15 ENT
Ear
OTM
path:
URI bugs, strep, moraxella, H. flu
middle ear (tympanic membrane affected)
symptoms: unilateral painful ear relieved by pulling of pinna (tug ear)
diagnosis
otoscope: loss of light reflex, bulging erythematous tm, fluid behind ear
pneumatic insulflation: rigid tm
treatment:
1st line: amoxicillin
recurrence: add clavulanic acid
recur and recur: ear tubes, tympanoplasty. 3 occurences in 6 months. 4 occurences in 1 year
penicillin allergy: cephalosporin if no anaphylaxis, cefdinir. Azithromycin if anaphylaxis
OTE
path
infection of outer ear, pinna and canal
swimmer's ear: shower, swimming. Pseudomonas
digintal trauma: picking at ear canal with Qtip. Staph
symptoms: unilateral, worse with pulling of pinna
diagnosis
otoscope: outer canal erythematous, no bulging tm
clinical diagnosis
treatment
spontaneous resolve for mild cases
if malignant and bad: ear drops. Cipro for antibiotic. Steroid to feel better
rule out mastoiditis
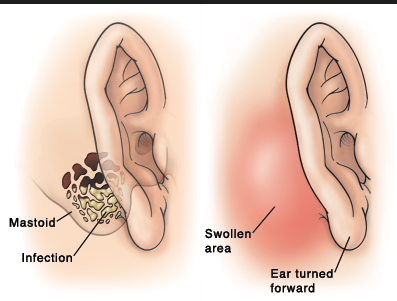
Mastoiditis
path: infection of mastoid bones caused by pseudomonas
pt: risk if has ear tubes
symptoms
looks like OTM
mastoid swelling (behind ear)
Anteriorly rotated ear
diagnosis: clinical and CT showing swelling of mastoid
treatment: surgical decompression
Sinus
Bacterial
path: URI bugs, strep usually. If recurrent, foreign body
symptoms
congestion
bilateral purulent discharge, thick white smelly from both nose
pain on facial tap
diagnosis
do not order xray/CT. Air fluid levels on xray and opacification on CT
Clinical
treatment
supportive
if temp > 38 or > 10 days, or symptoms worsens: penicillin (amoxicillin, clavulanic).,
Viral - "cold"
path: rhinovirus
symptoms
congestion
bilateral clear rhinorrhea, copious
diagnosis: no xray/CT, PCR, IF. No culture to see if bacterial
treatment
Supportive.,
CT if recurrent viral or bacterial sinusitis to find anatomic defect.
Pharyngitis
path: viral (most likely) or GAS
symptoms
sore throat
odynophasia: pain with swallowing
diagnosis: Centor criteria
treatment
Centor < or 1: nothing
2 - 3: rapid strep, f/u with culture if negative and really suspicious
greater or equal to 4: treat with antibiotics (amox, clavulanic)
r/out EBV: sorethroat, big spleen
C: no cough
E: exudates
N: nodes, LAD
T: temp > 38
OR: age
if < 14: +1
if > 44: -1
Foreign body
path
kids stick things in places
causes bacterial infection (ear, nose)
symptoms: unilateral bacterial infection
diagnosis: clinical suspicion
treatment: remove obj with forceps, endoscopy, bronchoscopy
Homeless population
path: homeless put coins in ears to prevent insects
symptoms: scratching, buzzing
treatment
do not shing light
use lidocaine to paralyze insect first
Epistaxis
path: digital trauma (nose picking) or injury
symptoms: unilateral and < 30 min
diagnosis: clinical
treatment
lean forward, allow blood drip, apply pressure or ice
anterior recurrent: cauterize with nitric stick
posterior recurrent: packing
Choanal Atresia
path: path from nose to throat blocked due to atresia or stenosis. Can't breath through nose
symptoms
baby turn blue with feeds and pink with crying
Child that snores
diagnosis: fail to pass catheter. Fiber optic wire for stenosis
treatment: surgery
Last updated