02 Pediatric
Hip
Developmental Dysplasia of the Hip
Pathogenesis
Result of abnormal development of the acetabulum, which leads to displacement of the femoral head.
Displacement of the femoral head in developmental dysplasia of the hip interferes with normal development of the hip joint.,
Developmental dysplasia of the hip is the most common orthopedic disorder in newborns.
Risks
Risk factors include:
Female gender (6:1 over males)
Firstborn children
Oligohydramnios
Delivery in breech
Family history.,
Diagnosis
Positive physical exam findings within the first 3 months of age include:
Barlow sign, which dislocates an unstable hip
Ortolani sign, which reduces a dislocated hip
Galeazzi sign, which indicate limb length discrepancies due to a dislocated hip.,
With the hip reduced, the Barlow test is performed by flexing the hips and knees then adducting the hips and applying a posterior force to the head of the femur. The test is positive if the hip dislocates posteriorly.
With the hip dislocated, the Ortolani test performed by flexing the hips and knees then abducting the hips and applying an anterior force to the head of the femur. The test is positive if the hips are reducible.
Positive physical exam findings after one year of age (i.e, a walking child) include:
Trendelenburg gait
Increased lumbar lordosis
Toe walking (compensating for limb length discrepancy)
Pelvic obliquity
Ultrasound is the preferred method of hip imaging in developmental dysplasia of the hip prior to femoral head ossification at 4-6 months of age.
X-ray imaging is the preferred method of viewing developmental dysplasia of the hip after the femoral head begins ossifiying at 4-6 months of age.
Treatment
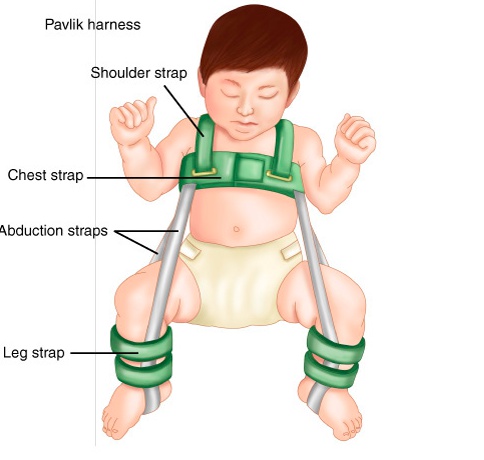
Treatment of developmental dysplasia involves a pavlik harness in children less than 6 months of age.
Pvlik harness:
Treatment of developmental dysplasia of the hip in children 6 months old to 2 years of age involves either closed or open reduction followed by Spica casting.

Treatment of developmental dysplasia of the hip in children ages 2-8 years can be treated with open reduction.
Developmental dysplasia of the hip is not corrected in children older than age 8 due to minimal benefit.
Permanent hip dysplasia is a complication that arises from inadequately treated cases of development dysplasia of the hip.
Legg-Calve-Perthes
Pathogenesis
An idiopathic avascular necrosis of the proximal femoral epiphysis
The disease is thought to be the result of disruptions in the vascular supply with subsequent revascularization. Damage results from epiphyseal resorption, collapse, and the effect of the repair process.
The disease is most commonly seen in children between 4-8 years of age and it affects males 5 times as often as females.,
Risks
Risk factors associated include:
Positive family history
Low birth weight
Exposure to second-hand smoke
Asian, Inuit, and Central European descent
Interestingly, the disease has been associated with ADHD in 33% of cases.,
Symptoms
The disease has an insidious onset, and may first present with a gradual painless limp followed by intermittent knee, hip, groin, or thigh pain.
Physical exam findings include:
Hip stiffness with loss of internal rotation and abduction
Gait disturbance
Limb length discrepancy (late disease finding)
Diagnosis
Radiographic findings include asymmetric hips visible on X-ray. Early findings include:
Medial joint space widening (earliest finding)
Small femoral head due to irregularity of the femoral head ossification center
Subchondral fracture.,

Treatment
The treatment strategy is containment of the hip within the acetabulum by either bracing or surgical means.
Nonoperative treatment is satisfactory in 60% of cases and includes:
Observation alone
Restricted activity
Physical therapy
Operative treatment is indicated in children over age 8 or in cases of permanent hip dysplasia, and involves acetabular reconstruction.,
Complications associated are related to increased risk of hip complications in adulthood, which include:
Osteoarthritis
Progressive avascular necrosis
Early arthroplasty in cases of permanent dysplasia.,
SCFE
Pathogenesis
A slippage of the epiphysis relative to the metaphysis at the level of the growth plate. It is one of the most important pediatric and adolescent hip disorders.
Cartilage in the hypertrophic zone acts as the weak point where the slippage occurs.
Demographics
More common in:
Adolescent males
African Americans
Obese children
Hypothyroidism
Down syndrome.,
Obesity is the single greatest risk factor for the development of slipped capital femoral epiphysis.
Symptoms
Thigh and groin pain is the most common presenting symptoms.
Can sometimes present as knee pain in a significant number of patients.
Physical exam findings in patients include:
Trendelenburg gait
External rotation during passive hip flexion (limited hip flexion)
Limited hip internal rotation and abduction.,
Bilateral involvement is seen in approximately 20% of patients at the time of presentation.
Diagnosis
X-ray imaging including AP and frog leg lateral of both hips shows the epiphysis remaining within the acetabulum while the neck displaces anteriorly and externally rotates leaving the head posterior to the neck. An early radiographic finding is epiphysiolysis where the growth plate is widened or shows increased lucency.,

Treatment
Treatment options are primarily surgical with percutaneous pinning of the slipped side. Treatment of this condition is emergent.,
Prophylactic pinning of the non-slipped side should be considered in cases of slipped capital femoral epiphysis related to hypothyroidism.

Complications of slipped capital femoral epiphysis include avascular necrosis, chondrolysis, and premature osteoarthritis.
Fractures
Torus
A Torus fracture, also known as a buckle fracture, is a common injury seen in children. It is a compression failure of bone.
Because the bones of children may be softer on one side, one side may buckle when stressed without affecting the other side.
Torus fractures usually occur at the junction of the metaphysis and diaphysis, especially in the distal radius.
Torus fractures are diagnosed with x-ray imaging. This injury is referred to as a torus fracture because of its similarity to the raised band around the base of a classic Greek column when viewed on x-ray.

Torus fractures are inherently stable and heal in 2-3 weeks with simple immobilization, such as casting.
Greenstick
A Greenstick fracture is an incomplete fracture of long bones that is commonly seen in children. The bone bends and cracks but does not break into pieces, largely due to the softness and flexibility of bones in children.
These fractures occur when the bone is bent and there is failure on the tensile (convex) side of the bone. This is different than in torus fractures where the concave side buckles.
The fracture line does not propagate to the concave side of the bone, but the concave side shows evidence of microscopic failure with plastic deformation.
X-ray imaging will show a mid-diaphyseal break, usually with angulation and disruption of the cortical bone on the side of the fracture.

It may be necessary to break the bone on the concave side in order to achieve reduction of the fracture because the plastic deformation recoils it back to the deformed position. Immobilization with casting for 2-3 weeks allows this fracture to heal.
Toddler
A toddler’s fracture is a nondisplaced spiral fracture of the distal tibial metaphysis.
The injury often occurs after a seemingly harmless twist or fall and is often unwitnessed. These fractures will often be presented in a question in regards to worrying about child abuse.
These fractures are most commonly seen in children 1-4 years of age.
The classic symptom of a toddler’s fracture is refusal to bear weight, which can manifest as pulling up the affected extremity or florid display of protest.
The AP and lateral x-ray views of the tibia-fibula may show a nondisplaced spiral fracture of the distal tibial metaphysis. An oblique view is often helpful because the fracture line may be visible in only 1 of the 3 views.
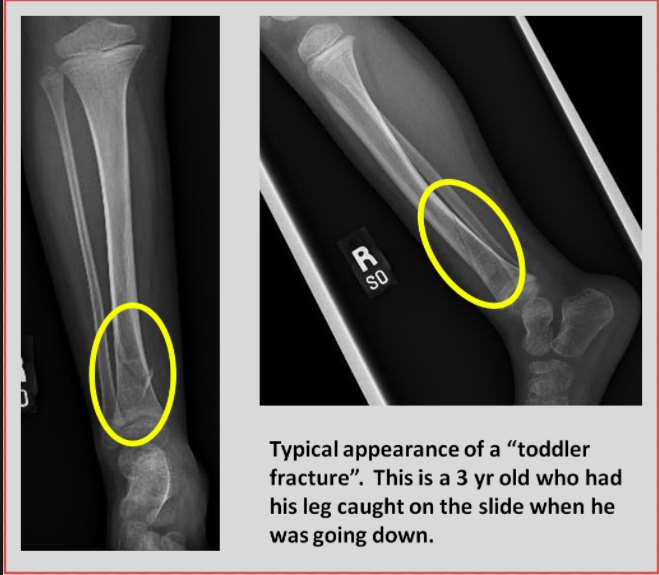
The treatment of a toddler's fracture involves the use of an above-knee cast for approximately 3 weeks.
GI
Neonatal Bilious
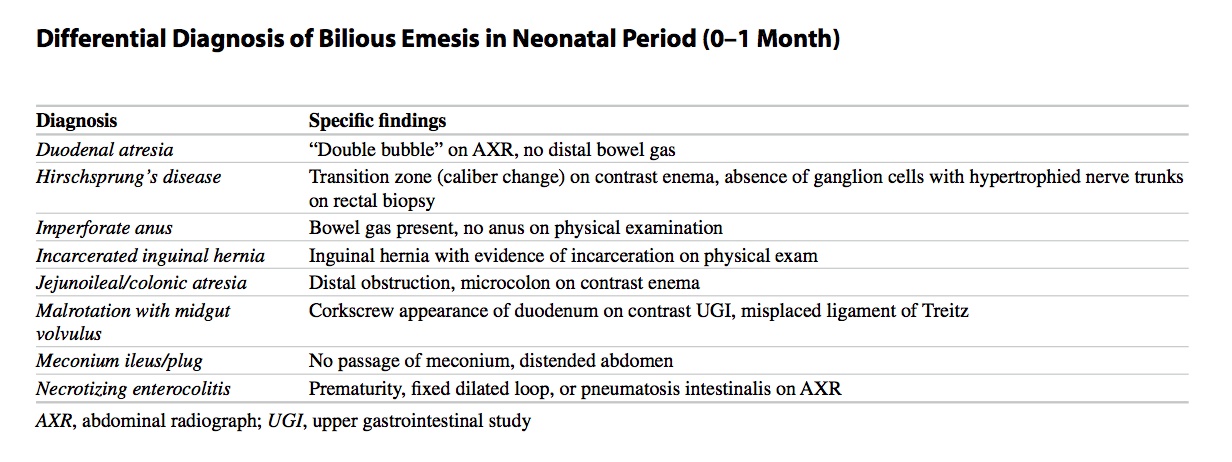
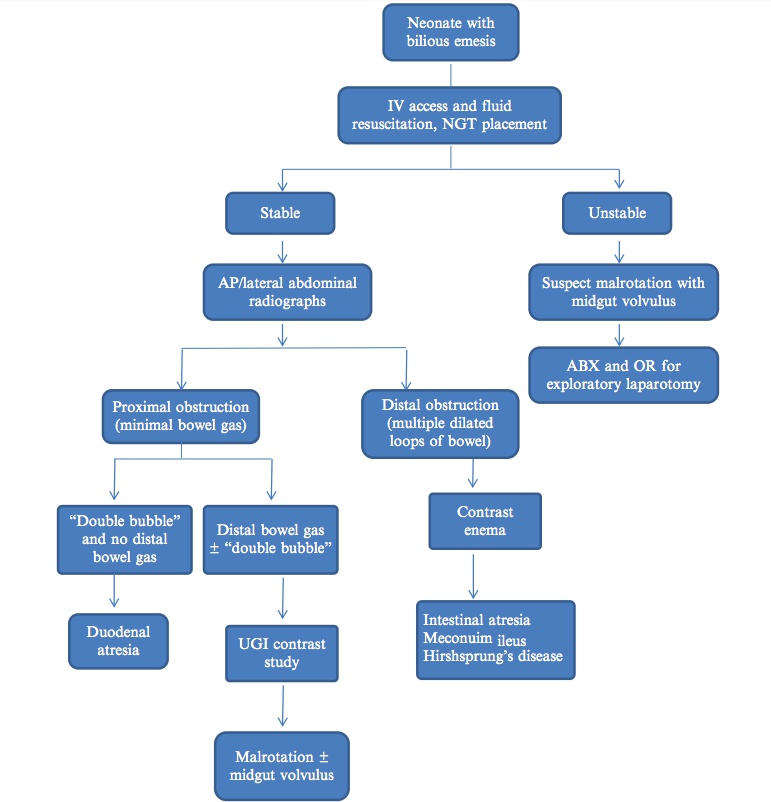
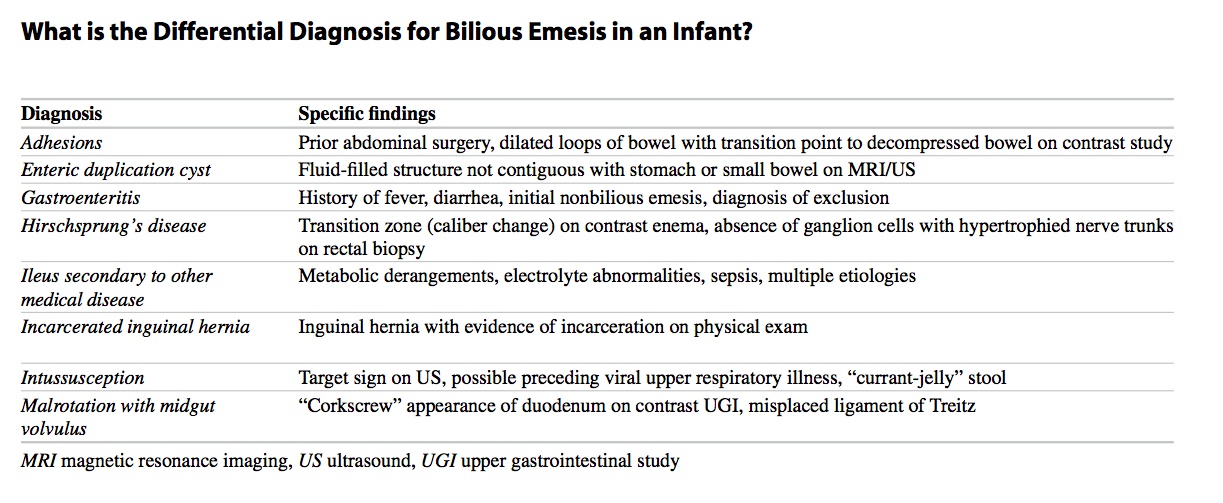
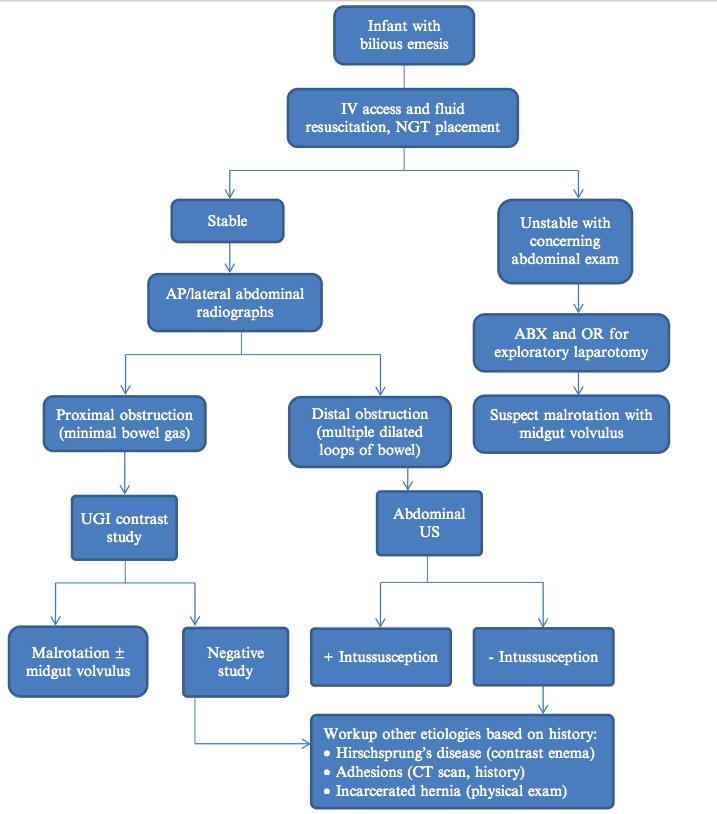
The absence of distal bowel gas in the above radiograph secures the diagnosis of a complete duodenal obstruction, and no further testing is indicated. If any distal gas is seen, an upper gastrointestinal (UGI) contrast study is necessary to rule out malrotation with midgut volvulus, the most life- threatening condition. The UGI contrast study may also be helpful in diagnosing other etiologies of partial duodenal obstruction.
Infant Bilious
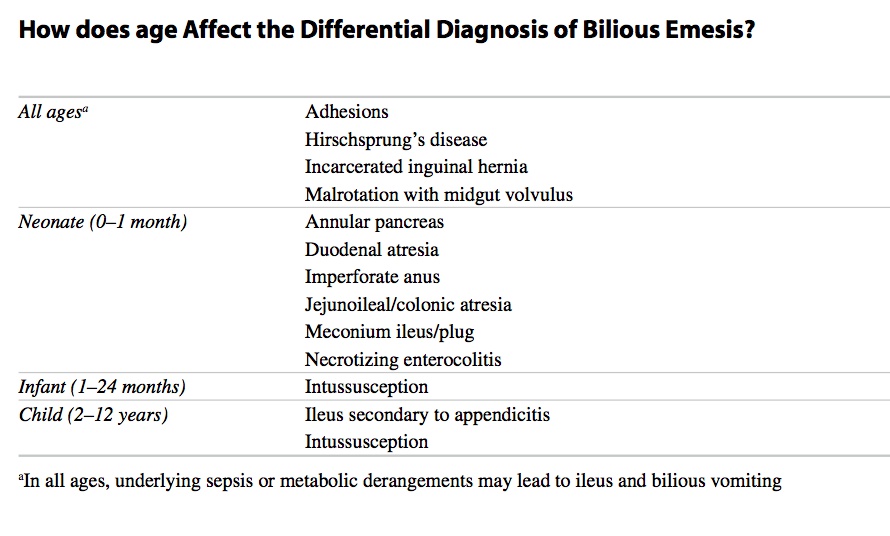
Duodenal Atresia
Demographics
Congenital duodenal obstruction most commonly results from duodenal atresia.
One-third of affected infants have trisomy 21.
Duodenal atresia has been described in association with congenital rubella and Prader-Willi syndromes.
Symptoms
Presentation of duodenal atresia is within the first few days of life and usually follows the first feed.
The major symptom is vomiting, most commonly bile stained as most atresias occur distal to the ampulla of Vater.
Gastric distention with visible peristalsis may be present but is easily decompressed by nasogastric aspiration.
Diagnosis
The classic radiographic sign associated with duodenal atresia is the “double bubble” sign on abdominal radiography.
The double bubble is denoted the higher, larger, left-sided stomach bubble together with the lower, smaller, right-sided bubble of the dilated proximal duodenum.
Treatment
Treatment for duodenal atresia is surgical correction, which is performed at open laparotomy or laparoscopically. The entire duodenum is visualized by mobilizing the right colon, allowing identification of the obstruction and exclusion of associated malrotation.
Malrotation
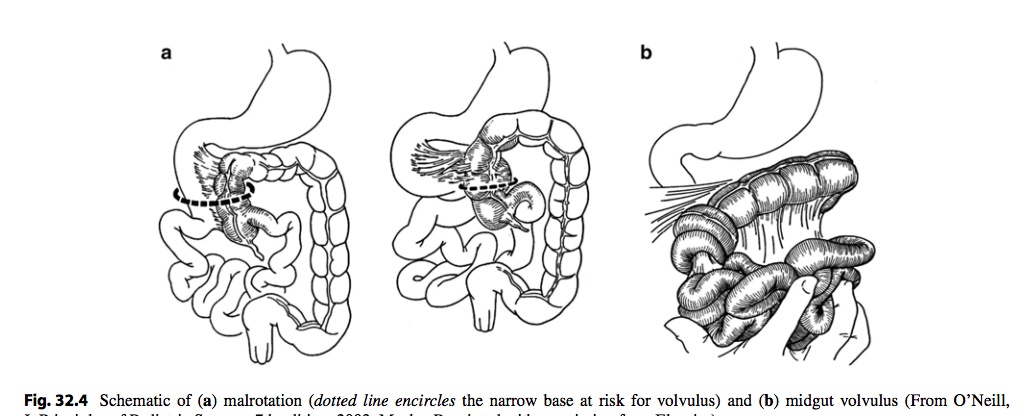
During embryologic development of the midgut, the bowel lengthens, herniates into a U-shaped (around 33 days) loop into the base of the umbilical cord and rotates around the SMA axis 270° counterclockwise (after 44 days). It then reenters the abdomen and undergoes fixation.
Malrotation is defined as a failure of normal rotation of any portion of the gastrointestinal tract. It also implies abnormal fixation, which is the predisposing factor for the development of a volvulus.
Demographics
Intestinal malrotation is associated with the following conditions:
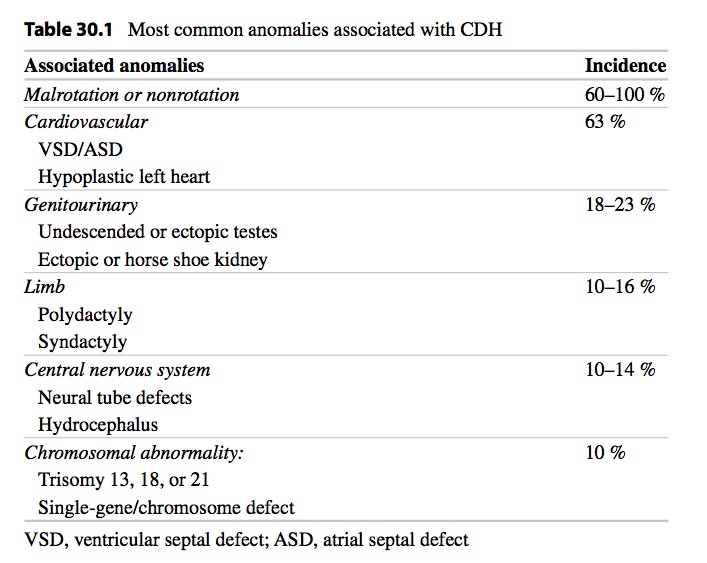
Diaphragmatic hernia
Duodenal atresia
Jejunoileal atresia
Intestinal malrotation is twice as common in males as in females.
Omphalocele, gastroschisis
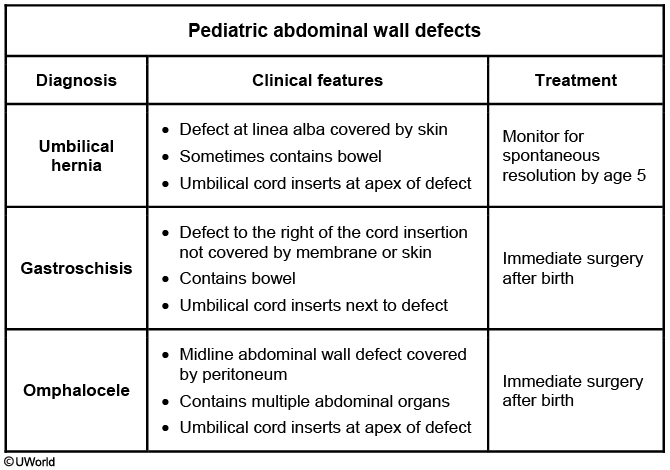
Omphalocele occurs when the midgut loop fails to return to the abdomen, which presents with an intact shiny mesenteric covering.
Gastroschisis is a defect in the ventral abdominal wall due to failure of closure of the lateral folds. The viscera extrude from the peritoneal covering without the shiny mesenteric covering seen in omphalocele. The umbilical cord is also to the left of the defect as opposed to omphalocele where it goes through the defect
Umbilical Hernia
An umbilical hernia is due to an incomplete closure of the abdominal muscles around the umbilical ring at birth. It is most commonly associated with African-American race, premature birth, Ehlers-Danlos syndrome, Beckwith-Wiedemann syndrome, and hypothyroidism. Physical examination shows a soft, non-tender bulge covered by skin that protrudes during crying, coughing, or straining. The hernia may contain omentum or portions of the small intestine. Most umbilical hernias are reduced easily through the umbilical ring with very low risk of incarceration and strangulation.
Small umbilical hernias typically close spontaneously by concentric fibrosis and scar tissue formation. Spontaneous closure is less likely with large (>1.5 cm diameter) hernias or in patients with underlying medical problems. Surgery is recommended around age 5 for persistent hernias, or sooner if it is bothersome or causing complications.
Volvulus
The clinical presentation of acute midgut volvulus includes:
Occurrence in the first decade of life
Sudden onset bilious vomiting
Diffuse abdominal pain out of proportion to physical exam
Chronic midgut volvulus typically presents with recurrent abdominal pain and intestinal malabsorption.
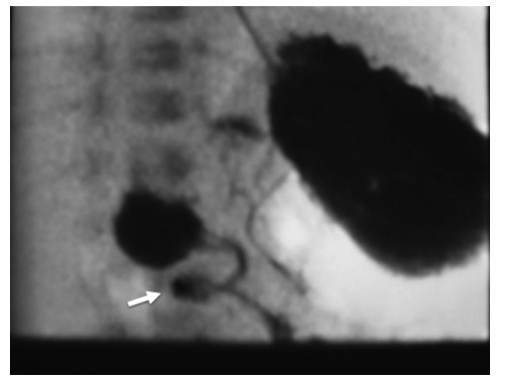

corkscrew appearance (white arrow)
PE, Diagnosis, Treatment
Some degree of abdominal distention should be seen on physical examination.
The gold standard for diagnosing intestinal malrotation is an upper gastrointestinal series. Ultrasound imaging is also associated with a 0% false positive rate in the hands of an experienced user.
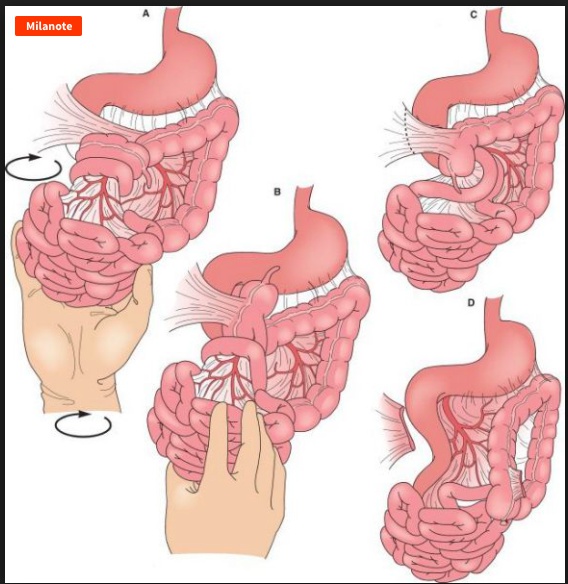
Intestinal congenital defects, such as malrotation, require surgical correction. The most effective procedure done for malrotation is the Ladd procedure which involves a reduction of the volvulus (if present), division of the mesenteric bands, placing the small bowel on the right, the large bowel on the left of the abdomen, and an appendectomy.
Meckel's
Meckel’s diverticulum is an anomalous remnant of the vitelline duct present in the terminal ileum that results from incomplete obliteration of the omphalomesenteric duct. It is a true diverticulum.
It is the most common congenital abnormality of the gastrointestinal tract, with an incidence ranging from 1 to 4% and a male-to-female ratio of 2:1.
50% of the diverticula contain heterotopic tissue, with gastric mucosa being by far the most common type. A few diverticula contain pancreatic tissue.
For exam purposes, it is good to know the five rules of 2s:
2 types of ectopic tissue
Within 2 years of life
2% of population
2 feet from ileocecal valve
2 inches long
Symptoms
Meckel’s diverticulum causes lower GI bleeding resulting from the ulceration of adjacent ileal mucosa by acid-secreting heterotopic gastric mucosa contained in the diverticulum. Bleeding is often brisk and painless.
Meckel’s diverticulum most common cause of significant lower GI bleeding in infants and young children.
Abdominal findings on physical examination are usually benign.
Provided that gastric mucosa is present, the diagnosis of Meckel’s diverticulum can be made with an 85 to 90% sensitivity by a radionuclide 99mTc pertechnetate scan (also called a Meckel’s scan).
Radionuclide scan findings associated with Meckel’s diverticulum show the presence of heterotopic gastric mucosa in the right lower quadrant of the abdomen.
If radionuclide scan results are equivocal, arteriography may be used which will show an anomalous branch of the superior mesenteric artery feeding the diverticulum.
Treatment
The treatment of choice for Meckel’s diverticulum is surgical excision.
Meckel’s diverticulum can cause intestinal obstruction and has been associated with the following complications:
Intussusception
Volvulus
Abdominal wall hernia
Meckel’s diverticulitis
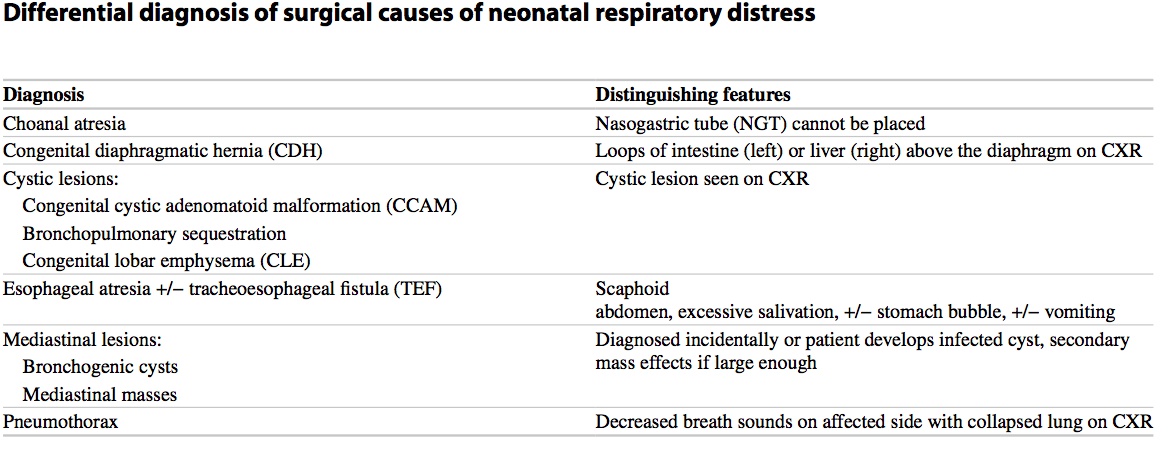
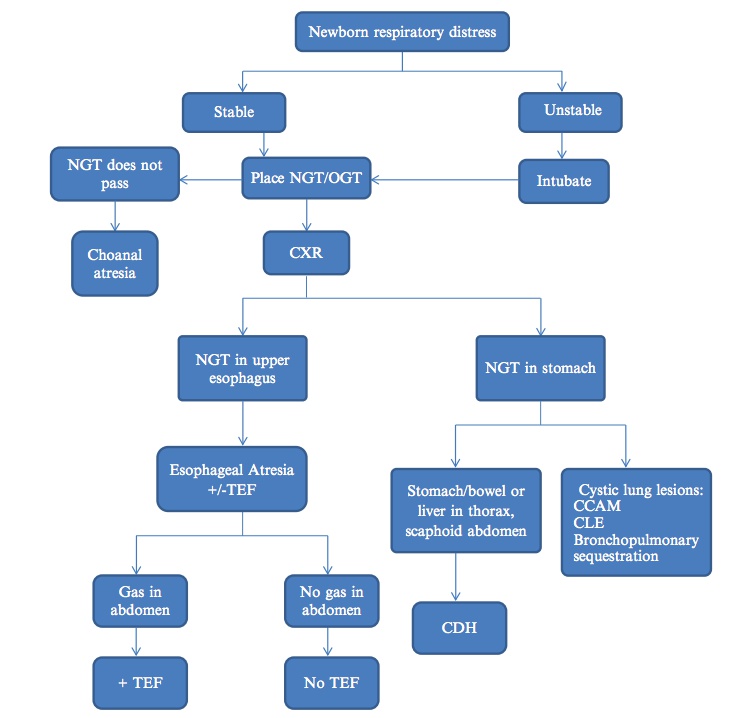
Diaphragmatic Hernia
path: failure of septum transversum to completely divide the pleural and coelomic cavities during fetal development. Herniation of intra-abdominal contents occurs during a critical period of lung development when the
pulmonary arteries and bronchi are branching. Pulmonary hypoplasia results from decreased pulmonary mass and bronchiolar branching as well as dysfunctional surfactant production.
PE: scaphoid abdomen
Diagnosis:
prenatal US
xray:

Associations
Respiratory
Last updated