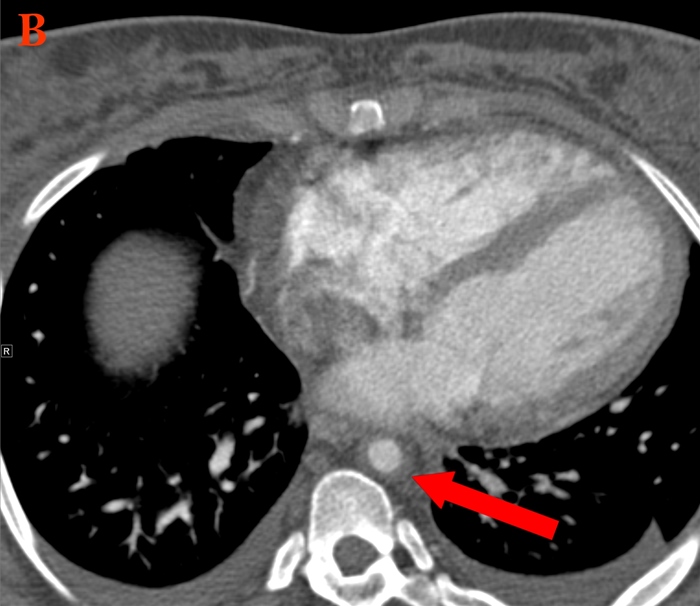
Male Hypogonadism
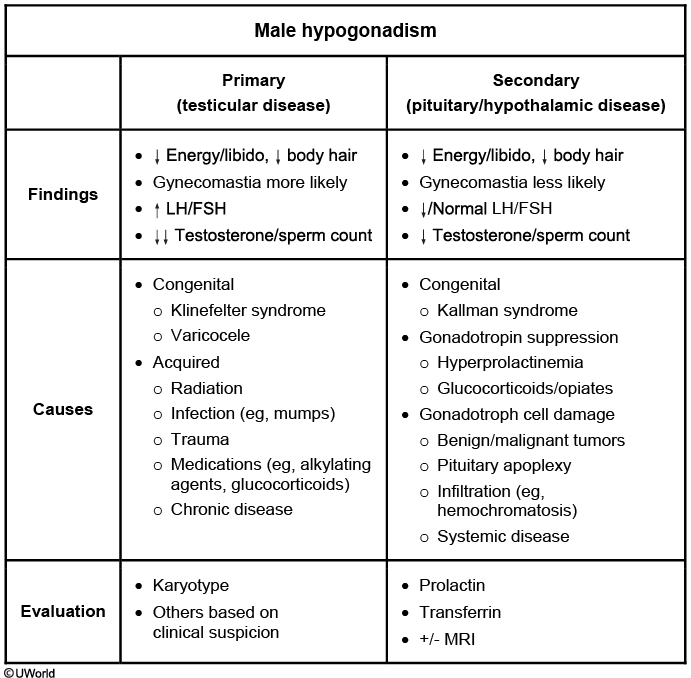
Secondary hypogonadism can be due to mass lesions in the hypothalamus or pituitary, hyperprolactinemia (due to suppression of gonadotropin-releasing hormone), long-term use of glucocorticoids or opiates, or severe systemic illness. Secondary hypogonadism is also more common in individuals with obesity or type 2 diabetes mellitus. Patients with secondary hypogonadism should have measurement of serum prolactin.
Hemochromatosis should be suspected when hypogonadism is associated with abnormal skin pigmentation, diabetes mellitus, elevated liver enzymes, and arthropathy.
Steven Johnsons
TEN and Stevens-Johnson syndrome (SJS) are related disorders and may be considered on a continuum of severity. By convention, SJS denotes involvement of less than 10% of body surface area, >30% is designated TEN, and 10-30% is referred to as a SJS/TEN overlap syndrome. The treatment of TEN and SJS is primarily supportive, with wound care similar to that for burns (and often provided in a designated burn unit). Aggressive fluid support is often needed due to poor oral intake and profound cutaneous fluid loss. Secondary infections are common, and antiseptic precautions are needed.
Contact lens keratitis
This patient with a painful, red eye and opacification and ulceration of the cornea has typical features of contact lens-associated keratitis. Most cases are due to Gram-negative organisms such as Pseudomonas and Serratia, but can also be due to Gram-positive organisms as well as certain fungi and amoebas. Contact lens-associated keratitis is a medical emergency and can lead to corneal perforation, scarring, and permanent vision loss if not addressed promptly. In addition to removal and discarding of the contact lens, most patients require topical broad-spectrum antibiotics.
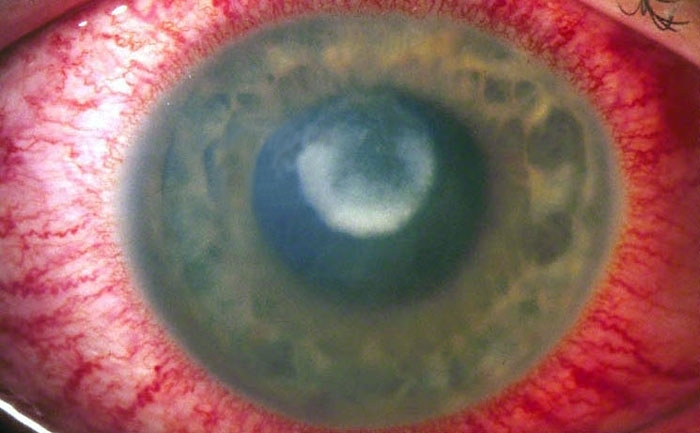
Porphyria
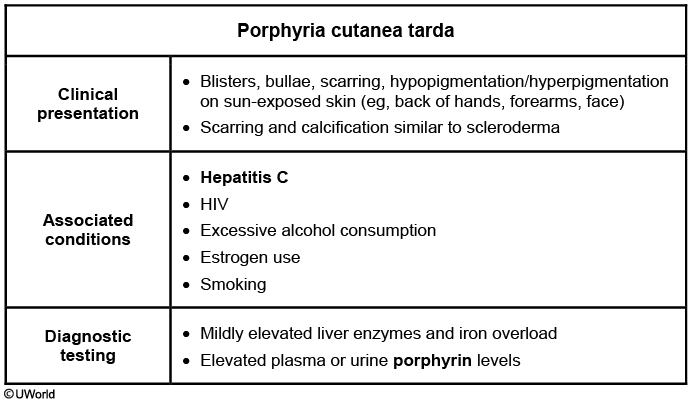
This patient with dermal blisters on the hands and untreated hepatitis C has typical features of porphyria cutanea tarda (PCT). The porphyrias are hereditary or acquired disorders of heme synthesis. Enzyme deficiencies in the early steps of porphyrin synthesis (eg, acute intermittent porphyria) cause abdominal pain and neuropsychiatric manifestations (eg, psychosis, neuropathy); abnormalities in the later steps (eg, PCT) lead to photosensitivity due to accumulation of porphyrinogens that react with oxygen on excitation by ultraviolet light. PCT is due to deficiency of uroporphyrinogen decarboxylase and is the most common porphyria.
PCT is characterized by painless blisters that heal with scarring, increased skin fragility on the dorsal surfaces of the hands, facial hypertrichosis, and hyperpigmentation. It can be triggered by ingestion of certain substances (eg, ethanol, estrogens) and is most common in patients with underlying hepatitis C. Elevated plasma or urinary porphyrin levels confirm the diagnosis. Phlebotomy or hydroxychloroquine may provide relief, as can treatment for hepatitis C.

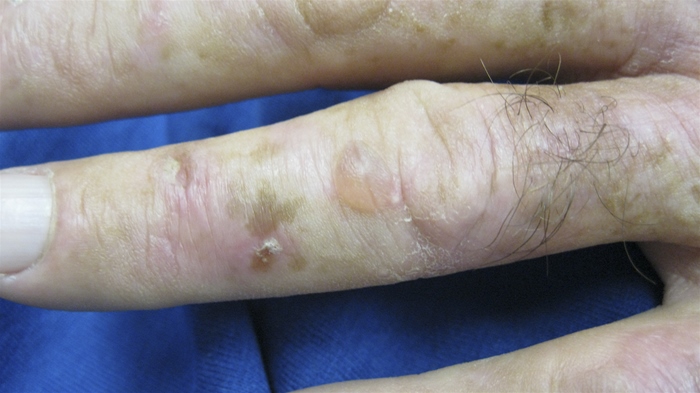
Last updated