01 Coagulation
Bleeding

occurs before any thrombus formation
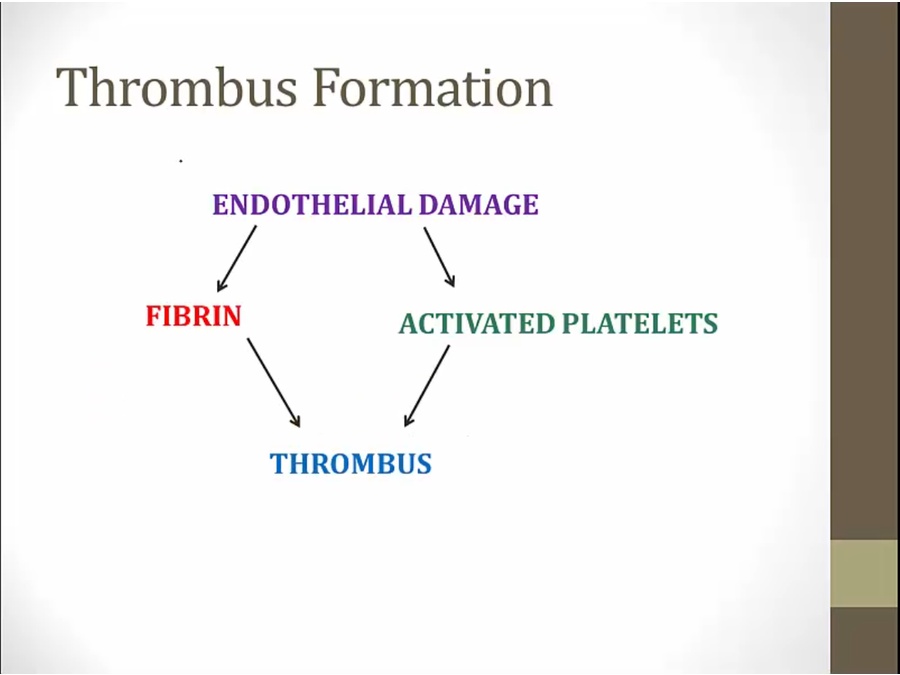
coagulation = fibrin formation into clot to stop blood loss
Coagulation Factors

First soluble. Become insoluble when activated



Coagulation Cascade
Main

fibrin insoluble, precipitate


Tissue Factor

when endothelium intact, no contact
when damaged, tissue factors expressed


not very effective, no amplification
Thrombin

thrombin amplification
5, 8, 11 activate more 10


hemophilia: low 8 or 9
Von Willebrand

unique: in endothelium
megakaryocytes: von willebrand stored in platelets and endothelium
injury: factor 8 released from vWF, thrombin formation
Factor 13
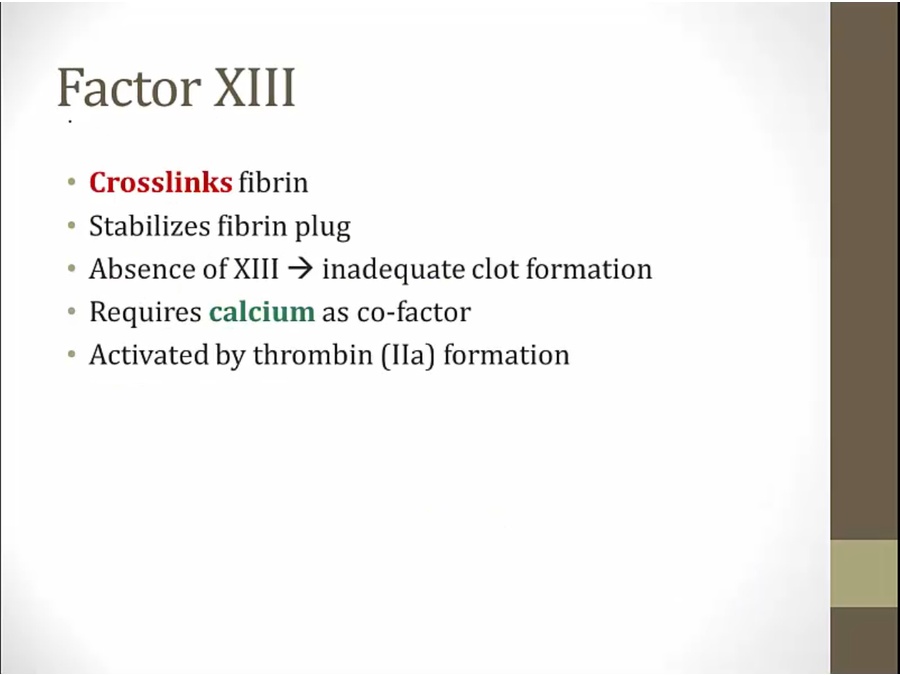
formed but not crosslinked

Factor 12

activate coagulation system when exposed to silica
Extrinsic and Intrinsic
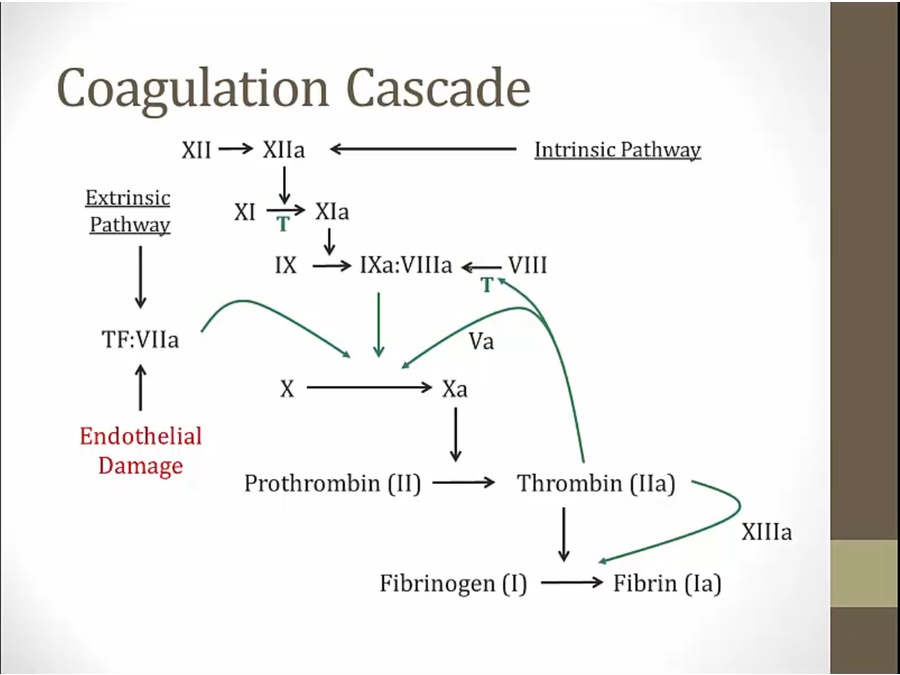
how written in textbook
1st pathway: TF pathway from TF:VIIa
2nd pathway: factor 12
T: which factors activated by thrombin



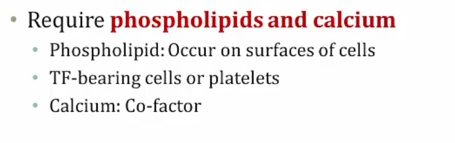
phospholipid: required, exists on TF cells or platelets
Calcium

needed in both pathways

used to be called factor 4

Kinin
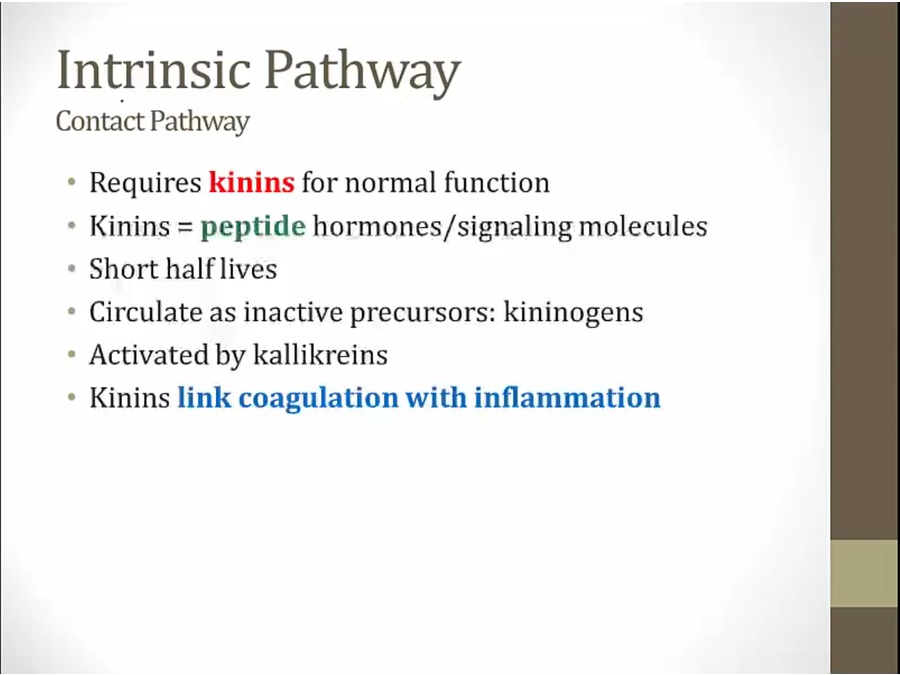
contact pathway: activated when plasma in contact with negatively charged substances
link between coagulation and inflammation
generated by factor 12

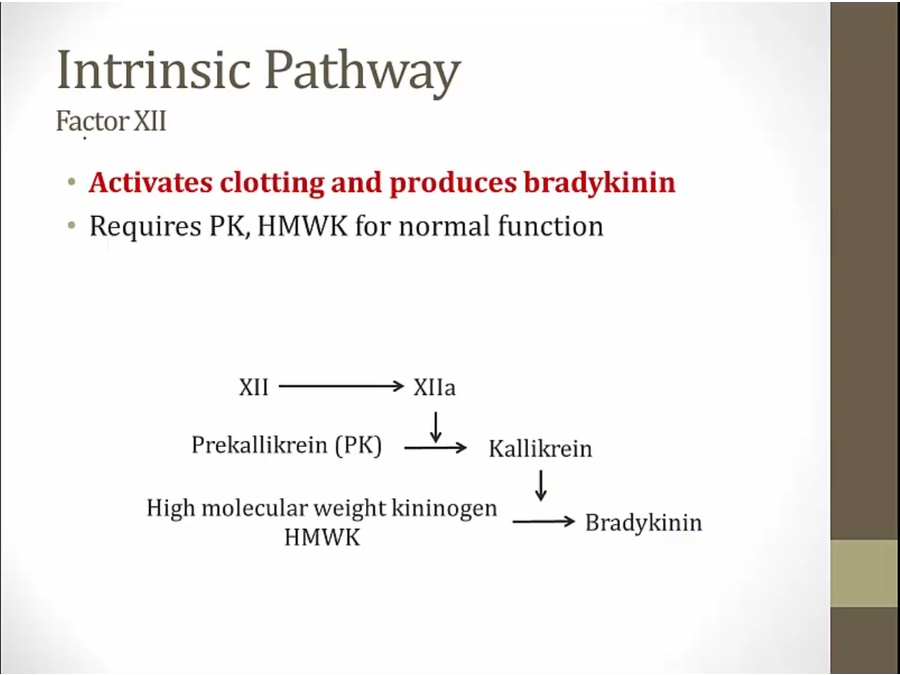
factor 12 leads to synthesis of bradykinin
link between coagulation system and kinin system (inflammation)

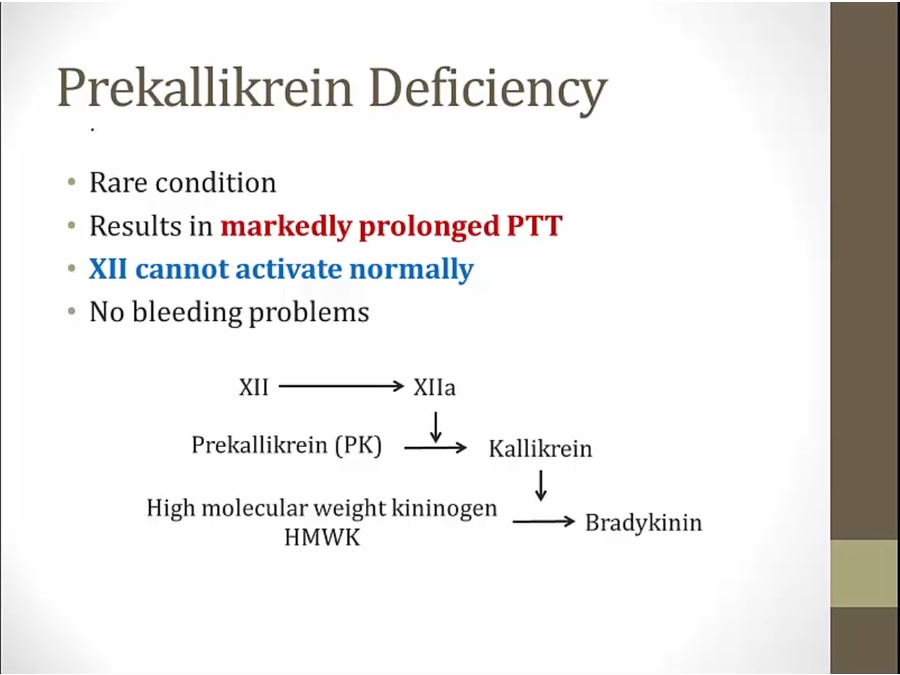
cannot activate bradykinin
routine test of PTT shows prolonged. No medical problems because 12 doesn't have a lot of physiologic significance

Coagulation Inhibitors

Antithrombin III

activated by healthy endothelial cells
Protein C and S

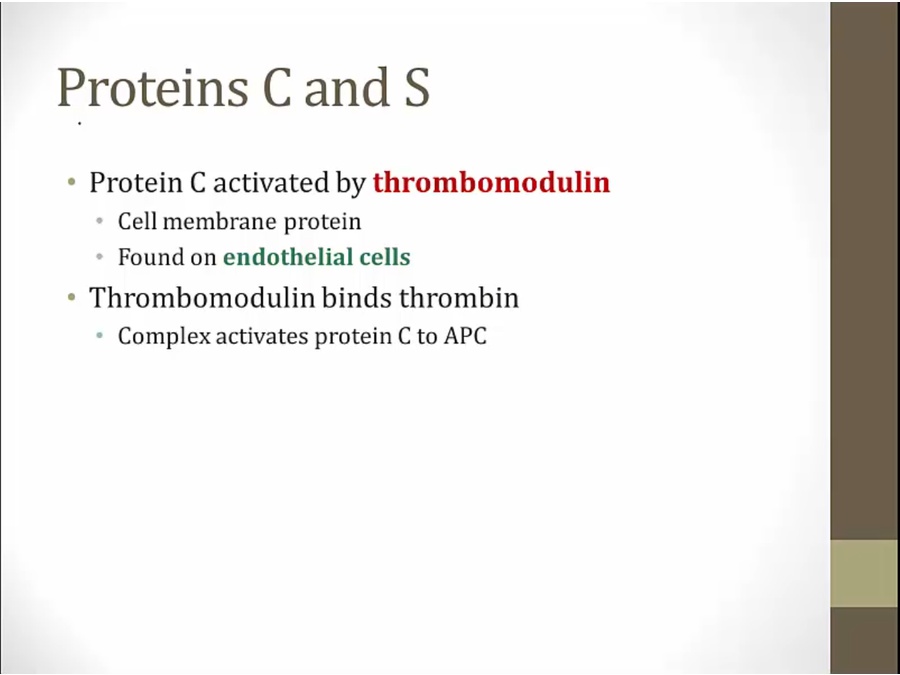
healthy endothelium: produce lots of thrombomodulin, less thrombin
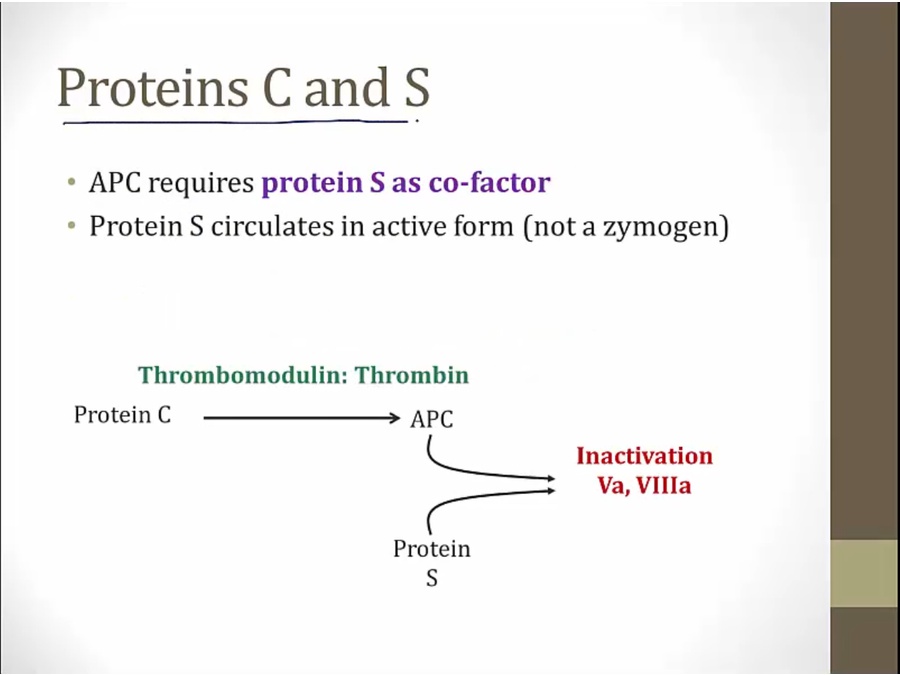
deficiency in one or both: hypercoagulable
factor 5 leiden mutation: cannot be inactivated by protein C/S: hypercoagulable

just know plasma level increased with heparin
Tissue factor pathway inhibitor (or TFPI) is a single-chain polypeptide which can reversibly inhibit Factor Xa (Xa). While Xa is inhibited, the Xa-TFPI complex can subsequently also inhibit the FVIIa-tissue factor complex. TFPI contributes significantly to the inhibition of Xa in vivo, despite being present at concentrations of only 2.5 nM.
Plaminogen

break down fibrin
converted to active in plasma

break up thrombus
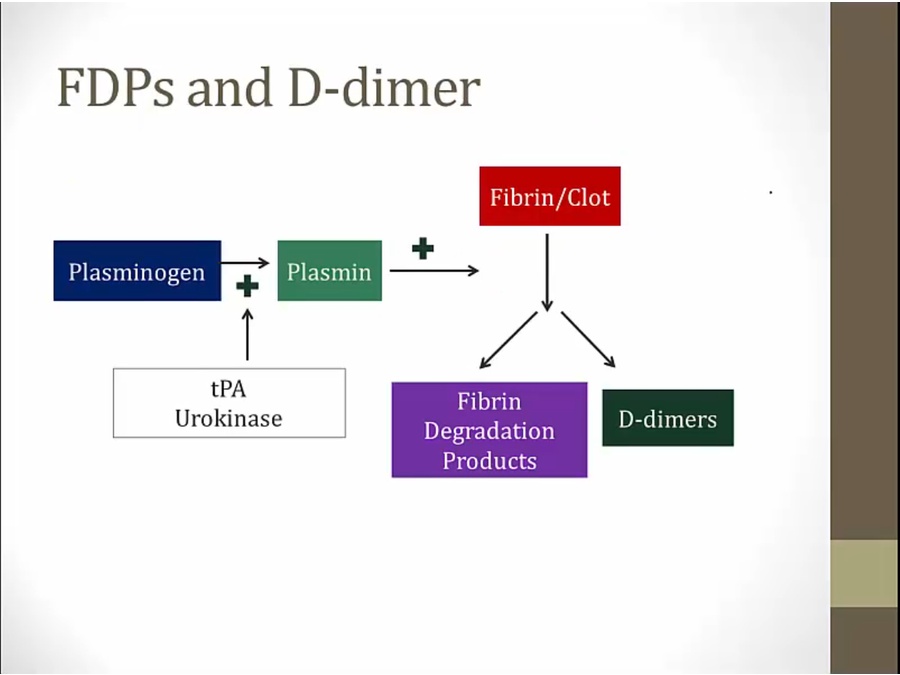


contain crosslinked bond by 13
indicates crosslinked fibrin clot broken down

FDP can increase without clot formation: not useful

break down of fibrinogen but not clot
break down other clotting factors: deplete clotting factors
looks like DIC
increased in prostate cancer and cirrhosis
alpha2- antiplasmin inhibitor of plasmin. Loss can leads to overactivation

Vitamin K

ESR

inflammation: increased protein levels
proteins are sticky, clump RBCs together, settle faster to bottom faster

liver makes more fibrinogen that will increase ESR
Last updated