13 ER
Airway
Patients who are unable to oxygenate their tissues require intubation.
Arterial oxygen saturation can be measured with the pulse oximetry.
Patients who are hypoxic act restless and agitated. They may eventually become cyanotic.
Patients who are unable to ventilate, and thus remove CO2 from their system, must be intubated.
Ventilation can be assessed with observed respirations and mental status.
Patients for whom a physician anticipates will soon need intubation should be intubated.
Patients who are unable to maintain or protect the airway require intubation.
Patients who are able to swallow secretions are adequately protecting their airway.
A patient who is able to phonate clearly and answer questions appropriately is adequately maintaining and protecting his or her airway.
Ectopic Pregnancy
Ectopic Pregnancy: Pregnancy occurring outside the uterus. Ectopic embryos will ultimately grow or invade underlying tissues, most commonly causing peritoneal rupture, leading to hemoperitoneum and acute abdomen.
Most often occurs in the ampulla of the fallopian tube. It can also occur in the ovary, peritoneal cavity, and cervix.
Risk factors:
Most common cause: Scarring from chronic salpingitis or PID
Other causes include: History of prior ectopic pregnancy and prior tubal surgery.
Heterotopic pregnancy: A multiple gestation with at least one intrauterine pregnancy and one ectopic pregnancy. The risk of this is small but increases with IVF if multiple embryos were used.
Clinical presentation
Sudden lower abdominal pain and/or vomiting (often mistaken for appendicitis)
Adnexal tenderness
Uterine bleeding > 6 weeks beyond LMP
Urine pregnancy test MUST be ordered, however, + result does NOT exclude appendicitis
Diagnosis
The first step in a patient with a suspected ectopic pregnancy is ultrasound. Transabdominal ultrasound is a reasonable first step, but transvaginal ultrasound may be necessary.
Possible ultrasound results are:
Non-diagnostic transabdominal ultrasound: No gestational sac seen, inside or outside of the uterus.
Perform transvaginal ultrasound.
Order a quantitative serum hCG. If serum hCG <1,500 then follow serial hCG levels (see below). If serum hCG >2,000 then ectopic pregnancy is likely. Remember that multiple gestations may also lead to elevated serum hCG.
Transabdominal or transvaginal ultrasound shows a viable intrauterine pregnancy, without evidence of a heterotopic (co-occurring ectopic) pregnancy: routine pregnancy care, evaluate for other possible causes of the patient's symptoms.
Transabdominal or transvaginal ultrasound findings suggestive of ectopic pregnancy:
The ring of fire is the classic finding on ultrasound, and describes the increased vascular flow to the adnexa when color Doppler is applied. Note: Similar findings occur with a well-developed corpus luteum, so be careful
No intrauterine pregnancy. Remember that a pseudogestational sac may be seen in cases of ectopic pregnancy.

Serial hCG is used to screen for suspected ectopic pregnancy:
hCG levels generally rise at a slower rate than a normal pregnancy.
Because of this, serum hCG levels can be compared to the normal if ectopic pregnancy is suspected.
Inappropriately low hCG levels → likely ectopic
Note: Inappropriately high hCG levels → molar pregnancy
Ectopic pregnancy may lead to destruction of the fallopian tube, and hypovolemic shock from intraperitoneal bleed (most common cause of hematosalpinx).
These pregnancies should not be considered viable - the fetus almost never survives.
Management:
If the ectopic pregnancy has ruptured, the first goal is to stabilize the patient with IV fluids, blood and pressors as needed before taking her to the operating room for exploratory laparotomy to stop bleeding and resect ectopic pregnancy.
If the woman has an unruptured ectopic and there is no fetal heartbeat, methotrexate is the treatment of choice.
Thoracic Outlet
Thoracic outlet syndrome is the compression of the neurovascular bundle at the thoracic outlet.
Causes of thoracic outlet syndrome include anomalous ribs, congenital cervical fibro-cartilagionous bands, muscular anomalies, and injury.
Neurogenic TOS
Venous TOS
Arterial TOS
Neurogenic thoracic outlet syndrome is due to brachial plexus compression. True neurogenic thoracic outlet syndrome is rare.
Venous thoracic outlet syndrome is due to subclavian vein compression.
Arterial thoracic outlet syndrome is due to subclavian artery compression.
Electrophysiological evaluation and imaging are used for diagnosis.
The first line imaging modality is usually arterial or venous duplex ultrasound. If that is unequivocal, CT or MRI should be ordered.
Management includes physical therapy, anticoagulation, embolectomy, and thoracic outlet decompression.
Surgery is indication only for patients who are symptomatic.
Symptoms depend on the type of thoracic outlet syndrome.
Patients with true neurogenic thoracic syndrome develop unilateral atrophic weakness in the intrinsic muscles of the hand. The thenar musculature is affected more than the hypothenar musculature is.
Venous TOS occurs in patients who uses an upper extremity repetitively. Swelling pain and cyanosis may be present in the affected extremity.
Arterial TOS is typically associated with a cervical or anomalous rib. Patients present with hand ischemia and pain, pallor, and paresthesia.
Subclavian Steal Syndrome
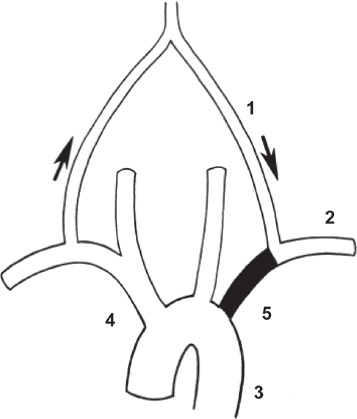
In subclavian steal syndrome, stenosis or occlusion of the proximal subclavian artery leads to reversal of blood flow through the ipsilateral vertebral artery.
The subclavian artery normally supplies blood to the upper extremity. One branch of the subclavian artery is the vertebral artery. If the proximal subclavian is obstructed, then blood will flow to the region of lowest pressure. Blood travels through the intracranial vasculature including the circle of willis and basilar artery. From the basilar artery it travels in a retrograde fashion through the vertebral artery and then to the distal subclavian artery (past the obstruction) and into the upper extremity. The subclavian artery is "stealing" blood from the vertebrobasilar system.
Arm ischemia
Exercise-induced pain
Fatigue
Coolness
Paresthesias
Vertebrobasilar ischemia
Dizziness
Vertigo
Ataxia
Dysequilibrium
Tinnitus
Hearing loss
Blurred vision
Diplopia
The primary physical exam finding of subclavian steal syndrome is >15 mmHg difference in pressure between upper extremities.
Diagnosis is done with continuous wave doppler, MRA, CTA, and contrast angiography.
Treatment for patients with symptomatic subclavian steal involves surgical revascularization of the affected area. The most common surgical procedures include carotid-subclavian bypass, carotid transposition, and percutaneous angioplasty with stenting.
Last updated