CNS Infections
Bacterial Meningitis
Bacterial meningitis is due to bacterial invasion of the meninges and CSF of the subarachnoid space that produces an inflammatory response, which can cause neurologic injury. This can be a medical emergency that must be treated quickly to avoid neurologic damage.
Causes
The most common causes of bacterial meningitis in neonates in descending order:
Group BStrep
E. coli
Listeria monocytogenes
The most common causes of bacterial meningitis in children (1 months – 2 years) in descending order:
Strep pneumoniae
Neisseria meningitidis
Haemophilus influenzae type B
The most common causes of bacterial meningitis amongst people 2-18 years of age in descending order:
N. meningitidis
Strep pneumoniae
Haemophilus influenzae
The most common causes of bacterial meningitis in adults (up to 60 years) in descending order:
Strep pneumoniae
Neisseria meningitidis
H. influenzae
The most common causes of bacterial meningitis in the elderly in descending order:
Strep pneumoniae
Neisseria meningitidis
Haemophilus influenzae
Listeria monocytogenes
The most common causes of bacterial meningitis in the immunocompromised in descending order:
Listeria monocytogenes
Gram negative bacilli
Strep pneumoniae
Symptoms
The classic clinical presentation of bacterial meningitis includes the triad of fever, nuchal rigidity, and change in mental status.
Bacterial meningitis can be further complicated by the following symptoms:
Headache (exacerbated by lying down), papilledema, and seizures
Photophobia
Maculopapular rash with petechiae in cases of N. Meningitidis
Physical exam findings associated with bacterial meningitis include:
Kernig’s sign, which is an inability to extend knees fully while patient is supine with hips flexed because the stretching of the meninges causes too much irritation and pain
Brudzinski’s sign, which is where passive flexion of neck leads to hip and knee flexion
Diagnosis
The diagnosis of bacterial meningitis is made with a lumbar puncture.
Note: do NOT perform an LP if you suspect a space occupying lesion, elevated intracranial pressure or any focal neurologic deficits because it can lead to herniation. In these cases, obtain a CT first.
The CSF Profile of bacterial meningitis consists of
Increased WBC count (1000-5000; neutrophils > 80%)
Increased protein (100-500 mg/dl)
Decreased glucose (<40)
Treatment
Treatment of bacterial meningitis consists of empiric antibiotic therapy with vancomycin and cephalosporins (3rd or 4th generation for CSF penetration) until the infectious agent is identified. If the patient is an infant, >50 yrs old or immunocompromised, then ampicillin is also added to the empiric therapy.
Fungal meningitis should be treated with amphotericin B and tuberculosis meningitis should be treated with rifampin, isoniazid, pyrazinamide, and ethambutol, which can be remembered using the mnemonic RIPE.
Prophylaxis for close contacts of patients with Neisseria meningitidis consists of either ciprofloxacin or rifampin.
Immunocompromised hosts for whom vaccination is recommended include:
Over 65 yrs against S. pneumoniae
Immunocompromised patients against N Meningitidis
Asplenic patients against N. meningitidis, S. pneumoniae,and H. influenzae
Complications
Complications of bacterial meningitis include:
Subdural effusion
Empyema
Brain abscess
Hearing loss
Mental impairment
Viral Meningitis
Causes
Viral meningitis, or aseptic meningitis, is meningitis caused by viral infection by:
Enterovirus, such as echovirus
Herpes simplex virus and varicella-zoster virus
Lymphocytic choriomeningitis virus
HIV
Mumps virus
Symptoms
The clinical presentation of viral meningitis is similar to bacterial meningitis, consisting of the classic triad of:
Neck stiffness
Headache
Fever
It is important to note that symptoms of viral meningitis are generally more mild and have a slower onset (days instead of hours) than those of bacterial meningitis.
In addition to the classic triad, other symptoms associated with viral meningitis include:
Nausea and vomiting
Photophobia
Malaise
Rash
Diagnosis
The diagnosis of viral meningitis is made based on the CSF profile, which will show:
Increased WBC count (lymphocyte predominant)
Slight increase in protein, but < 150 mg/dl (nl = 100)
Normal glucose (note bacterial meningitis has decreased glucose)
Treatment
Viral meningitis is generally self-limiting, but empiric antibiotic treatment is usually started until a viral cause is confirmed. An exception to this would be meningitis found to be caused by HSV. This circumstance would be treated with acyclovir.
Encephalitis
Encephalitis is inflammation of the brain parenchyma most commonly caused by viral infections.
Causes
Viral etiologies of encephalitis include:
Herpes viruses: HSV-1, VZV, EBV
Arboviruses: eastern equine, West Nile, Zika
Enterovirus: polio
Nonviral etiologies of encephalitis include:
Toxoplasmosis
Cerebral aspergillosis
T-cell lymphoma
Symptoms
The presence of abnormal brain function is the differentiating feature between encephalitis and aseptic meningitis. Patients with aseptic meningitis, while uncomfortable and lethargic, will have normal cerebral function. In patients with encephalitis, altered mental status and brain abnormalities (such as motor or sensory deficits, altered behavior and personality changes) are expected.
Thorough history is important to narrow the differentials of potential viruses causing the encephalitis. For example, arbovirus is more likely to be possible during seasons or activities with increased mosquito exposure while herpes simplex virus can be transmitted any time of the year.
Patients with encephalitis will present with an altered mental status ranging from subtle deficits to complete unresponsiveness.
Other symptoms include:
Malaise
Headache
Vomiting
Neck pain
Focal neurologic deficits
Fever
Parotitis in association with the other symptoms of encephalitis indicates infection with mumps virus.
Flaccid paralysis with maculopapular rash that evolves into an encephalitis strongly suggests the possibility of West Nile virus infection.
Findings of dermatomal vesicular lesions in association with symptoms of encephalitis is indicative of varicella-zoster virus.
Diagnosis
Diagnosis of a patient with encephalitis relies upon history, physical exam, lumbar puncture and imaging.
Lumbar puncture in patients with viral encephalitis shows:
Increased WBCs with lymphocytic predominance
Increased protein (but <150mg/dL)
Normal glucose
PCR of CSF is used to confirm the diagnosis of viral encephalitis and identify the pathogen.
Results of imaging in patients with encephalitis may or may not demonstrate abnormal radiographic findings on CT or MRI modalities. Temporal lobe involvement is a strong indication for encephalitis caused by HSV-1.
The most important viral pathogen to rule out in a patient with suspected encephalitis is HSV-1, since it is nearly universally fatal if left untreated.
Treatment
Treatment of encephalitis patients entails supportive therapy.
Patients with encephalitis without a known etiology should receive empiric therapy with acyclovir for HSV-1 infection due to the morbidity and mortality associated with delayed treatment for HSV-1 encephalitis. Empiric therapy should be initiated while the CSF PCR results are pending.
CMV encephalitis can be treated with ganciclovir or foscarnet.
GBS
Guillain-Barré syndrome is an inflammatory demyelinating polyneuropathy that affects motor neurons.
Guillain-Barré syndrome is typically preceded by a bacterial or viral infection of upper respiratory or gastrointestinal tract. This infection evokes an immune response, which in turn cross-reacts with peripheral nerve components. This is referred to as "molecular mimicry".
Common infections that cause Guillain-Barré syndrome include:
Campylobacter jejuni (most common)
CMV
Hepatitis
HIV
Mycoplasma pneumoniae
Symptoms
Guillain-Barré syndrome presents with abrupt onset of rapidly ascending weakness and paralysis in all four extremities with decreased or absent deep tendon reflexes (spinal cord compression has weakness and increased reflex. GBS also does not have sensory symptoms that cord compression has).
Generally, symptoms of Guillain-Barré syndrome are symmetric and progress from distal to central muscles.
If Guillain-Barré syndrome progresses to generalized paralysis, it can lead to respiratory arrest.
While sensation loss is not common in Guillain-Barré syndrome, patients may present with:
Paresthesias in the hands and feet
Pain involving the back and extremities
Dysautonomia can occur and manifests as symptoms that include:
Tachycardia (most common)
Urinary retention
Hypertension alternating with hypotension
Bradycardia
Arrythmias
Loss of sweating
These are dangerous complications often associated with sudden death.
Diagnosis
Diagnosis of Guillain-Barré syndrome is typically made through history and physical along with electrodiagnostic studies and CSF analysis.
CSF analysis in Guillain-Barré syndrome reveals increased CSF protein with a normal CSF white blood cell count. This is known as albuminocytologic dissociation.
Electrodiagnostic studies in Guillain-Barré syndrome reveal decreased motor nerve conduction velocity.
Treatment
The major disease-modifying treatments for Guillain-Barré syndrome are plasma exchange (aka plasmapheresis) and intravenous immune globulin (IVIG).
Treatment of Guillain-Barré syndrome includes supportive care with monitoring of pulmonary function as mechanical ventilation may be necessary.
After the diagnosis of GBS is suspected, the most important next step in management is assessing the patient's pulmonary function by serial spirometry. Measurement of forced vital capacity (FVC) is the gold standard for assessing ventilation; a decline in FVC (especially ≤20 mL/kg) indicates impending respiratory arrest requiring endotracheal intubation.
Steroids should not be given in patients with Guillain-Barré syndrome. They have been shown to not be helpful in the treatment of the disease and in some studies have hindered the improvement of the patient.
Guillain-Barré syndrome usually progresses over a period of about two weeks and by four weeks after the initial symptoms, 90 percent of patients have recovered from the disease.
Tick Born Paralysis
cause: The etiology of the paralysis is neurotoxin release; the tick needs to feed for 4-7 days for the release of neurotoxin.
symptoms: Patients usually present with progressive ascending paralysis over hours to days. Paralysis may be localized or more pronounced in 1 leg or arm, as in this patient. Fever is typically not present. Sensation is usually normal. There is no autonomic dysfunction noted in these patients, unlike that seen in the majority of patients with Guillain Barré syndrome (GBS).
diagnosis: The CSF examination is typically normal.
treatment: Meticulous search for ticks in these patients usually reveals a tick, and removal usually results in improvement within an hour and complete recovery after several days.
Intracranial Abscess
Causes
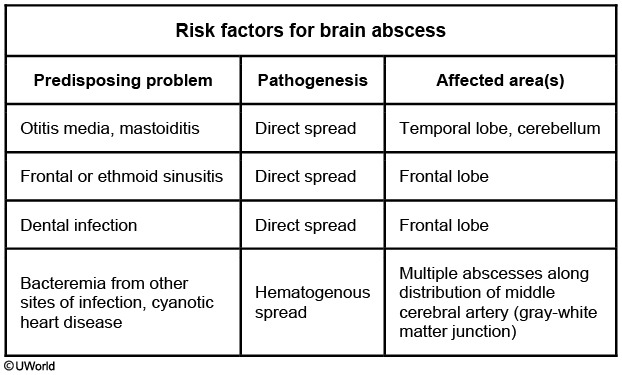
An intracranial abscess is usually the result of infection elsewhere in the body.
Contiguous spread may occur in sinusitis, otitis media, mastoiditis, or dental infections.
Hematogenous spread may occur in endocarditis, intrapulmonary right-to-left shunting (Tetralogy of fallot), chronic pulmonary infections or pneumonia. The right-to-left shunt of venous blood in the heart (eg, through a ventricular septal defect) bypasses the pulmonary circulation, where bacteria in the bloodstream are typically filtered and removed by phagocytosis. These patients have poor perfusion to the brain due to chronic hypoxemia, metabolic acidosis, and increased blood viscosity from secondary polycythemia. This results in a tendency for bacterial seeding at the gray-white matter junction.
The most common organisms are Streptococcus and Staphylococcus spp, most notably viridans streptococi and S. aureus, respectively, and most abscesses are polymicrobial.
Immunocompromised patients (particularly with in HIV+ with CD 4 counts < 50 – 100 /μl) may have toxoplasmosis.
Symptoms
Patients often present with some combination of headache, fever, and focal neurological deficits. Seizures are also commonly seen in patients with an intracranial abscess. (e.g. Tetralogy kid with seizure)
Diagnosis
Diagnosis of intracranial abscess is based on CT with contrast showing a ring-enhancing lesion.
Gram stain and culture after stereotactic drainage should follow imaging of the intracranial abscess.
Treatment
Treatment involves incision and drainage with sterotactic guidance, and antibiotic therapy.
Empiric, broad coverage antibiotics should be the initial therapy, and narrowed upon culture and sensitivity analysis. Commonly used empiric coverage includes metronidazole (for patients with a brain abscess arising from an oral, otogenic, or sinus source) and vancomycin (for patients with a brain abscess from hematogenous spread).
Rabies
Rabies is a lethal CNS infection caused by rabies virus, which is transmitted to humans by the bite of an infected animal.
The rabies virus is a rhabdovirus, a bullet-shaped virion that contains a single-stranded RNA virus.
Symptoms
The virus causes a severe encephalitis resulting in neuronal degeneration and inflammation.
What makes the rabies virus particularly lethal is its ability to evade the immune system by sequestering itself in the nervous system. The incubation period ranges from 3-8 weeks and is determined by the distance of the bite from the central nervous system (a bite to the foot will result in a longer incubation period than a bite to the neck).
The acute neurological form of the disease begins within 2-7 days of onset of symptoms and coma may result within 10 days of the onset of symptoms.
The early presentation of a rabies infection includes malaise, headache, restlessness, and fear of water ingestion, which is secondary to laryngeal spasm.
Progressive cases of rabies have a more severe presentation, which includes:
Severe CNS excitability
Foaming at the mouth
Extremely painful laryngeal spasms
Alternating mania and stupor
Diagnosis
Laboratory testing is recommended with both the offending (biting) animal and the patient who was bitten. Viral testing (CSF, skin, and serum) in humans with symptoms is confirmatory of the disease.
The offending animal should be caught and tested or observed for signs of rabies.
If infected, the animal needs to be killed so the brain can be tested for the presence of the virus and Negri bodies, which are round eosinophilic inclusions in neurons that are characteristic of a rabies infection.
Patients with rabies exposure are managed with thorough wound cleansing plus postexposure prophylaxis. In previously unimmunized individuals, postexposure prophylaxis includes both passive and active immunization:
Rabies immune globulin (passive immunization)
Rabies vaccine (active immunization)
Note that the vaccine alone (i.e. no rabies immune globulin) is indicated for postexposure prophylaxis of individuals who have been previously vaccinated for rabies.
If the virus has replicated to the point where motor and sensory axons have been invaded and the patient has become symptomatic, treatment attempts are futile.
Rabies carries a 100% mortality rate without treatment, or if the virus has invaded motor and sensory axons.
Last updated