Psychopharmacology
Traditional Antidepressant
SSRI
Selective Serotonin Reuptake Inhibitors (SSRI's) include fluoxetine, sertraline, paroxetine, citalopram, escitalopram, and fluvoxamine. They work by inhibiting serotonin reuptake. They are used to treat many conditions, including:
Major depressive disorder
Obsessive compulsive disorder
Bulimia nervosa
Panic disorder
Diabetic neuropathy associated pain
Premenstrual dysphoric disorder
GAD
PTSD
SSRI's normally require 4-6 weeks for treatment effect.
In the treatment of major depressive disorder, SSRI's are the first line treatment. If no response occurs after 2-4 weeks of treatment, a second SSRI should be attempted. If there is still no response, then a different class of antidepressant may be trialed.
The most common side effect of SSRI's is GI upset. Other common side effects include sedation, weight gain, and sexual dysfunction (impotence, decreased libido, erectile dysfunction).
Fluoxetine
Has the longest half life with active metabolites; therefore, it does not need to be tapered because of a low risk of SSRI discontinuation syndrome (a phenomenon characterized by headaches, dizziness, nausea, and malaise).,
Sertraline
Is the most likely SSRI to cause GI disturbances.,
TCA
Tricyclic antidepressants (TCAs) are heterocyclic compounds that inhibit the reuptake of norepinephrine and serotonin. They include the following drugs:
Imipramine
Amitriptyline
Clomipramine
Doxepin
Desipramine
Nortriptyline
Amoxapine
TCAs are used as second-line medications to treat major depressive disorder. They also have multiple other uses, including treatment of migraines, chronic pain, and fibromyalgia. TCAs are classically tested for use in diabetic neuropathy, but pregabalin and gabapentin may be more frequently used.
Clomipramine can be used in obsessive compulsive disorder. However, SSRI's are 1st line in OCD.
Imipramine
Can be used as a treatment for bed wetting in children older than 6 years old by causing contraction of the internal sphincter of the bladder secondary to anticholinergic effects and stimulation of ADH secretion.,
Amoxapine
Can be used in MDD with psychotic features because it is metabolized into 2 active metabolites: one that inhibits reuptake of norepinephrine (an antidepressant effect) and another that blocks dopamine receptors in the CNS (an antipsychotic effect).,
SE
Side effects of TCA's can be grouped into the following clusters of side effects based on non-therapeutic inhibition of receptors:
Antihistaminic (sedation and weight gain)
Antiadrenergic (orthostatic hypotension and arrhythmias)
Anticholinergic (dry mouth, tachycardia, confusion, constipation, and urinary retention)
Serious adverse effects of TCAs include:
3 C's:
Convulsions
Coma
Cardiotoxicity (due to blockade of fast Na+ channels)
Respiratory depression
Hyperpyrexia
Suspect TCA overdose in a question regarding a patient with a history of depression presenting with anticholinergic signs and ECG abnormalities (e.g. prolonged QRS interval). The patient will likely have an altered mental status as well, though this is a relatively nonspecific finding in suspected overdose.
Sodium bicarbonate is the mainstay of treatment for TCA-related cardiotoxicity. It is indicated in patients with a QRS interval >100 msec, a ventricular arrhythmia, or hypotension.
Sodium bicarbonate treats TCA-related cardiotoxicity by:
Alkalizing the plasma, which reduces the binding of TCAs to fast sodium channels
Increasing extracellular sodium, which increases the electrochemical gradient across cardiac cells and reduces the efficiency of TCA-induced fast sodium channel inhibition
Due to their cardiotoxicity, TCA's should be used cautiously in patients with risk of arrhythmia. Conduction abnormalities on ECG are a contraindication for use of a TCA.
TCAs are lethal in overdose. One must assess suicide risk before prescribing TCA's because a 1-week supply is all that is necessary for lethality.
The USMLE commonly tests this antidepressant class in questions centering around a patient having undergone a suicide attempt. Suspect these medications when asked to identify the causative agent based on symptoms, or in a patient whose suicide attempt quickly followed a recent prescription for depression.
Atypical Antidepressant
Bupropion
Bupropion is an atypical antidepressant that is also used as an aid for smoking cessation. It primarily acts as a reuptake inhibitor of dopamine and norepinephrine.
Since bupropion is a mild stimulant, it can also help to facilitate weight loss in obese patients.
Bupropion carries a risk of seizures and should be avoided in patients who are susceptible to seizures. These patient populations include:
Bulimics (electrolyte imbalance)
Epileptics
Abstaining alcoholics (risk of delirium tremens)
Adverse effects of bupropion include:
Stimulant effects (tachycardia, insomnia, increased BP)
Headache
Seizures
Note that many of the stimulating effects can be beneficial in depressed patients with obesity, hypersomnia, and poor concentration.
Unlike other antidepressants, bupropion does not cause weight gain or sexual dysfunction.
Mirtazapine
Mirtazapine is an atypical antidepressant that acts by antagonizing α2 and serotonergic receptors.
Its two most important side effects are sedation and weight gain. These are often used advantageously, in patients who have trouble sleeping or who are unhealthily underweight.
Trazodone and Nefazodone
Trazodone and nefazodone are atypical antidepressants that act by antagonizing serotonin and α1 receptors (trazodone more than nefazodone) and weakly inhibit serotonin reuptake.
With the discovery and exploration of antidepressants, trazodone has fallen out of use as an antidepressant. Instead, its side effect of sedation is used advantageously to the extent that it is more frequently used as a sleeping aid (particularly in patients with substance abuse or sedative tolerance).
A frequently-tested side effect of trazodone is priapism (think trazoBONE). For this reason, it is relatively contraindicated in adolescent males.
The treatment for unremitting priapism is phenylephrine injection into the corpora cavernosa. Epinephrine and other sympathomimetics may also be used.
Nefazodone
Carries a black-box warning for rare but serious hepatotoxicity.,
SNRI
Venlafaxine and duloxetine are antidepressants of the serotonin-norepinephrine reuptake inhibitor (SNRI) class.
In addition to depression, venlafaxine can also be used to treat generalized anxiety disorder (GAD).
In addition to depression, duloxetine can also be used to treat neuropathies and fibromyalgia.
Venlafaxine
Venlafaxine can increase blood pressure; avoid using it in patients with elevated or labile blood pressure.,
MAOI
Nonselective MAO inhibitors (phenelzine, tranylcypromine, isocarboxazid) perform nonselective MAO inhibition (inhibit both MAOA and MAOB) leading to increased levels of norepinephrine, dopamine, and serotonin.
MAO inhibitors are not used as first-line agents but can instead be used to treat atypical depression.
Signs of atypical depression include labile mood, sensitivity to rejection, leaden paralysis, hypersomnia, and increased appetite.
Note: Do not confuse nonselective MAO inhibitors (e.g. phenelzine) with selective MAO inhibitors (e.g. selegiline, rasagiline), which perform selective irreversible MAOB inhibition leading to increased levels of dopamine. Selegiline and rasagiline are used in Parkinson’s disease.
Hypertensive crisis occurs when MAO inhibitors are used while eating foods that are digested to form tyramine (aged cheeses, chicken liver, beer, and red wines). Large amounts of stored catecholamines are released resulting in headaches, tachycardia, nausea, hypertension, cardiac arrhythmias, and stroke. No hyperthermia.
See the pheochromocytoma topic for more information on the management of hypertensive crisis.
Mood stabilizers
Lithium
Lithium is used in maintenance therapy and prophylaxis of bipolar disorder. It may also be used in cyclothymia and major depression. It is the only mood stabilizer shown to decrease suicidality.
Lithium can lead to the development of nephrogenic diabetes insipidus.
Lithium can lead to the development of hypothyroidism.
Lithium can lead to the development of hypercalcemia. The mechanism of this includes development of a parathyroid adenoma, development of parathyroid hyperplasia, or direct effect of lithium on the renal tubules.
When possible, lithium should not be used in pregnancy due to an increased risk of Ebstein’s cardiac anomaly. Ebstein's anomaly is the "atrialization" of the right ventricle of the heart, due to a downward displacement of the tricuspid valve.
Lithium therapy requires a close monitoring of serum levels due to narrow therapeutic range. Signs of lithium toxicity include GI distress, tremors, acne, and edema.
Serum lithium levels are tightly coupled to salt and water balance and renal function. Lithium concentration and the possibility of lithium toxicity increase in the following clinical conditions:
Hypovolemia
Salt deprivation
Impaired renal function (elderly patient with low GFR)
Important medications that can cause lithium toxicity are thiazides, NSAIDs, and ACE inhibitors.
Prior to initiating therapy, patients should have the following tests to establish baseline functioning and anticipate toxicity:
Urinalysis, serum blood urea nitrogen (BUN), serum creatinine
Thyroid function studies
Serum calcium
Pregnancy test for women of childbearing potential
Electrocardiogram (ECG)(for patients at risk of cardiac disease)

Renal, thyroid, and parathyroid function should monitoring at the following intervals:
UA, BUN, and creatinine 2-3x for the first 6 months of therapy, and every 6-12 months thereafter
Thyroid function tests 1-2x for the first 6 months, and every 6-12 months thereafter
Serum calcium once a year
The preferred treatment of severe lithium toxicity is hemodialysis, which is effective due to the small molecular weight and small volume distribution of lithium. While unlikely to be tested, the indications for dialysis are
Serum levels of >4 mEq/L, OR
Serum levels of >2.5 mEq/L in the setting of renal insufficiency or heart failure
Others
Carbamazepine, valproic acid, and lamotrigine are other important mood stabilizers. See the corresponding topics below for more information on these medications.
Carbamazepine
Valproic acid
Lamotrigine
FGA
MOA
Traditional/Typical antipsychotics (neuroleptics) are used to treat psychotic disorders and psychotic symptoms by blocking dopamine D2 receptors. The therapeutic effect is mediated by blockade of the mesolimbic dopaminergic pathway. Typical blocks all 4 dopamine pathways.
Traditional antipsychotics are used to treat primarily the positive symptoms of schizophrenia. They can also be used to treat other psychoses, acute mania, and Tourette’s disorder.
Undesirable blockade of the tuberoinfundibular dopaminergic pathway results in increased prolactin and its endocrine side effects. These include gynecomastia, impotence, amenorrhea, and decreased libido.
Undesirable blockade of the nigrostriatal dopaminergic pathway results in the motor manifestations of extra-pyramidal symptoms (EPS).
Blockade of mesocortical pathway results in worsening negative symptoms.
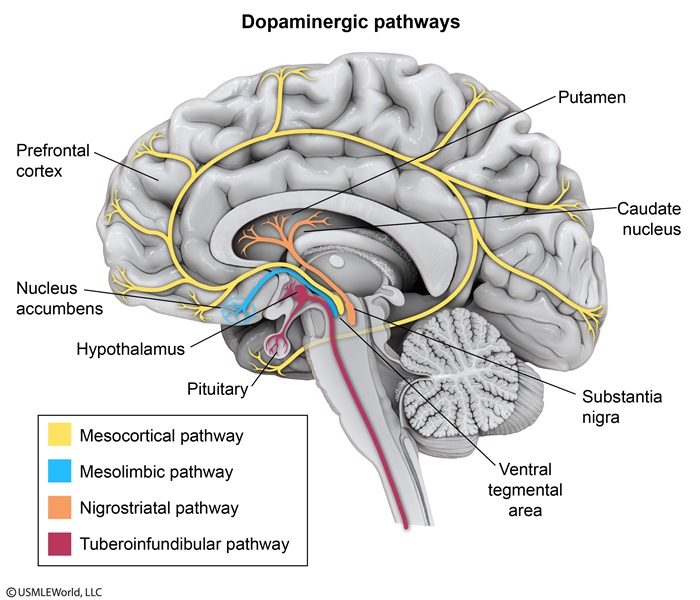

Increased dopamine activity in the mesolimbic pathway accounts for the euphoria accompanying drug use as well as the delusions and hallucinations experienced by patients with schizophrenia.
Increased dopamine activity in the nigrostriatal pathway is thought to be involved in movement disorders such as chorea and tics.
High Potency
Haloperidol, trifluoperazine, and fluphenazine are high-potency traditional antipsychotics.
Mnemonic: An angel with a halo will tri to fly high.
The most notable side effects of high-potency antipsychotics are extra-pyramidal symptoms (EPS).
Intramuscular high-potency antipsychotics are the treatment of choice for acute delirium and agitation in the elderly.
Benzodiazepines are contraindicated in the delirious elderly and may result in paradoxical worsening of delirium.
Non-compliance is an important indication for the use of depot versions (long-acting, injectable decanoate compounds) of high-potency traditional antipsychotics.
Patients may be described as repeatedly necessitating hospitalization, but responding well once hospitalized.
Low potency
Low-potency antipsychotics include chlorpromazine and thioridazine.
Mnemonic: Cheating Thieves are low.
The most notable side effects of low-potency antipsychotics are non-neurological. Low-potency antipsychotics are less potent at inhibiting dopamine receptors, and therefore lose relative specificity for the dopamine receptor as opposed to other receptors.
Anticholinergic side effects: Dry mouth, tachycardia, urinary retention, constipation
Antihistaminic side effects: Sedation, weight gain
Anti-α1 adrenergicside effects: Orthostatic hypotension, cardiac abnormalities
Chlorpromazine may cause Corneal deposits and blue-gray skin disColoration.
Thioridazine can cause irreversible reTinopathy, resembling retinitis pigmentosa. This side effect may manifest as night blindness.
SE

The extrapyramidal symptoms associated with high-potency antipsychotics occur in a predictable time frame (mnemonic: ADAPT):
Hours - days: Acute Dystonia: sustained painful contraction of neck, tongue, and oculogyric crisis
Days - months: Akathisia (restlessness), Parkinsonism (masked facies)
Months - years: Tardive dyskinesia: choreoathetoid (writhing) involuntary movements of mouth and tongue

The first-line management for akathisia, the most common form of extrapyramidal symptoms, is cautious dosage reduction of the offending agent.
If akathisia does not resolve with dosage reduction or if dosage reduction is not possible, first-line agents for the treatment of akathisia include:
Beta blockers (e.g. propranolol)
Benztropine, a muscarinic antagonist
Benzodiazepines (e.g. lorazepam) are second-line agents for the treatment of akathisia.
The key step in clinical management of tardive dyskinesia is discontinuing the traditional antipsychotic and switching to an atypical antipsychotic(e.g. quetiapine or clozapine).
Localized forms of tardive dystonia, such as cervical dystonia, retrocollis, and torticollis, may be treated with botulinum toxin injections.
The pathophysiology of TD is thought to involve D2 receptor upregulation and supersensitivity resulting from chronic blockade of dopamine receptors. When dopamine D2 receptor blockade is reduced, an exaggerated response of the D2 receptor (even to low concentrations of dopamine) may result in a variety of hyperkinetic movements.
SGA
Atypical antipsychotics are used to treat both positive and negative symptoms of schizophrenia.
Contrast this to typical antipsychotics, which primarily treat the positive symptoms of schizophrenia.
Most atypical antipsychotics are dopamine(D2) antagonists. Atypical antipsychotics can also variably modulate α1, H1, and 5-HT2 receptors. 5HT blockade gives SGA selectivity.
Atypical antipsychotics are a class of psychogenic medications which can be remembered by the mnemonic, "It's Atypical for OLd CLOsets to QUietly RISPER from A to Z."
OLanzapine
CLOzapine
QUetiapine
RISPERidone
Aripiprazole
Ziprasidone
The side effect profile of atypical antipsychotics is notable for having fewer EPS and anticholinergic side effects than traditional antipsychotics. As such, part of the management of tardive dyskinesia is switching from a typical to an atypical antipsychotic.
aripiprazole
In contrast to other atypical antipsychotics, which are dopamine (D2) antagonists, this is a partial agonist at D2 receptors.,
Olanzapine
Olanzapine can be used for obsessive compulsive disorder (OCD).
A notable side effect of olanzapine is metabolic syndrome (hyperlipidemia, glucose intolerance, and weight gain).
A notable side effect of risperidone is hyperprolactinemia manifesting in any of the following:
Gynecomastia (in males)
Impotence (in males)
Galactorrhea
Amenorrhea (in females)
In contrast to lactotroph adenomas (prolactinomas), which can increase serum prolactin >200 ng/mL, serum prolactin levels in drug-induced hyperprolactinemia (e.g. by risperidone) rarely exceed 200 ng/mL.
Ziprasidone
Ziprasidone prolongs the QT interval (all atypical antipsychotics have the potential to increase QT interval, however ziprasidone is most likely to have this specific side effect).,
Clozapine
Is the only atypical antipsychotic that has actually been shown to be more efficacious than other antipsychotics.
Is the only antipsychotic shown to reduce suicide attempts in patients with schizophrenia and schizoaffective disorder at high risk for suicide.,
Clozapine carries a dose-dependent risk of seizures.
Clozapine is associated with agranulocytosis and requires monitoring of WBC counts. If agranulocytosis develops, clozapine must be immediately discontinued.
Mnemonic: Must watch CLOZapine CLOZely!
Clozapine is associated with hypersalivation and myocarditis. It is also associated with weight gain.
Due to risk of agranulocytosis and seizures, clozapine is reserved for severe schizophrenic symptoms refractory to traditional therapy. Use if nonresponsive to two or more other antipsychotics.
Quetiapine
Associated with cataracts; therefore, periodic slit lamp examination is recommended.,
Mnemonic: Quetiapine is associated with Quataracts.
Diabetes
ziprasidone, aripripazole
Sedatives
Benzos
Benzodiazepines (e.g. diazepam, lorazepam, midazolam, chlordiazepoxide) potentiate the effect of GABA by increasing the frequency of chloride channel opening. Therefore, these drugs are ineffective in the absence of GABA.
Toxicity of benzodiazepines primarily involves sedation and respiratory depression.
The treatment of benzodiazepine toxicity is flumazenil, a competitive antagonist at GABA receptor. Flumazenil has a short half-life and has no effect in the absence of benzodiazepines.
As people age, they metabolize benzodiazepines more slowly and are more likely to experience confusion and increased risk of falls. Another adverse effect of benzodiazepines is paradoxical agitation, which is suggested by this patient's recurrent episodes of confusion and agitation shortly after taking his alprazolam dose. Paradoxical agitation is characterized by increased agitation, confusion, aggression, and disinhibition, typically within an hour of administration. Although paradoxical reactions to benzodiazepines are relatively uncommon (<1%), they are important to recognize as increasing the dose of the benzodiazepine will only worsen the patient's condition.
"When he emerged an hour later, he was agitated, irritable, and confused. When asked what was wrong, he became belligerent and seemingly unable to recognize some family members."
Many drugs of abuse cause withdrawal symptoms of varying discomfort or pain, but only sedative-hypnotics (alcohol, benzodiazepines, and barbiturates) cause a life-threatening withdrawal syndrome.
Benzodiazepines (e.g. diazepam or lorazepam) are first line agents for sedative-hypnotic withdrawal (including withdrawal from benzodiazepines themselves), as well as for status epilepticus.
The following benzodiazepines are appropriate for patients with liver disease because they are minimally metabolized in the liver (mnemonic: LOT):
Lorazepam
Oxazepam
Temazepam
Chlordiazepoxide used for withdrawal but not acutely in hospital and not for pt's with liver disease
Short acting benzodiazepines include (mnemonic: ATOM):
Alprazolam
Triazolam
Oxazepam
Midazolam
Short-acting benzodiazepines have a higher addictive potential and are most likely to cause seizures upon abrupt cessation.
Clonazepam
Should be avoided in patients with renal dysfunction.,
Nonbenzo hypnotics and anxiolytics
Non-benzodiazepine anxiolytics include:
1st generation anti-histamines
Buspirone
Propranolol
Barbiturates
Barbiturates are not used frequently due to their narrow therapeutic window; lethal overdose from significant respiratory depression is the most notable adverse effect.
1st generation anti-histamines (hydroxyzine, diphenhydramine) can be utilized for their sedative side effects in patients that cannot or should not use benzodiazepines. (e.g. drug abuse, drug tolerance)
Buspirone
Buspirone is an 5HT1a partial agonist.
Buspirone is anxiolytics/sedative useful in alcoholics because it does not potentiate CNS depression.
Buspirone does not work immediately; it takes 1-2 weeks to take effect. As such, buspirone can not be used as an as-needed anxiolytic/sedative.
Zolpidem
Zolpidem, zaleplon, and eszopiclone are sleep aids that are GABAA agonists. Because they act on the same receptor as benzodiazepines, tolerance and dependence are still possible.
Ramelteon
Ramelteon is a selective MT1 and MT2 (melatonin receptor) agonist used as a sleep aid. It exhibits no tolerance or dependence.
Neurotransmitter
Schizo
The neurotransmitter changes include:
Mesolimbic pathway (positive symptoms): ↑ dopamine
Mesocortical pathway (negative symptoms): ↓ dopamine.,
Alzheimer
The neurotransmitter changes include:
↓ acetylcholine.,
Recall that the primary ameliorative treatment for Alzheimer's dementia is acetylcholinesterase inhibitors, which produce a cholinergic type effect.
Parkinson
The neurotransmitter changes include:
↓ dopamine
↑ acetylcholine.,
Recall that the pathophysiology of Parkinson's is an increased acetylcholine:dopamine ratio in the basal ganglia, in the pathways in which acetylcholine is inhibitory and dopamine is excitatory.
Huntington
The neurotransmitter changes include:
↑ dopamine
↓ GABA
↓ acetylcholine.,
Consider the neurotransmitter changes of Huntington's disease as "dementia + spasticity". As with Alzheimer's, decreased acetylcholine is associated with Huntington's disease. Spasticity and stereotyped movements that exemplify the disease can be correlated to increased dopamine in the basal ganglia, and decreased inhibitory transmission from decreased GABA.
Anxiety
The neurotransmitter changes include:
↑ norepinephrine
↓ GABA
↓ serotonin.,
Anxiety is a state of stress and pathologically heightened sensorium. Elevated norepinephrine and decreased GABA (decreased inhibitory neurotransmission) correlate with this. Serotonin is typically decreased in states of depression and anxiety, contributing to the logical basis for why these disorders' first-line medications are SSRIs.
Depression
The neurotransmitter changes include:
↓ norepinephrine
↓ serotonin
↓ dopamine.,
Depression is associated with decreased energy and anhedonia. Associate decreased norepinephrine with decreased energy, and decreased serotonin and dopamine with anhedonia.
Serotonin Syndrome and NMS
Serotonin syndrome
Serotonin syndrome occurs when SSRIs are co-administered with any drug that can increase serotonin levels. The following medications have been implicated in serotonin syndrome:
Antidepressants: SSRIs, TCAs, and MAOIs
Ondansetron
Triptans (e.g. sumatriptan)
Tramadol
Linezolid
Meperidine
Mnemonic: Any Of These Treatments Love Myoclonus
The manifestations of serotonin syndrome include (mnemonic: HARMED):
Hyperthermia
Autonomic instability
Rash (flushing)
Myoclonus
Encephalopathy
Diarrhea
The treatment of serotonin syndrome includes:
Cessation of offending medications (i.e. serotonergic agents)
Sedation with benzodiazepines (e.g. lorazepam)
Supportive care: oxygen, IV fluids, cardiac monitoring
If benzodiazepines and supportive care fail, administer cyproheptadine
NMS
Neuroleptic malignant syndrome (NMS) is a serious toxicity of antipsychotic medications that can occur at any length of treatment. Traditional/typical high-potency antipsychotics (e.g. haloperidol, fluphenazine) are more likely to cause NMS than atypical antipsychotics. The following characteristics are observed:
Fever
Encephalopathy
Vitals unstable
Elevated creatine kinase and WBCs
Rigidity of muscles
Think FEVER.
The initial treatment of mild neuroleptic malignant syndrome is discontinuation of the offending agent and supportive care.
Patients who do not respond to supportive care or who present with severe neuroleptic malignant syndrome (e.g. elevated CK, hyperthermia) are candidates for treatment with dantrolene, bromocriptine, and/or amantadine.
Serotonin syndrome and neuroleptic malignant syndrome have significant overlap in clinical presentation and can be difficult to distinguish in the setting of polypharmacy.
While both syndromes can have rigidity and clonus, these signs have diagnostic utility.
Neuroleptic malignant syndrome: More likely to have muscularrigidity
Serotonin syndrome: More likely to have hyperreflexia and clonus
While both syndromes can exhibit rhabdomyolysis, the presence of significantly elevated creatine kinase is indicative of neuroleptic malignant syndrome.
Findings of GI distress such as nausea, vomiting, and diarrhea are more likely in the setting of serotonin syndrome.
ECT
Unipolar & bipolar depression
Catatonia
Bipolar mania/psychosis
treatment resistance
Psychotic features present
Emergency conditions
Refusal to eat or drink
Imminent risk for suicide
Pharmacotherapy contraindicated due to comorbid medical illness or poor tolerability
Pregnancy when pharmacotherapy is undesirable or ineffective
History of ECT response
No absolute contraindications
Increased risk
Severe cardiovascular disease, recent myocardial infarction
Space-occupying brain lesion
Recent stroke, unstable aneurysm
SE: amnesia most common
Last updated