Uworld Neuro Notes
Lumbar Spinal Stenosis
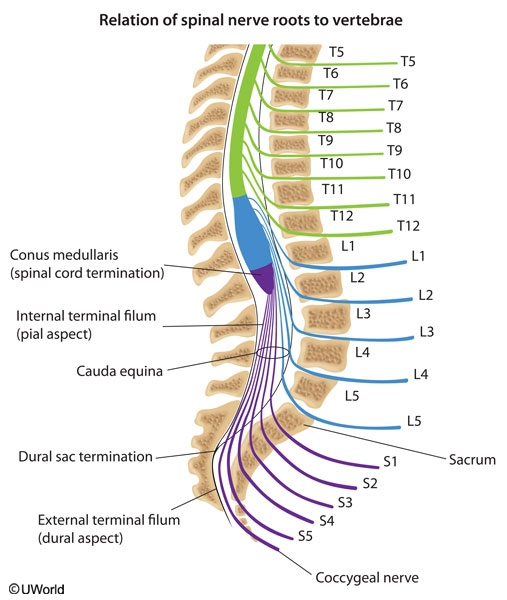
path: may result from any condition that narrows the spinal canal and compresses nerve roots. The most common cause is degenerative joint disease (DJD). In DJD, disc herniation and facet osteophytes impinge upon the spinal cord.
demographics: This is most commonly seen in middle-aged and elderly patients.
Symptoms: flexion of the spine causes widening of the spinal canal, while extension causes narrowing of the canal. Therefore, the symptoms of lumbar spinal stenosis are exacerbated by extension of the spine (e.g. standing and downhill walking), and improved by flexion of the spine (e.g. sitting and uphill walking). Weakness, sensory loss, numbness/tingling, and discomfort of the legs may all be seen. Neurologic examination may be entirely normal and only 10% of patients have a positive straight leg test.
Diagnosis: The diagnosis is confirmed radiologically. MRI demonstrates bony anatomy, neural structures, and soft tissue, making it the study of choice for suspected lumbar spinal stenosis.
PVD: Ankle-brachial index measurements are performed to evalutate peripheral vascular disease (PVD). PVD presents with leg and buttock pain that are worse with activity and relieved by rest. On the other hand, the pain of spinal stenosis is posture-dependent, persisting when standing but improving when walking uphill. Furthermore, this patient has 2+ dorsalis pedis pulses.
Ankylosing Spondylitis: There is a strong association between HLA-B27 and ankylosing spondylitis (AS). AS presents in young males (aged 15-30 years) and symptoms include low back pain with limited spinal mobility. Symptoms improve with exercise early in the disease.
Gait Disorders
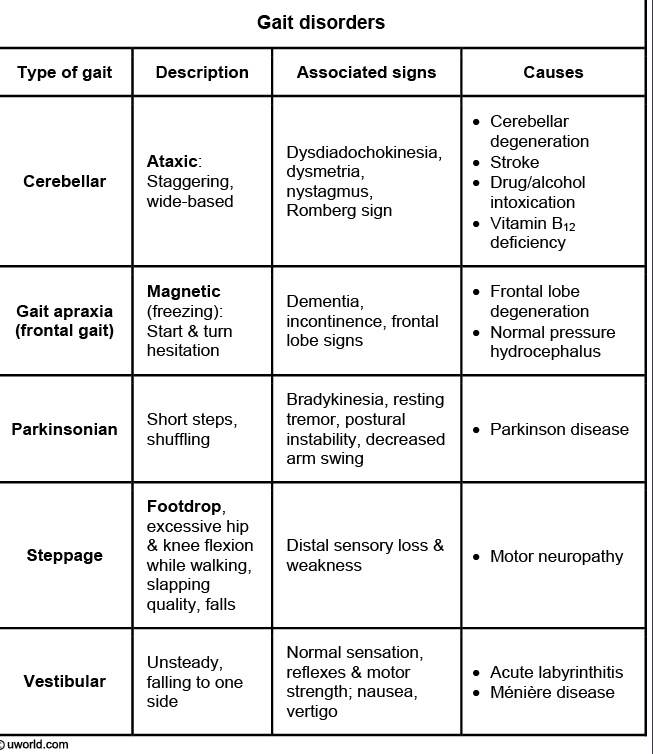
Steppage gait is most commonly caused by L5 radiculopathy or neuropathy of the common peroneal nerve. L5 radiculopathy is typified by back pain radiating to the foot, often with weakness of foot inversion and plantar flexion. Peroneal neuropathy is due to compression of the nerve at the lateral aspect of the fibula (eg, due to prolonged crossing of the legs or squatting) and is associated with paresthesias and sensory loss over the dorsum of the foot but normal foot inversion and plantar flexion. The diagnosis can be clarified with electromyography and nerve conduction studies.
Lesions in the basal ganglia can present with a slow shuffling gait as seen in patients with Parkinson's disease.
(Choice B) Cerebellar ataxia can result from lesions of the vermis (truncal ataxia) or the cerebellar hemispheres (limb ataxia). Features of cerebellar ataxia include staggering and swaying from side to side, impaired tandem gait and titubation (truncal tremor).
(Choice D) Pyramidal tract or corticospinal tract (CST) lesions can cause spastic ataxia. The gait appears stiff or rigid with circumduction (the spastic leg is abducted and advanced while in extension and internal rotation) and plantar flexion of the affected limb.
(Choice E) Damage to the cortico-cortical white matter fibers of the frontal lobe, as seen in normal pressure hydrocephalus, can lead to gait apraxia (Bruns ataxia). Strength, coordination, and sensory functions are intact, but there is difficulty in initiation of forward movement of the feet when they are in contact with the ground ("magnetic gait").
(Choice F) Patients with loss of proprioception due to sensory neuronopathy may have postural or gait instability and a wide-based gait. Patients may stomp their feet against the floor (slap gait) to help them know where their lower limbs are relative to the ground.
vestibular ataxia: Vestibular ataxia results in an en-bloc gait, with minimal movements of the head during walking. It is typically a staggering gait, and is accompanied by vertigo and nystagmus.
waddling gait: Muscular dystrophy results in a waddling gait owing to weakness of the gluteal muscles.
Spinal Cord Compression
Causes: Possible etiologies for spinal cord compression are disk herniation, abscess, and malignancy. An epidural abscess (even without fever) is of particular concern in IV drug abusers.
Symptoms: Isolated, symmetric lower-extremity symptoms, including loss of sensation, and signs of upper motor neuron disease. Signs of an upper motor neuron lesion include weakness without fasciculations, hyperreflexia, and positive Babinski sign. The presence of upper motor neuron symptoms indicates involvement of the central nervous system. Because the symptoms are bilateral and present only in the lower extremities, the lesion can be localized to the spinal cord.
Diagnosis: Spinal cord compression is a medical emergency and must be evaluated immediately with an MRI of the spine. Lumbar puncture is not recommended when there may be an epidural abscess as bacteria can be introduced into the spinal fluid.
Hypokalemia Neuropathy
Symptoms of hypokalemia depend on the severity of the imbalance, but can include weakness, fatigue, and muscle cramps. Flaccid paralysis, hyporeflexia, tetany, rhabdomyolysis, and arrhythmias may occur with severe hypokalemia (serum concentration <2.5 mEq/L). An ECG will show broad flat T waves, U waves, ST depression, and premature ventricular beats. Atrial fibrillation, torsades de pointes, and ventricular fibrillation can occur. This woman is taking a potassium-wasting diuretic, which is the most likely cause of her hypokalemia. Other common causes include diarrhea, vomiting, anorexia, and hyperaldosteronism. This patient's symptoms should resolve with potassium supplementation.
Glioblastoma
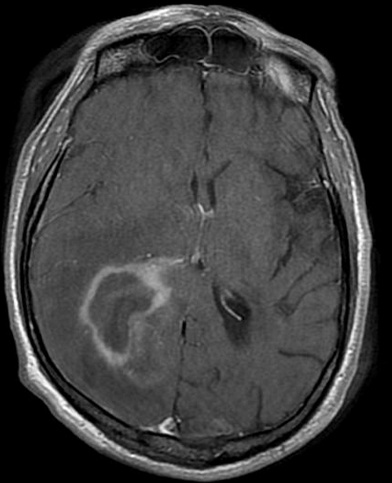
Glio: The CT/MRI findings of a butterfly appearance with central necrosis is classic for GBM, and the heterogenous, serpiginous contrast enhancement is typical of high-grade.
Patients with brain abscess usually have fever, acute onset of symptoms and evidence of a systemic infectious process. On neuroimaging, there is uniform contrast enhancement.
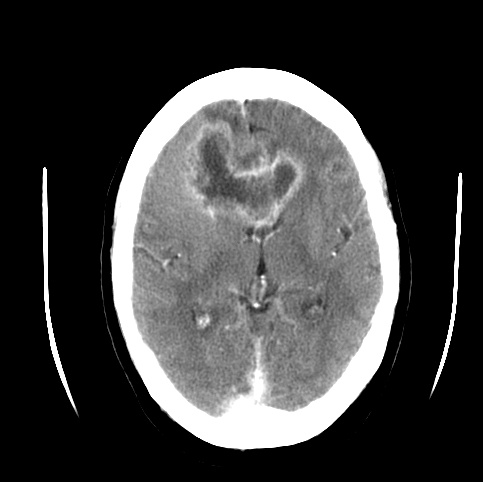
Diffuse Axonal Injury
It is frequently due to traumatic deceleration injury and results in vegetative state as in this patient. Sudden acceleration-deceleration impact produces rotational forces that affect the brain areas where the density difference is the maximum, thus most of the diffuse axonal injury occur at gray white matter junction.
CT scan characteristically shows numerous minute punctate hemorrhages with blurring of grey white interface.
Pseudodementia vs Alzheimers
A key distinguishing factor is that patients with pseudodementia are frequently distressed by their impaired memory; those with Alzheimer dementia are often relatively unconcerned and confabulate.
Ulnar compression
most common compression site at medial epicondyle at elbow
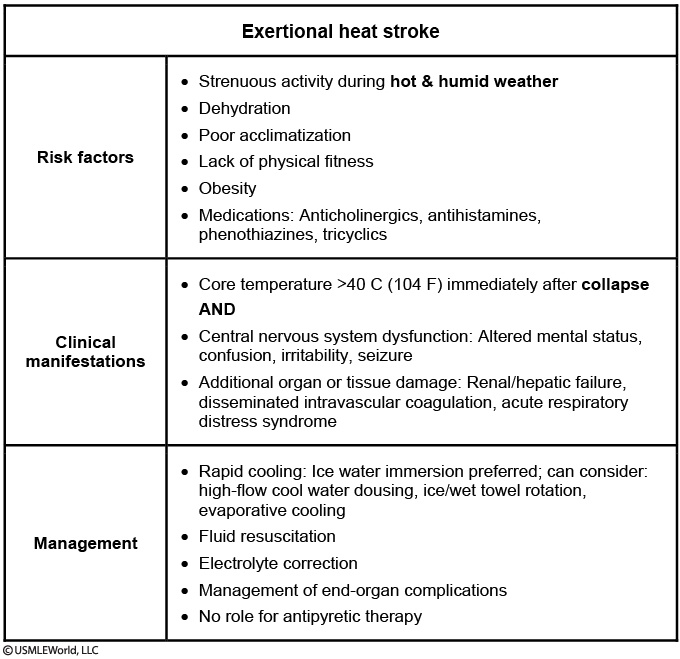
Heat stroke
in direct sunlight for hours
core temp > 40 degrees, tachycardia, and altered mental status
Complications of heat stroke include rhabdomyolysis, renal failure, ARDS, and coagulopathic bleeding. Coagulopathic bleeding explains this patient’s persistent epistaxis.
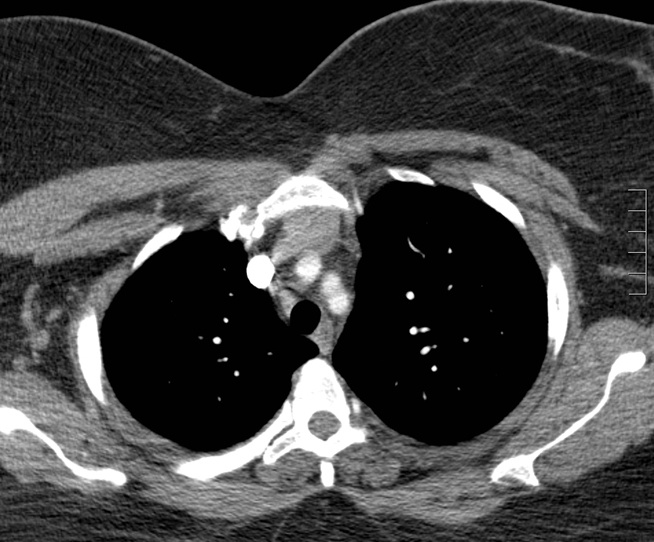
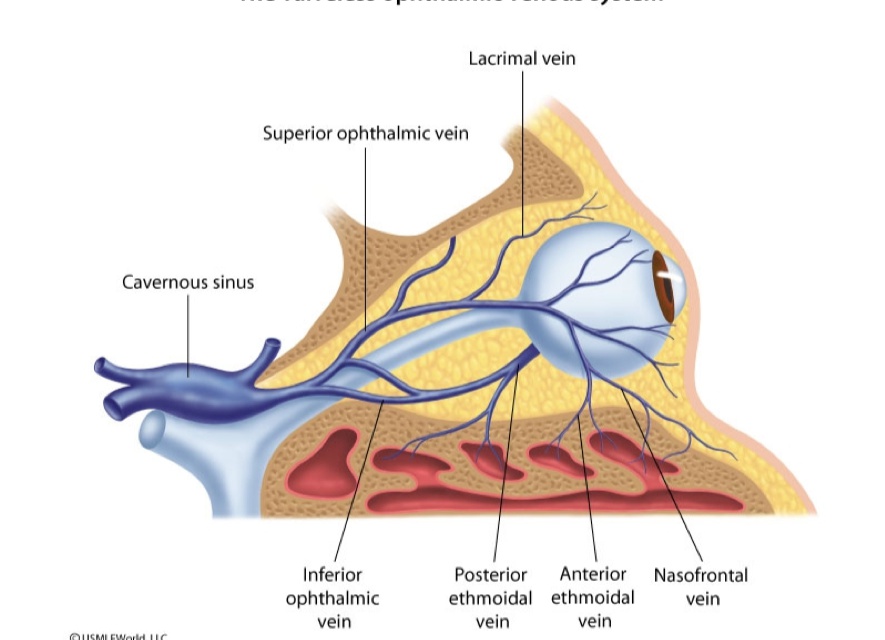
Cavernous Sinus Thrombosis
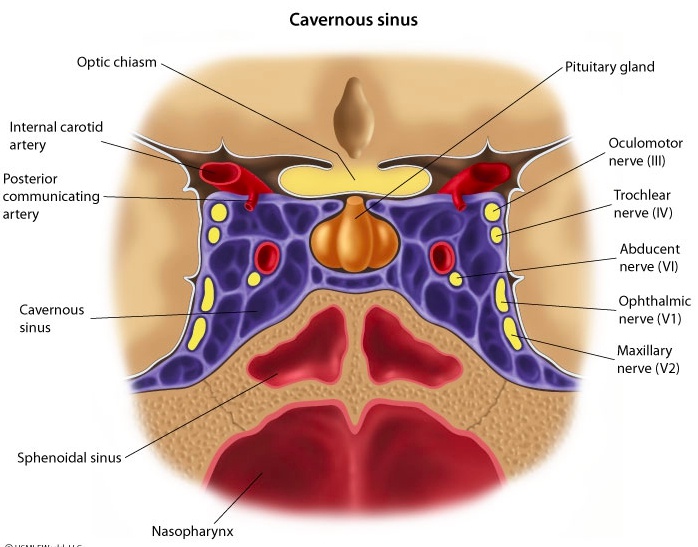
Cause: Because the facial/ophthalmic venous system is valveless, uncontrolled infection of the skin, sinuses, and orbit can spread to the cavernous sinus.
Symptoms; Inflammation of the cavernous sinus subsequently results in life-threatening CST and intracranial hypertension. Headache is the most common symptom and can become intolerable. A low-grade fever and periorbital edema usually occur several days later secondary to impaired venous flow in the orbital veins. Vomiting is also a result of intracranial hypertension, and fundoscopy may reveal papilledema.
Cranial nerves III, IV, V, and VI pass through the cavernous sinus, which has anastomoses crossing midline. As a result, unilateral symptoms (eg, headache, binocular palsies, periorbital edema, hypoesthesia, or hyperesthesia in V1/V2 distribution) can rapidly become bilateral. Magnetic resonance imaging with magnetic resonance venography is the imaging modality of choice for diagnosis of CST. Treatment includes broad-spectrum intravenous antibiotics and prevention or reversal of cerebral herniation.
case: A 23-year-old man comes to the physician complaining of worsening headache over the past week. He is "under a lot of stress at school" and having trouble sleeping because the headache is constant. Two weeks ago, he had an insect bite on his right cheek and now both of his eyes are swollen. He also has lost his appetite and vomited twice today. His temperature is 38.3° C (101° F), blood pressure is 130/90 mm Hg, pulse is 104/min, and respirations are 20/min. Examination shows erythema and swelling of the right cheek and bilateral eyelid edema, right greater than left. Bilateral extraocular movements are restricted. The bilateral forehead and mid-face are extremely tender to light palpation. Which of the following is the most likely diagnosis?
GIM
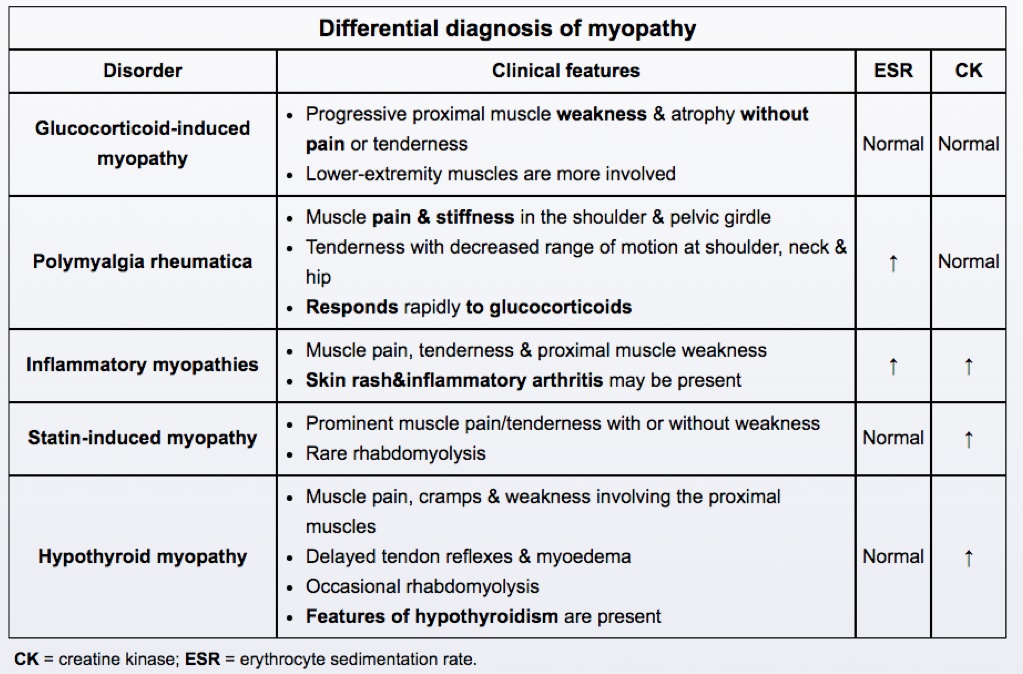
GIM is one the most common types of drug-induced myopathy and typically occurs weeks to months after starting glucocorticoid therapy. Acute myopathy following very high-dose pulse glucocorticoid therapy can occur in critically ill patients but is not as common as chronic myopathy complicating long-term glucocorticoid use. The mechanism is thought to be due to increased muscle catabolism and decreased anabolism as a direct effect of glucocorticoids.
This risk of GIM rises with higher doses of glucocorticoids (generally >40 mg hydrocortisone daily or its equivalent). Patients typically develop painless proximal muscle weakness (lower extremity before upper extremity) that manifests as difficulty in daily activities such as getting up from a chair, climbing stairs, or brushing hair. There is no muscle inflammation or tenderness, and creatine kinase and erythrocyte sedimentation rate (ESR) are normal. Muscle power improves after discontinuation of glucocorticoids, but recovery can take weeks to months.
Orbital cellulitis
Orbital cellulitis: is an infection of the fat and extraocular muscles of the eye. Patients usually have erythema, edema, and tenderness, often with impaired extraocular movement. These conditions generally do not cause paroxysms of severe retro-orbital pain or miosis.

Fibular Compression
This patient with intermittent foot drop likely has common fibular neuropathy.
The common fibular nerve, also called the common peroneal nerve, travels near the fibular head and is susceptible to compressive injuries from leg immobilization (eg, cast, bedrest), prolonged leg crossing, or protracted squatting. Manifestations are typically transient and reflect impaired functioning of the fibular nerve as follows:
Unilateral foot drop
Numbness/tingling over the dorsal foot and lateral shin
Impaired ankle dorsiflexion (walking on heels) and great toe extension
Preserved plantar flexion (walking on toes) and reflexes
Diagnosis is typically made with electromyography and nerve conduction studies. Treatment has limited effect but includes reducing pressure on the nerve (eg, avoiding crossing the legs), an ankle-foot orthosis splint, and physical therapy.
Glaucoma
demographics: is more common in women (especially age >40), Asian and Inuit populations, and individuals with farsightedness. Dim light, antimuscarinic can trigger.
symptoms: Patients typically develop rapid onset of severe eye pain and may see halos around lights. The affected eye will appear injected and the pupil will be dilated and poorly responsive to light. Patients can also develop tearing and headache with subsequent nausea and vomiting as the intraocular pressure increases.
complication: Untreated acute ACG can lead to severe and permanent vision loss within 2-5 hours of symptom onset.
Corneal Abrasion
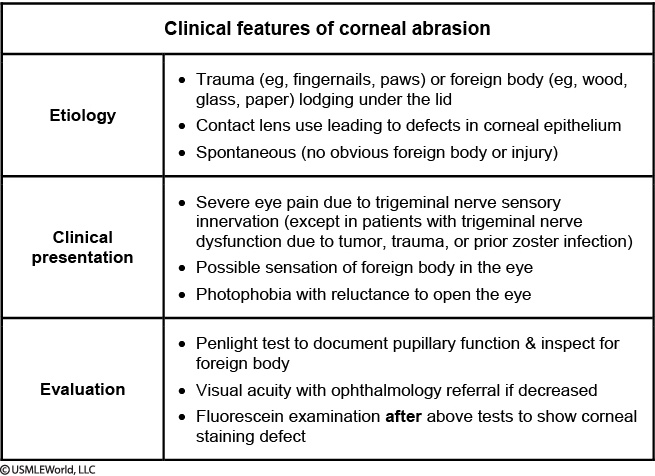
This patient's presentation suggests a corneal abrasion. Common causes of corneal abrasion include trauma (eg, fingernail, paws), foreign body (eg, paper, wood, glass) lodging under the lid, and contact lens use leading to a corneal epithelial defect. Abrasions can also occur without obvious corneal trauma. Patients typically develop severe eye pain and can further damage the surface by rubbing or washing the eye repeatedly. They ultimately can have photophobia with reluctance to open the eye and a foreign body sensation. Visual acuity may be normal or reduced. Fluorescein examination is notable for a corneal staining defect. Indications for ophthalmology referral include ulceration, pus, drop in visual acuity (the potential cause of blurry vision in this patient), or lack of healing within 3–4 days.
Although the patient has a corneal abrasion, he does not complain of eye pain. This indicates a likely cranial nerve (CN) V lesion. CN V (trigeminal nerve) contains sensory fibers in its 3 branches; the V3 (mandibular) branch also contains motor fibers. The V1 (ophthalmic) branch carries sensory fibers to the scalp, forehead, upper eyelid, conjunctiva, cornea, nose, and frontal sinuses. Damage to the V1 branch (specifically to the nasociliary nerve mediating the afferent limb of the corneal reflex) causes corneal anesthesia. Common causes of trigeminal nerve dysfunction include tumor, trauma, or prior herpes zoster infection.
Spinal Epidural Infection
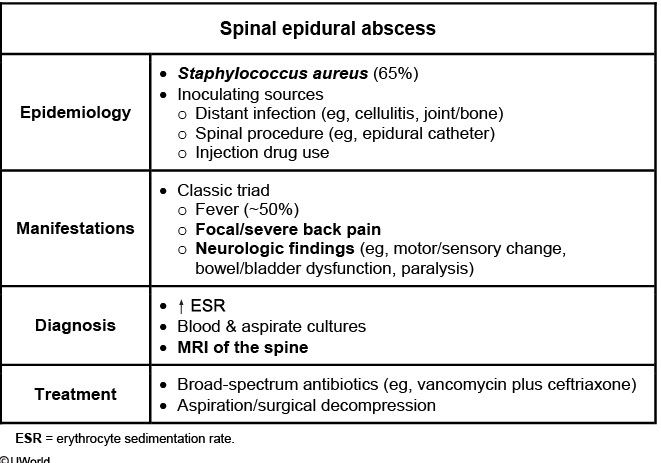
Spinal epidural abscess (SEA) is a rare infection of the epidural space that may threaten the spinal cord and result in paralysis. Most cases are due to hematologic spread from a distant infection (eg, cellulitis, bone/joint), intravenous drug use, or direct inoculation during a spinal procedure. Staphylococcus aureus is the most common (65%) causative organism.
SEA classically results in the triad of fever, back pain, and neurologic deficits; however, all 3 symptoms are present in a minority of cases. Most patients initially develop severe, focal back pain that progresses over days to nerve root pain ("shooting/electric") and more severe neurologic manifestations (motor weakness, sensory changes, bowel/bladder dysfunction, paralysis). The diagnostic test of choice is MRI of the spine due to high sensitivity early in the course of illness and excellent localization of infection extent. Treatment with broad- spectrum antibiotics and aspiration/surgical decompression is usually required.
case: A 68-year-old hospitalized man is evaluated for new-onset leg weakness. Six days ago, he was admitted to the hospital due to fever, right leg pain, and swelling. Physical examination showed right lower extremity edema, erythema, warmth, and tenderness from the foot to the midcalf. Leukocyte count was 16,000/mm3, and venous Doppler ultrasonography revealed patent leg veins without thrombosis. Blood cultures grew Staphylococcus aureus. The patient was treated with intravenous antibiotics, and his leg symptoms improved. However, this morning he had trouble getting out of bed due to significant leg weakness. The patient has a history of hypertension, type 2 diabetes mellitus, coronary artery disease, and systolic heart failure. He also has chronic low back pain from a work-related injury. The patient has had worsening mid-back pain over the last 2 days. Temperature is 38 C (100.4 F), blood pressure is 130/80 mm Hg, and pulse is 88/min. Physical examination shows normal mental status and cranial nerves. Abdominal examination reveals a suprapubic mass. There is midline tenderness over the lower thoracic vertebral area. Upper extremity strength is normal, but he is not able to lift either lower extremity against gravity. Which of the following is the best next step in management of this patient?

Hearing Loss
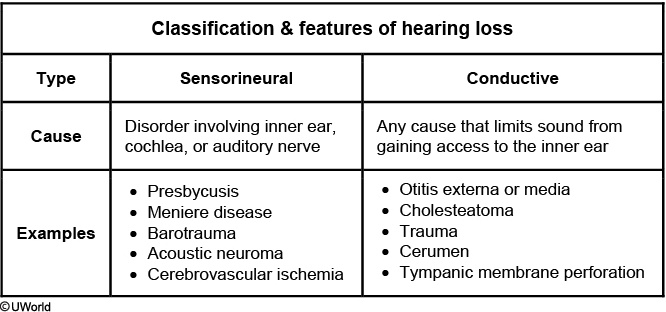
Meniere: vertigo, tinnitus. Unilateral.
neuroma: vertigo, nausea, mass effect. Bilateral
cholesteatoma: abnormal PE. White plaque on TM
otosclerosis: normal PE. Sclerosis in middle ear
Presbycusis (age-related hearing loss) is characterized by progressive bilaterally symmetric and predominantly high-frequency sensorineural hearing loss that occurs over many years. The condition affects more than half of all adults by age 75 and is due to degenerative changes of the inner ear or cochlear portion of the eighth cranial nerve. Patients with presbycusis will often hear well in one-on-one conversations in a quiet room; however, this ability will decline even if a small amount of competing noise is present. Subjective bilateral tinnitus can develop as the hearing loss progresses and is typically described as a steady or continuous ringing or rushing sound.
The presence of unilateral tinnitus, pulsatile tinnitus (eg, due to vascular malformations or pseudotumor cerebri), or tinnitus associated with other unilateral otologic symptoms should generally prompt the clinician to evaluate for other etiologies.
Botulism
Patients with suspected foodborne botulism should be checked for toxin in the blood. In addition to supportive care, treatment for adults and children age >1 involves passive immunity through administration of horse-derived (equine) antitoxin.
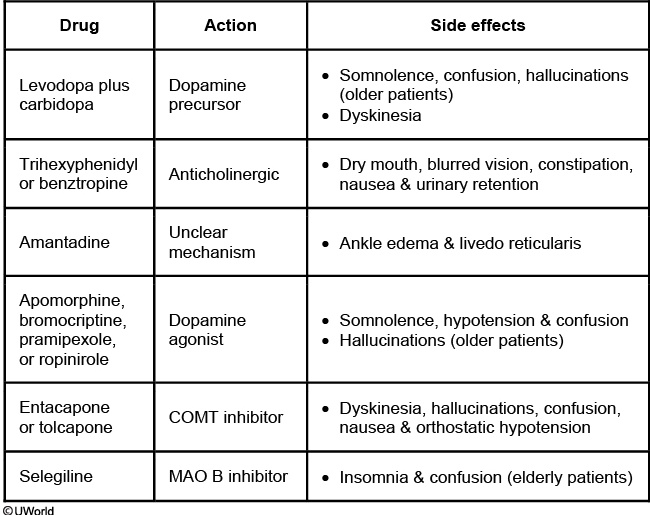
Parkinson drug SE
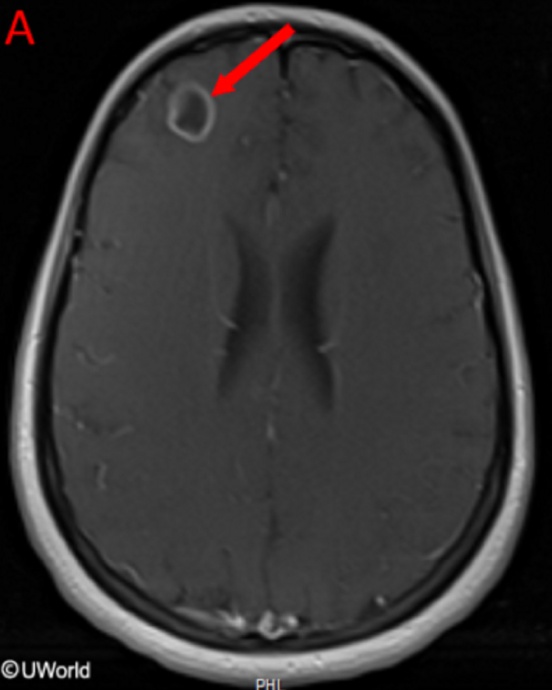
CNS Lymphoma
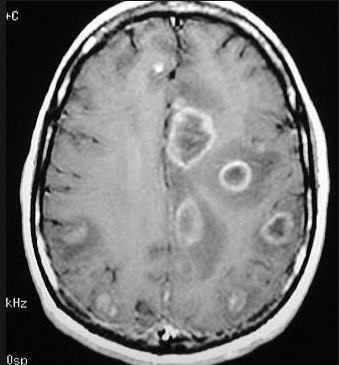
This patient has a primary CNS lymphoma. The presence of EBV DNA in the CSF is specific for this condition. MRI reveals a weakly ring-enhancing mass that is usually solitary and periventricular.
Toxoplasmosis is a good differential diagnosis; however, it is unlikely in this patient since he is receiving trimethoprim-sulfamethoxazole. MRI reveals multiple, ring-enhancing, spherical lesions in the basal ganglia. A positive Toxoplasma serology is quite common in normal subjects in the United States, and is therefore not specific for toxoplasmosis.
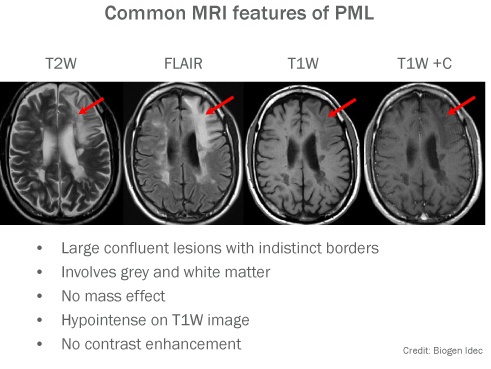
Progressive multifocal leukoencephalopathy lesions are non-enhancing, and do not produce mass effects.
In patients with AIDS dementia complex imaging studies reveal cortical and subcortical atrophy and secondary ventricular enlargement.
MG
.,
thymoma
Head Trauma
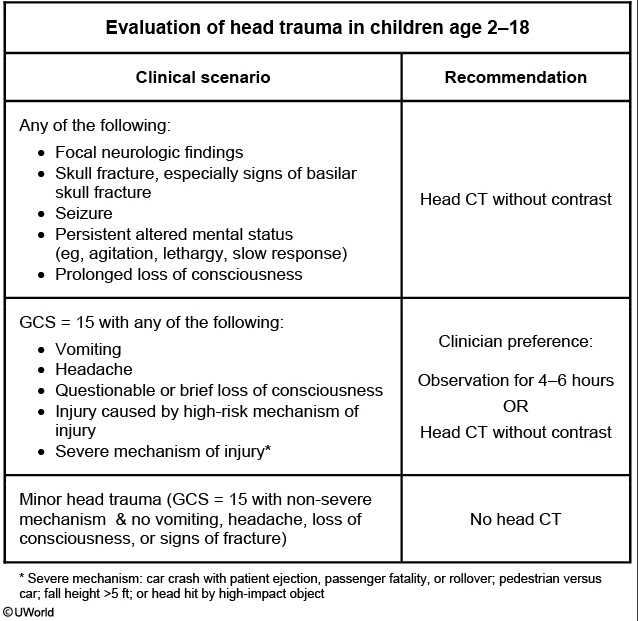
Head trauma can be categorized as minor, mild traumatic brain injury (TBI), or serious TBI. Mild traumatic brain injury (TBI) is defined as a head injury that is associated with a Glasgow coma scale (GCS) score of 13-15, loss of consciousness for <5 minutes, headache, loss of memory (amnesia) before/after injury for <24 hours, alteration in mental status at time of injury, and/or vomiting. This patient's brief loss of consciousness, headache, and vomiting is consistent with a mild TBI (eg, concussion).
Head CT without contrast is the first-line imaging modality in the emergency department. Neuroimaging results are often normal in mild TBI but should be considered due to overlapping clinical features with serious TBI (eg, headache, vomiting, loss of consciousness). Observation for 4-6 hours in the emergency department is an alternative option for patients with mild TBI, and head CT can be performed if symptoms worsen. The patient can be discharged home with a reliable caretaker if the CT scan is normal or if there is improvement during observation. Clear written instructions with return precautions should also be provided.
CNS Malignancy Treatment
Chemotherapy may be coupled with surgical resection and radiation in patients with highly malignant primary brain tumors (eg, glioblastoma multiforme, medulloblastoma). It can also be considered in patients with highly chemosensitive metastatic brain disease (eg, due to testicular germ cell tumor).
Whole brain radiation is not indicated for the treatment of meningioma; rather, it is usually considered for the treatment of diffuse metastatic brain disease. Focused tumor radiation (stereotactic radiosurgery) may be considered for partially resected or unresectable meningiomas.
Phenytoin
The fetal hydantoin syndrome is characterized by midfacial hypoplasia, microcephaly, cleft lip and palate, digital hypoplasia, hirsutism and developmental delay.
Absence Seizure

Absence seizures are brief (<20 seconds), generalized seizures characterized by asudden impairment of consciousness in children age 4-10. Events can occur infrequently or up to 100 times a day without warning. Absence seizures may be accompanied by simple automatisms (eg, eyelid fluttering, lip smacking) but not more complex motor events. No aura. Patients generally are unaware that a seizure has occurred and do not remember what happened during it. The events are often first noticed by teachers and are frequently mistaken for attention deficit hyperactivity disorder (ADHD) or normal childhood staring spells.
Absence seizures can usually be provoked by hyperventilation and are diagnosed by electroencephalography, which classically reveals a 3-Hz spike-wave discharge pattern during episodes. The first-line treatment for absence seizures is ethosuximide.
Gentamicin Toxicity
Aminoglycosides can cause ototoxicity (hearing loss) by damaging the cochlear cells. In addition, some aminoglycosides (especially gentamicin) can also damage the motion-sensitive hair cells in the inner ear to cause selective vestibular injury (vestibulopathy) with or without significant ototoxicity.
Because both vestibular end organs are equally affected, patients usually do not experience significant vertigo as there is no left or right imbalance in vestibular input to the central nervous system. Patients can experience oscillopsia, a sensation of objects moving around in the visual field when looking in any direction. This deficient vestibulo-ocular reflex can lead to gait disturbances. An abnormal head thrust test can help detect vestibular dysfunction due to gentamicin. The patient is asked to look at a fixed target. Rapid head movement away from the target normally causes the eyes to remain fixed on the target. However, patients with vestibulopathy are unable to maintain their eyes on the target. The eyes move away and then return back to the target with a horizontal saccade. Patients with aminoglycoside toxicity occasionally have severe bilateral vestibulopathy, which can lead to chronic symptoms.
Warfarin Antidote
Initial therapy should include intravenous vitamin K, which has a sustained response but takes approximately 12-24 hours to be effective (promotes clotting factor synthesis in the liver). Prothrombin complex concentrate (PCC) should also be provided as it contains vitamin K-dependent clotting factors (eg, II, VII, IX, X) that offer rapid (minutes) and short-term (hours) reversal of warfarin. Fresh frozen plasma can be considered if PCC is not available; however, it takes longer to prepare/administer and requires more volume infusion compared to PCC.
Tranexamic acid is an antifibrinolytic agent that may be used to treat heavy menstrual bleeding and prevent excessive blood loss during certain types of surgery. However, it would not reverse this patient's elevated INR and does not have a role in the treatment of warfarin-associated hemorrhage.
Amaurosis Fugax
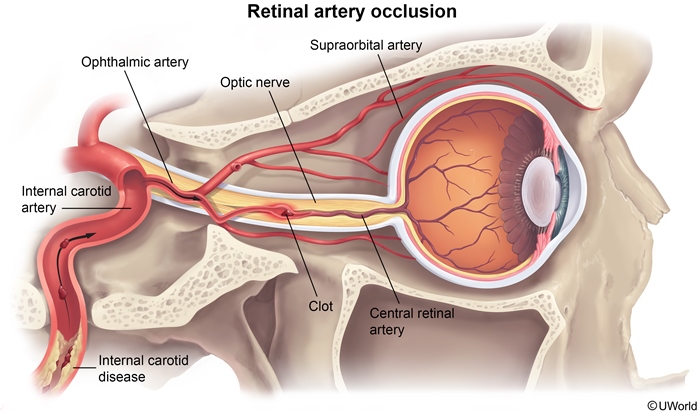
This patient has amaurosis fugax, which is characterized by painless, rapid, and transient (<10 minutes) monocular vision loss. The description of a curtain descending over the visual field is highly suggestive of this diagnosis. The most common etiology is retinal ischemia due to atherosclerotic emboli originating from the ipsilateral carotid artery; therefore, patients with vascular risk factors (eg, hypertension, hyperlipidemia, smoking) should be evaluated with a duplex ultrasound of the neck. Funduscopic examination is often normal but may show embolic plaques and retinal whitening (due to ischemia). Patients with amaurosis fugax and concomitant carotid artery disease have an increased risk of stroke.
Cardioembolic disease is a much less common cause of amaurosis fugax compared to carotid atherosclerosis. Do not use echocardiogram.
Other causes of transient monocular vision loss are uncommon and include cardioembolic disease, giant cell arteritis, retinal vein occlusion, retinal vasospasm, and papilledema.
Tonometry
Ocular tonometry is indicated for measuring intraocular pressure in patients with acute angle-closure glaucoma, which typically presents with painful monocular vision loss, headache, and nausea/vomiting.
Heat Stroke
Cancer Pain
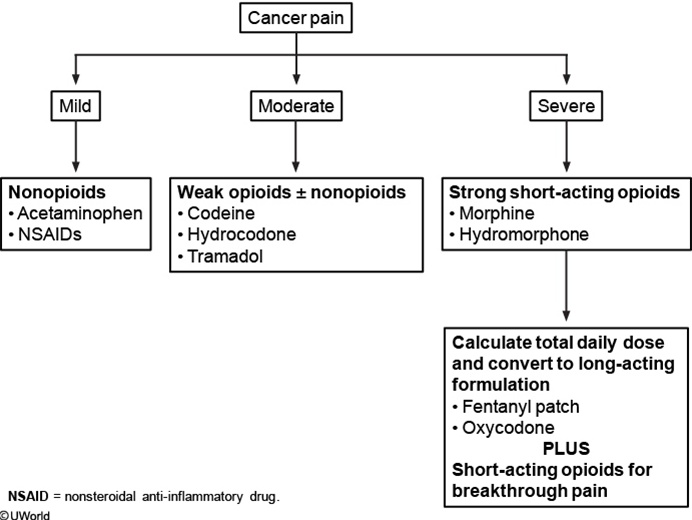
Mild to moderate cancer-related pain can usually be managed with nonopioid analgesics (eg, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]). However, for severe pain, or if initial interventions are not effective, short-acting opioids (eg, morphine, hydromorphone, oxycodone) should be offered. Short-acting opioids are safe and well-tolerated if taken as directed, and the dose and schedule can be varied depending on the patient's pain pattern. If the patient has pain requiring frequent dosing or if bedtime dosing does not provide adequate relief through the night, a long-acting opioid (eg, sustained-release morphine) may be added (Choice A).
Carotid Dissection
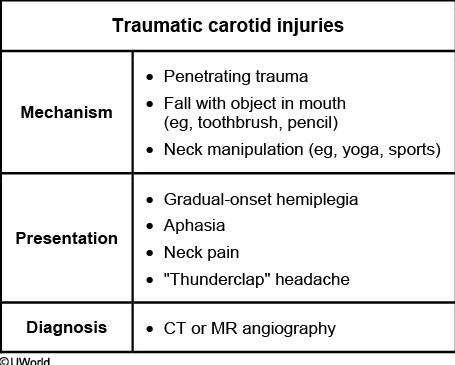
This patient's symptoms of hemiparesis and aphasia after injury to the posterior pharynx are suspicious for an injury to the cervical internal carotid artery, which is located directly lateral and posterior to the tonsillar pillars. Carotid artery dissection is a rare but potentially severe complication of penetrating trauma, seemingly minor oropharyngeal trauma (eg, a fall with object in mouth), or neck strain/manipulation (eg, yoga, sports).
Intimal injury to the internal carotid artery can result in dissection or thrombus formation, which occurs over hours to days and can extend into the middle and anterior cerebral arteries. Patients may develop neck pain, "thunderclap" headache, and symptoms of an ischemic stroke (eg, hemiparesis, facial droop, aphasia). The diagnosis of a carotid artery dissection is confirmed with CT or MR angiography.
Supraspinatous vs Axilliary
A complete supraspinatus tear causes weakness of abduction, which can be appreciated in the drop arm test.
Although the deltoid is responsible for shoulder abduction between 15-90 degrees, deltoid weakness is best appreciated at extreme extension rather than abduction.
HTN and Stroke
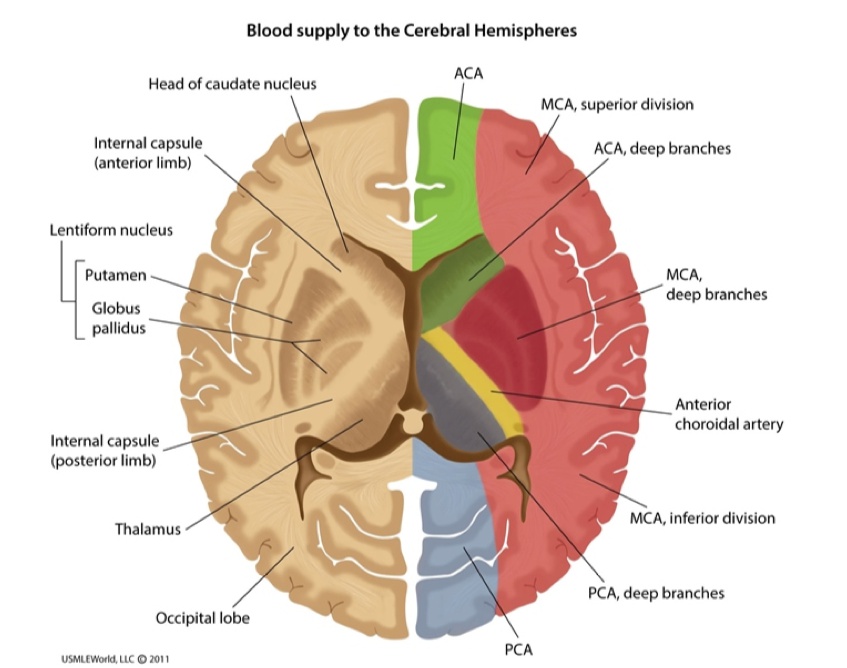
Although he has many risk factors for cerebrovascular accident (CVA), hypertension has the strongest association with both ischemic and hemorrhagic stroke due to elevated shearing force on the intracerebral vascular endothelium, which accelerates the atherosclerotic process and promotes thrombi formation.
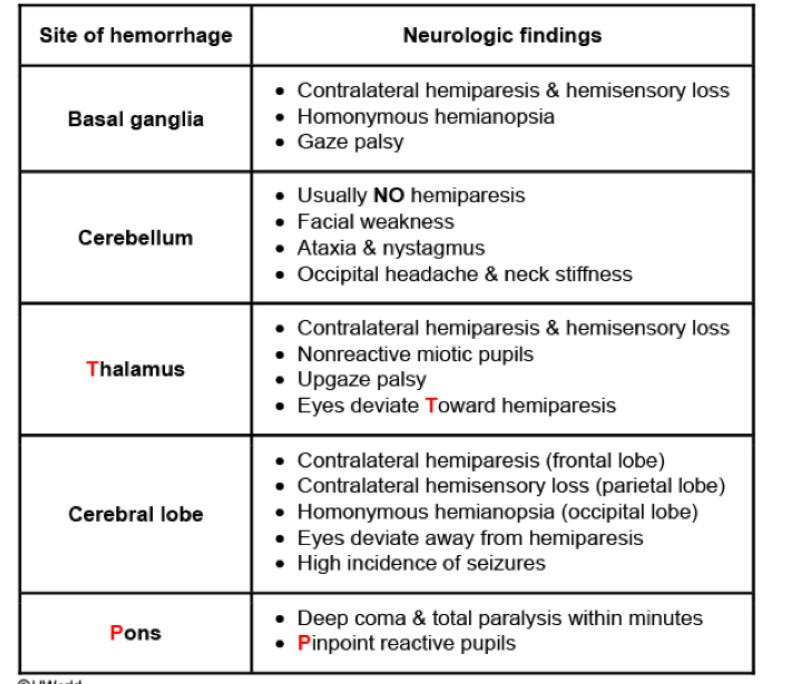
Hemorrhage
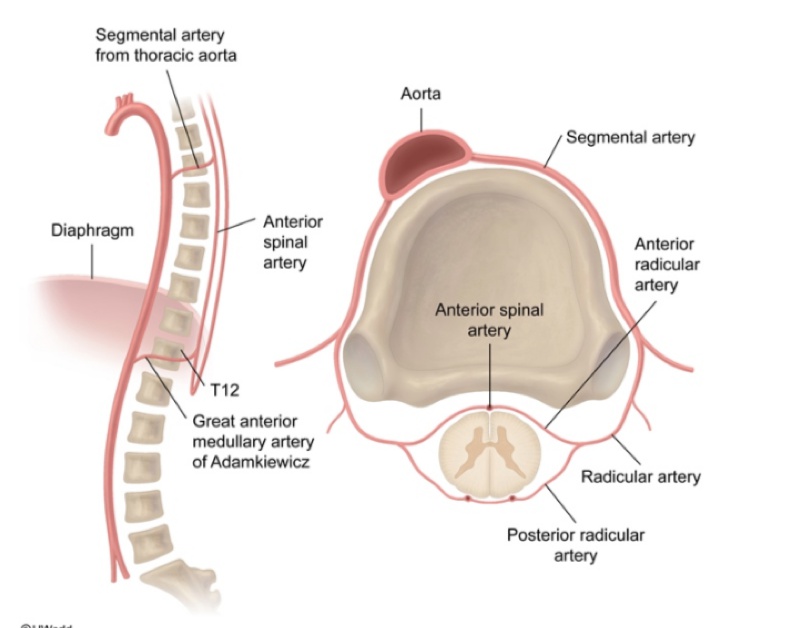
Spinal cord
Ophthalmic Veins
Ddx myopathy
Brain Blood Supply
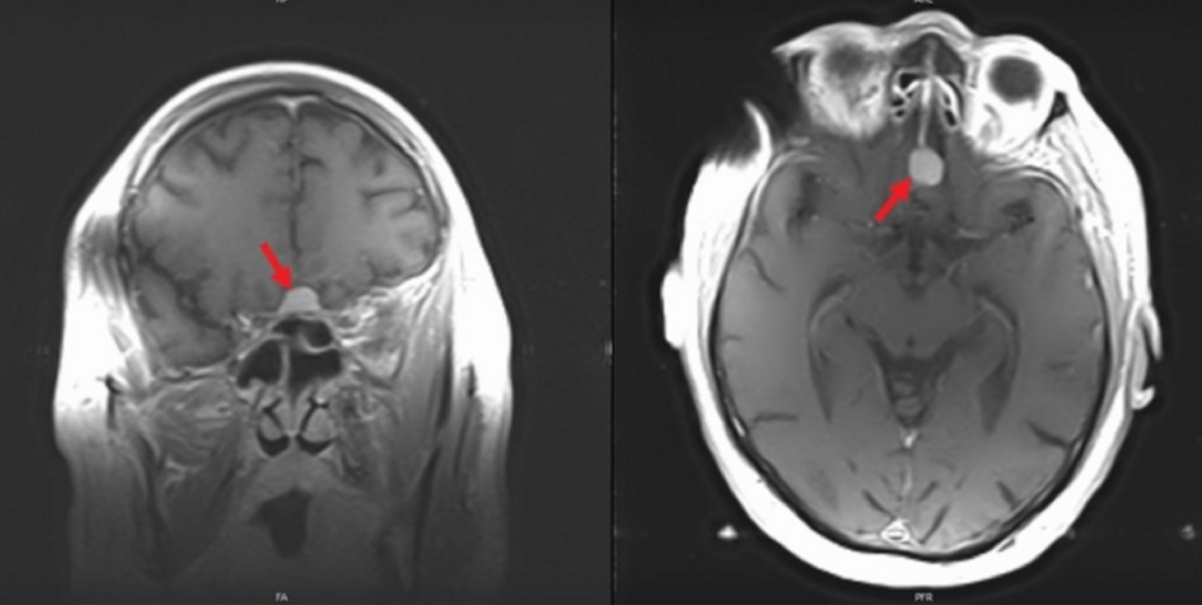
Meningioma
Cauda
Last updated