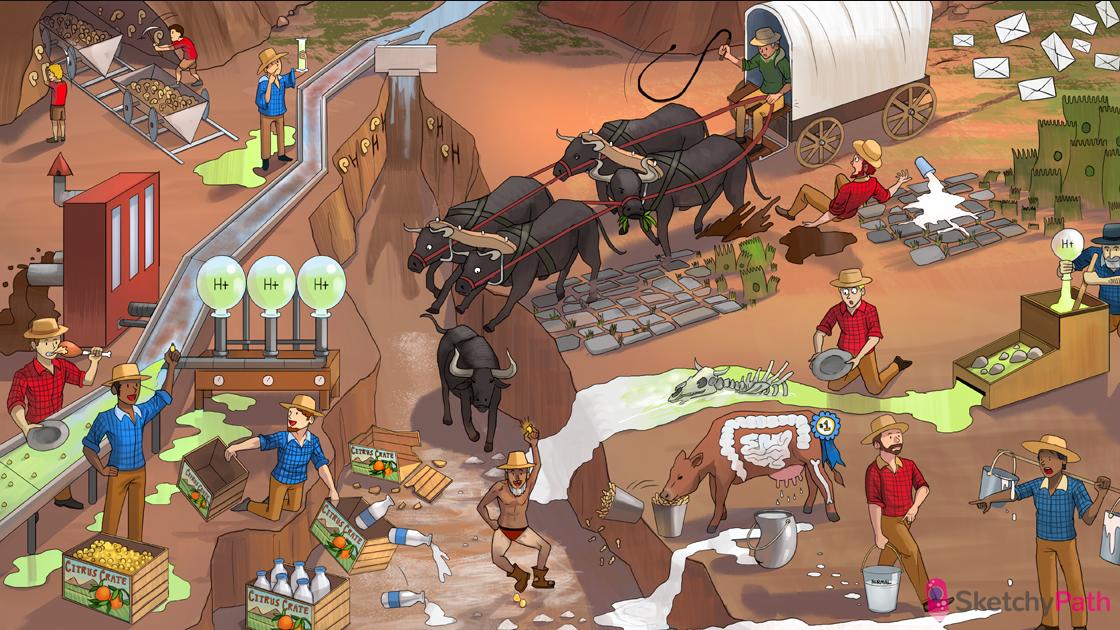
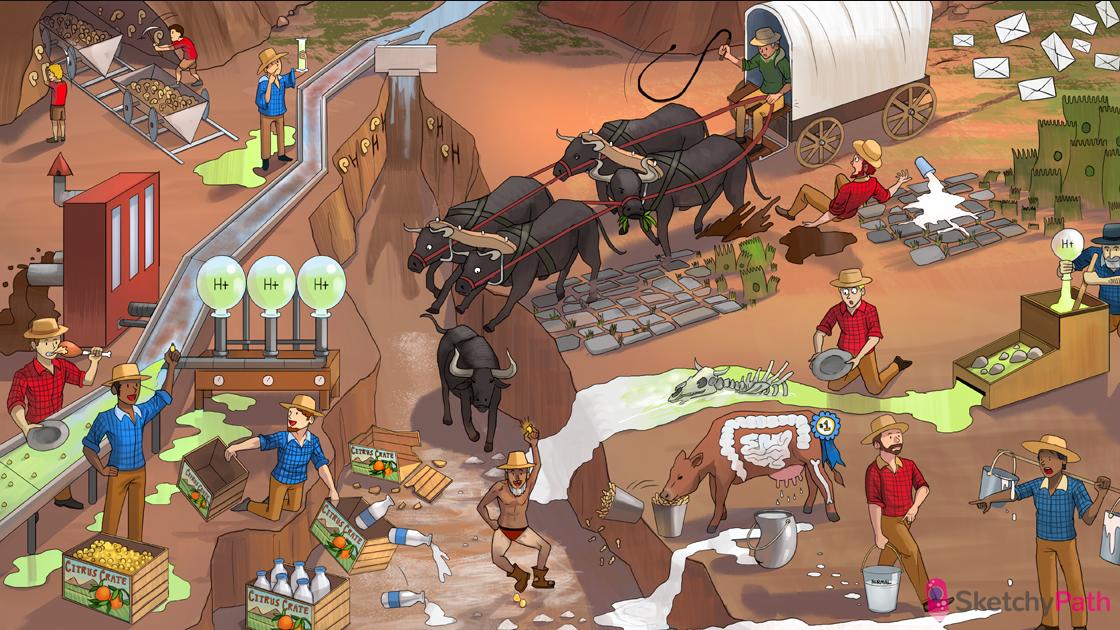
28 Pathogenesis
_..

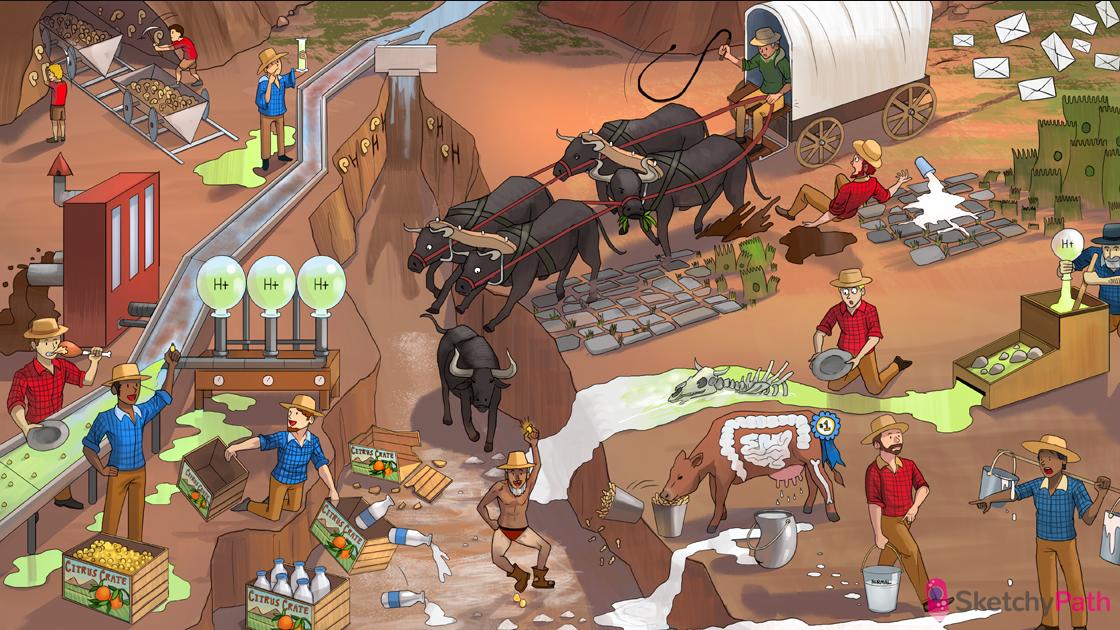
CREATE your own MEAT combo: creatinine is the breakdown product of CREATINE (found in muscle cells)
Credit card: creatinine (used to measure kidney function)
“$1 MENU”: creatinine has a normal serum concentration of 1.0 mg/dL (ranging from 0.6 to 1.2)
“Free filtered”: creatinine is freely filtered at the glomerulus
“NEVER REABSORBED!”: once in the nephron, creatinine is NOT resorbed and only minorly secreted (Cr filtered load ≈ Cr urinary excretion)
“*May contain minor secretions”: creatinine is secreted in small amounts into the nephron → urine conc. is slightly higher than serum conc. (slightly overestimate GFR)
“Grounds Filter Rate”: glomerular filtration rate (GFR) is the amount of fluid that filters across the glomerulus into Bowman’s space (125ml/min)
Credit card cleared: creatinine clearance can be used to approximate GFR (slight overestimation) because Cr is freely filtered at the glomerulus and is neither secreted (almost!) nor reabsorbed
“CUP → ”: C=UV/P (creatinine clearance equation used to estimate GFR)
“100% real”: creatinine clearance (estimation of GFR) is normally >100 ml/min mg/dL (<100 ml/min is abnormal, <10 indicates renal failure)
Elderly man knocking over filtered coffee: GFR decreases with age (renal dosing of drugs)
BUN bag: Blood Urea Nitrogen (BUN) is cleared by the kidney (final breakdown product of nitrogen containing compounds)
“N” order cycle: BUN comes from the urea cycle in the liver (amino acid metabolism)
Pyrimidine hexagon titles: BUN also comes pyrimidine metabolism (nitrogenous bases)
“Order 10": BUN has a normal serum concentration of 10 mg/dL (ranging from 7-20)
Spilled filtered coffee: a decrease in GFR (renal injury or dysfunction) will cause an increase in BUN
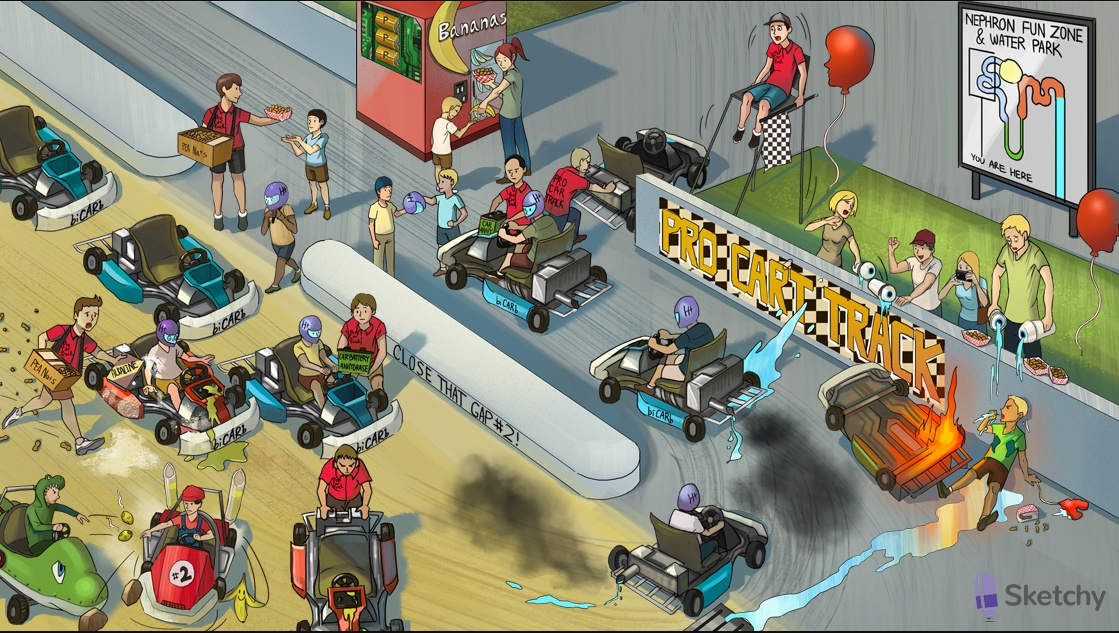
“Pro Car Track” absorbing BUN grease: once in the nephron BUN is actively reabsorbed at the Proximal Convoluted Tubule
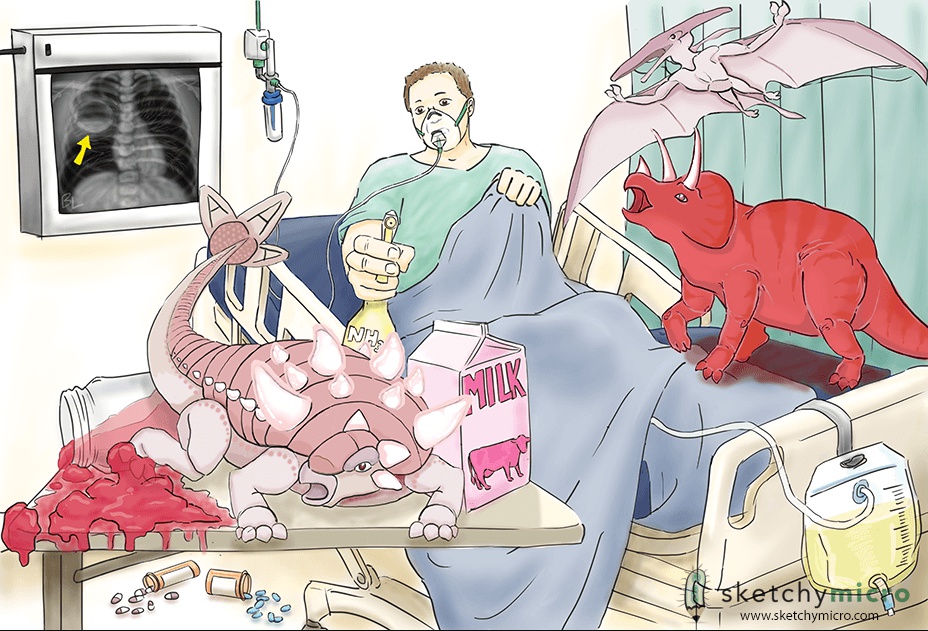
MEGAKING: Acute Kidney Injury (acute pre-renal, renal, or post-renal azotemia)
Trickle next to credit card: Acute Kidney Injury (AKI) manifests as increased serum creatinine and/or decreased urine output (oliguria)
Ketchup hemorrhage: hypovolemia or hemorrhage can cause PRE-RENAL AKI (kidney is hypoperfused)
Failing heart balloon: low output states (e.g. heart failure, shock) can cause PRE-RENAL AKI (kidney is hypoperfused)
BUN grease reabsorption: urea resorption in the proximal tubule is INCREASED during low perfusion states → INCREASED BUN/Cr ratio (>15)
Lifted BUN bag over credit card: increased BUN/Cr ratio (>15) in PRE-RENAL AKI
FENa fries dropping: decreased fractional excretion of sodium (FENa <1%) in PRE-RENAL AKI (sodium is conserved during low perfusion states)
“UP/UP N away!”: UNaPCr/PNaUCr (FENa equation used to assess ability to reabsorb sodium)
Pepper in the consOSMents: PRE-RENAL AKI is associated with a UOsm > 500 (concentrated urine to conserve volume)
Necrotic chocolate straw: acute tubular necrosis (ATN) is the most common cause of INTRINSIC RENAL AKI
Blue spotted kidney tray: acute interstitial nephritis (AIN) causes INTRINSIC RENAL AKI
Dripping glomerular curly straw: glomerulonephritis can cause INTRINSIC RENAL AKI
Falling BUN Bag over Credit card: BUN/Cr ratio <15 in INTRINSIC RENAL AKI (but both BUN and Cr are elevated)
Elevated FENa fries: FENa is >2% in INTRINSIC RENAL AKI (unable to reabsorb sodium)
Empty condOSMents bottle: INTRINSIC AKI is associated with a UOsm <350 (unable to conserve water)
Elevated BUN bag over Credit card: the BUN/Cre is >15 in POST-RENAL AKI (back-pressure enhances urea reabsorption)
Obstructive spit balls: bilateral nephrolithiasis can cause POST-RENAL AKI
BPH Fire hat: benign prostatic hyperplasia (BPH) can cause POST-RENAL AKI
Cancer crab buckle: cancer of the ureter, bladder, or urethra can also cause POST-RENAL AKI
Fallen BUN bag and Credit card: the BUN/Cr ratio can be decreased in severe or prolonged POST-RENAL AKI
Toys behind cracked kidney glass: AKI can cause hyperkalemia, acidosis, hypertension, and uremia (see chronic kidney disease video)

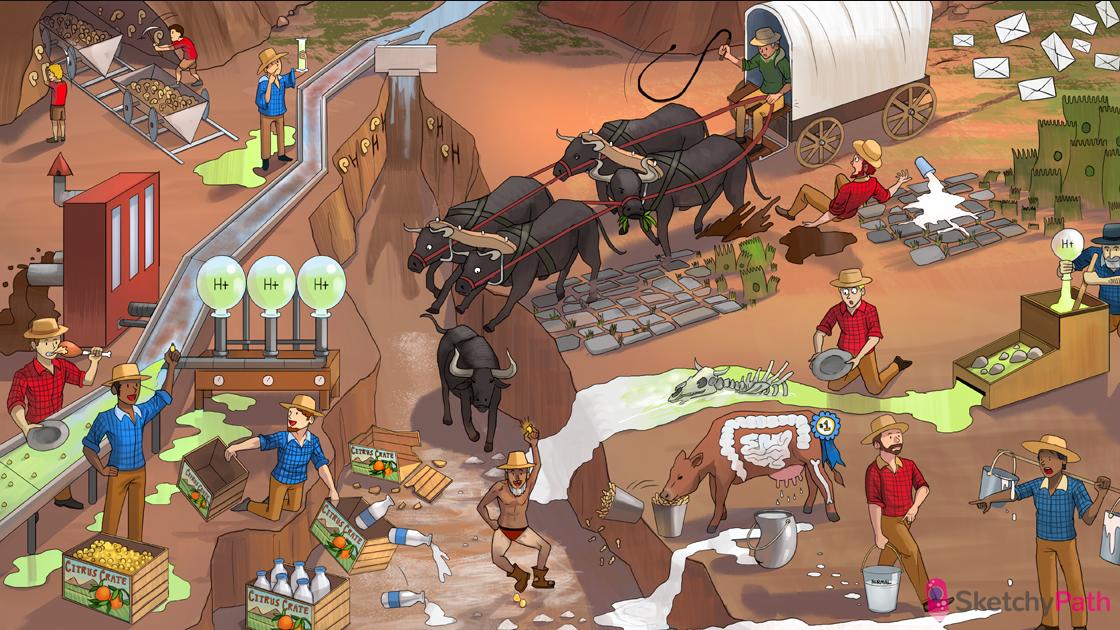
Necrotic muddy drain pipe: acute tubular necrosis (ATN) is the most common form of acute kidney injury (AKI)
Ischemic zombie: ATN is caused by ischemia of tubule cells
Empty kidney water gun: ATN is usually caused by decreased renal perfusion (prerenal AKI)
Bloody wound: severe blood loss → systemic hypoperfusion → prerenal AKI → ischemic damage to kidney → ATN
Broken heart string: MI → systemic hypoperfusion → prerenal AKI → ischemic damage to kidney → ATN
Constricted red exhaust pipe: ischemia damages endothelial cells → decreased nitric oxide (vasodilator) and increased endothelin (vasoconstrictor) production
Constricted red sleeve: ischemic injury to the endothelium of the afferent arteriole leads to vasoconstriction
Zombies stuck at AFFERENT entry way: vasoconstriction of the damaged afferent endothelium impedes blood flow to the glomerulus
Broken grounds filter rate: glomerular filtration rate (GFR) is decreased in ATN
Muddy epithelial leaves: ATN causes “muddy brown” casts in the urine sediment (sloughed tubular cells)
Obstructing epithelial leaves: sloughed epithelial cells accumulate in the tubular lumen, causing obstruction
Mud spilling on grounds filter rate: obstruction of tubular lumen by sloughed tubular cells in ATN further reduces GFR
Broken down PRO CART TRACK: The proximal convoluted tubule is particularly susceptible to ischemic injury in ATN
Broken down loop-de-loop: The thick ascending limb of the loop of henle is particularly susceptible to ischemic injury in ATN
Patchy tube lining: in ATN, the nephron will show dilated tubules with a patchy loss of epithelial cells
Broken tube edge and rusty holes: in ATN, sections of the nephron will show ruptured basement membrane and vacuolization of epithelial cells
“Come on IN”: the initial insult (e.g. MI, sepsis, hemorrhage) occurs during the INITIATION phase of ATN (lasts 36 hours)
Smiling clown face: the INITIATION phase of ATN is associated with fairly normal kidney function and urine output
Maintenance shed: AKI develops during the MAINTENANCE phase of ATN with severe metabolic derangements and reduced urine output (lasts 1-2 weeks after initial insult)
Cracked kidney on maintenance shed: the maintenance phase of ATN is associated with symptoms of AKI (e.g. oliguria, increased creatinine, fluid overload, metabolic abnormalities)
BUN bag: BUN is elevated during the maintenance phase of ATN
Credit card slot: creatinine is elevated during the maintenance phase of ATN
Trickle: the maintenance phase of ATN is associated with oliguria (<400mL/24hr)
Covering up with epithelial jacket: tubular re-epithelialization occurs during the recovery phase of ATN (!1-2 weeks after initial insult)
Wet crotch: the recovery phase of ATN is marked by profound diuresis (urine output up to 3-5 L/day)
Spilled banana peels, peanut shells, Calci-Yum cups, and magazine trash: the recovery phase of ATN can cause electrolyte abnormalities (e.g. hypokalemia, hyponatremia, hypocalcemia, and hypomagnesemia)
Toxic waste at the Pro Cart Track: the proximal convoluted tubule is the primary site of injury in NEPHROTOXIC ATN
Sai weapon: aminoglycosides can cause nephrotoxic ATN
Chomped chicken leg: damaged muscle (e.g. crush injury, rhabdomyolysis) can cause nephrotoxic ATN
Heme ninja stars: damaged muscle releases nephrotoxic heme pigments into the bloodstream → nephrotoxic ATN
Yin-yang: IV contrast can cause nephrotoxic ATN

Flaming kidney: tubulointerstitial nephritis (e.g. acute interstitial nephritis - AIN) is associated with acute renal interstitial inflammation
Anti-inflammatory fire extinguisher: NSAIDs can precipitate acute interstitial nephritis (AIN)
Furious kid under the loop de loop: furosemide (a loop diuretic) can precipitate AIN
Pencils in kidney: penicillin can precipitate AIN
Stinky sulfur eggs: sulfonamide drugs (e.g. TMP/SMX) can precipitate AIN
Degranulating bee hive: drug-induced interstitial nephritis can be mediated by a type I hypersensitivity reaction (cross-linking Ig-E on mast cells → release of proinflammatory substances)
Helper squire running by cage: drug-induced interstitial nephritis can be mediated by a type IV (“delayed-type”) hypersensitivity reaction (antigen presenting cells activate TH2 helper T-cells)
Blue lights dotting kidney: AIN shows interstitial edema with a diffuse inflammatory infiltrate on histology
Slingshot with pink granules: AIN can cause eosinophilia
Eo-slingshot granules in puddle: AIN can cause eosinophiluria
White knights, squires, and archers in puddle: AIN can present with white blood cell casts
BUN bag and credit card: AIN can present with elevated serum BUN and creatinine)
Trickling water: AIN can present with oliguria
Cracked kidney mirror: AIN causes intrinsic AKI (elevated serum BUN and creatinine and numerous metabolic and hemodynamic derangements)
Flaming head: AIN can present with fever
Spotted clown outfit: AIN can present with rash
Delayed demolition: AIN symptoms occur 1-2 weeks after inciting agent (type IV hypersensitivity reaction)
Chronic grandfather clock: chronic tubulointerstitial nephritis (TIN) (e.g. analgesic nephropathy)
Anti-inflammatory fire extinguisher: chronic NSAID use can cause analgesic nephropathy (chronic TIN)
Kicking in the BACK: Chronic pain patients (e.g. BACK pain, migraines) are at risk for chronic TIN due to chronic NSAID use
Pointy pyramids in renal tunnel: NSAIDs accumulate at the renal papillae (the tips of medullary pyramids)
Oxidizing sparks: NSAIDs cause injury to the renal interstitium via free radical damage
Patchy blue sparks: → NSAIDs cause patchy inflammation in the renal interstitium
Calcium deposits: NSAIDs cause calcification in renal papillae (in areas of chronic inflammation)
Fibrotic bush: chronic inflammation in analgesic nephropathy causes interstitial fibrosis
Decaying pyramids in renal tunnel: in analgesic nephropathy causes microvascular damage AND vasoconstriction of afferent renal vessels → ischemia → renal papillary necrosis
Shrunken kidney pendulums: chronic TIN causes chronic kidney disease → bilaterally small scarred kidneys
Lead paint cans: chronic lead exposure can cause chronic TIN (i.e. lead nephropathy)
“Liftium”: chronic lithium use can cause chronic TIN
Antibody lights: autoimmune diseases (e.g. Sjögren syndrome, lupus) can cause chronic TIN
Nephrotic
_..

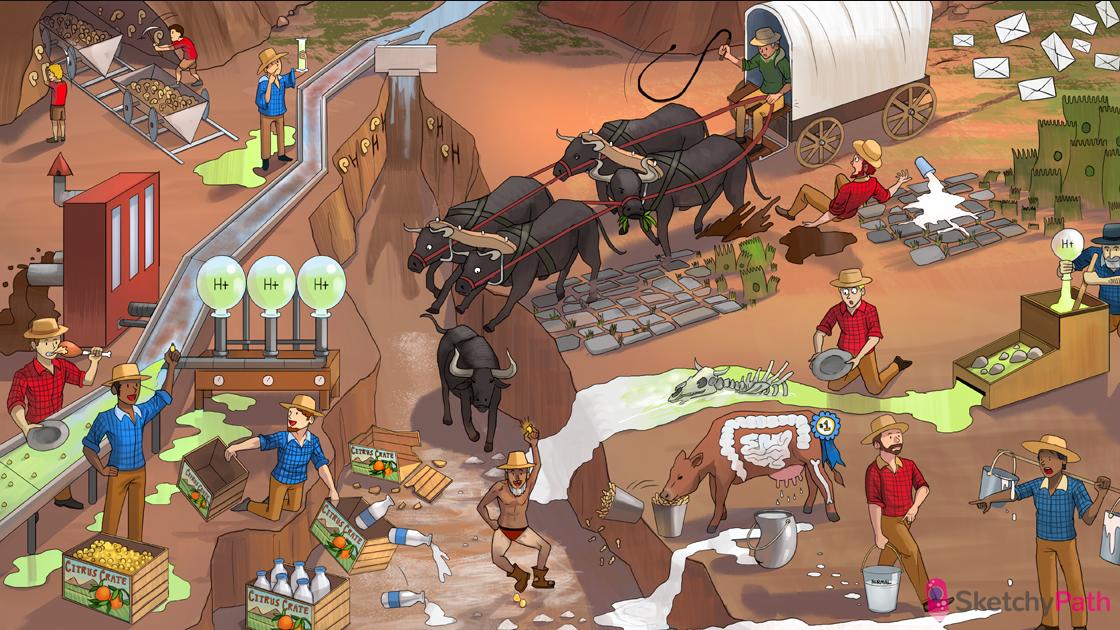
Endothelial shields: glomerular capillary (ENDOTHELIUM)
The wall: the glomerular basement membrane is thick, electron dense, and made of collagen, laminins, and glycoproteins
Minus signs: the GBM is normally negatively charged
Foot soldiers: podocytes (EPITHELIUM) have foot processes with filtration slits (selectively permeable)
Supportive field: the mesangium surrounds the capillaries and provides structural support to the glomerulus
Excretory river: Bowman’s space→ renal tubule
Falling minus bricks: injury to the basement membrane can cause loss of negative charge → NEPHROTIC syndrome
Cowering footsoldier: podocytes effacement, slit diaphragm disruption, depletion → NEPHROTIC SYNDROME
Coins: in NEPHROTIC syndrome, injury to the glomerulus via cytokines (NOT cellular infiltrate, inflammation) → NEPHROTIC syndrome
Meat cart #35: NEPHROTIC syndrome is characterized by marked PROTEINURIA (> 3.5 grams/day)
Falling album: NEPHROTIC syndrome is characterized by HYPOALBUMINEMIA due to loss of albumin into the urine (hyperalbuminuria)
Edematous king: hypoalbuminemia → decreased oncotic pressure → fluid shifts into interstitium → generalized edema (NEPHROTIC syndrome)
Butter in front of liver tent: hypoalbuminemia → liver synthesis of proteins (including lipoproteins) → hyperlipidemia (NEPHROTIC SYNDROME)
Fat oval pigs: fatty casts and “oval fat bodies” in urine (lipiduria)
Dropping throm-beaver cage: proteinuria includes loss of antithrombin III → hypercoagulable state
Firewood thrombus: decreased antithrombin III → increased thrombin activity (hypercoagulable state)
Stabbing in flank: hypercoagulable state → renal vein thrombosis ( flank pain, gross hematuria)
Wormy left pant leg: left renal vein thrombosis can cause left varicocele
Falling antibody keys: proteinuria includes loss of gamma-globulins in the urine → hypogammaglobulinemia → increased risk of encapsulated bacterial infections
Frothy river: massive proteinuria can cause frothy urine
MCD
_..

“MINIMUM”: minimal change disease primarily affects children and causes “minimal” changes on histology (normal light microscopy, no immune complexes on immunofluorescence)
Hugging kid foot soldiers: minimal change disease causes podocyte effacement and fusion (visible on electron microscopy)
Blowing nose: minimal change disease develops several weeks after an upper respiratory infection, allergic reaction, insect sting, or immunization
Photos falling from album: minimal change disease causes selective leakage of albumin (“selective albuminuria”) due to loss of negative charge on the basement membrane
Moon face: minimal change disease responds glucocorticoids
FSGS
_..

“FOCAL ATTACK”: focal segmental glomerulosclerosis (FSGS) is “focal” (affecting only some glomeruli)
“SEGMENTAL ATTACK”: focal segmental glomerulosclerosis (FSGS) is “segmental” (affecting only some segments of a glomerulus)
SCALY sclerotic snake: focal segmental glomerulosclerosis (FSGS) causes sclerosis (light microscopy shows: obliterated capillaries with hyalin deposition)
Hugging foot soldiers: FSGS causes podocyte effacement and fusion (visible on electron microscopy)
Cracked kidney rocks: FSGS frequently causes end stage kidney disease
Virus lantern: FSGS can be caused by viral infections (HIV, hepatitis)
Syringe: FSGS can be caused by heroin abuse or systemic disease (diabetes, hypertension, vasculitis, sickle cell)
Diabetic
_..

Glycosylated kidney lollipops: diabetic nephropathy generally causes a nephrotic syndrome
Wall thickened by pink deposits: early on, diabetic nephropathy causes basement membrane thickening (due to nonenzymatic glycosylation)
Big pink lollipop in mesangial field: later stage of diabetic nephropathy causes nodular glomerulosclerosis, characterized by Kimmelstiel-Wilson nodules (light microscopy shows pink round deposits of laminated mesangial matrix)
SCALY sclerotic snake: nodular glomerulosclerosis (diabetic nephropathy) causes sclerosis (light microscopy shows: obliterated capillaries with hyalin deposition)
Membranous
_..

Wall thickened by long cape: membranous glomerulopathy causes diffuse thickening of the glomerular basement membrane (visible on light microscopy)
Antibody arrows injuring foot soldier: membranous nephropathy can be caused by autoantibodies against the phospholipase A2 receptor on podocytes → leads to subepithelial antibody deposits). IgG, C3
Dome-like helmet decorated with spikes: subepithelial deposits have a “spike and dome” appearance on electron microscopy (in membranous glomerulopathy)
Wall engulfing antibody arrows: “spike” appearance is due to the basement membrane engulfing “domes” of subepithelial immune deposits (visible on electron microscopy in membranous glomerulopathy)
Crab chest plate: membranous nephropathy can be secondary to solid tumors (lung, breast, prostate, colon)
Viral quiver: membranous nephropathy can be secondary to viral infections (hepatitis B or C)
Lupus wolf: membranous nephropathy can be secondary to lupus erythematosus. RA
Fluorescent green arrows: immunofluorescence microscopy shows granular deposits of immunoglobulin and complement along the basement membrane (in membranous glomerulopathy)
Moon shield: membranous nephropathy can be treated with corticosteroids
Amyloid
_..

Armored lady: amyloidosis (a systemic disorder that involves deposition of misfolded proteins in tissues) can cause nephrotic syndrome
Armoured lady in mesangial field: in early renal amyloidosis, there are focal amyloid deposits within the mesangium
Armoured lady in capillary circle: in later renal amyloidosis, amyloid obliterates glomerular capillaries
Stained with red paint: amyloid appears pink when stained with Congo red
Green perfume bottle: amyloid displays apple green birefringence in polarized light
Nephritic
_..

Supportive field: the mesangium surrounds the capillaries and provides structural support to the glomerulus
Circle of endothelial warriors: glomerular capillary (ENDOTHELIUM)
The Great Wall: the glomerular basement membrane
Footsoldiers: podocytes (EPITHELIUM) have foot processes with filtration slits (selectively permeable)
Excretory river: Bowman’s space→ renal tubule
Endothelial warriors around fire: in nephritic syndrome, glomerular injury is a result of inflammation
First responders carrying away endothelial warrior: inflammatory infiltrate (including neutrophils) → glomerular capillary damage → hematuria and AKI (nephritic syndrome)
Dropped meats: nephritic syndrome causes proteinuria (>150 mg/day - less than nephrotic range of 3.5 g/day)
Blood in river: nephritic syndrome is characterized by hematuria (gross or microscopic)
Dysmorphic red soldier: nephritic syndrome presents with dysmorphic RBCs (hallmark of glomerular injury)
Collecting red helmets: nephritic syndrome presents with RBC casts (hallmark of glomerular injury)
White soldier in river: nephritic syndromes can present with WBC in the urine sediment
Collecting white helmets: nephritic syndrome can present with WBC casts
Raised BUN bag: nephritic syndrome can present with an elevated BUN and creatinine (AKI)
Trickle: nephritic syndromes can present with oliguria (AKI)
High pressure steam: nephritic syndromes can present with hypertension (due to salt and volume retention)
Puffy face: nephritic syndromes can cause periorbital (and less commonly peripheral) edema (due to salt and volume retention)
IgA
_..

IgA dummy soldiers in the field: IgA nephropathy (Berger disease) is caused by deposition of IgA and IgA immune complexes in the mesangium)
Blowing nose and grabbing stomach: IgA nephropathy may present 1-2 days after an upper respiratory or GI infection (abnormal IgA synthesis and glycosylation)
Berger: Berger disease (IgA nephropathy)
Shoeshine: Henoch-Schonlein purpura (HSP) causes a renal disease similar to IgA nephropathy
Blood trickling: IgA nephropathy usually presents with gross hematuria that lasts for several days
Periodic blood puddles: patients with IgA nephropathy may have episodic hematuria
Proliferating army in the field: focal or diffuse mesangial proliferation (IgA nephropathy, post-strep, diffuse proliferative, membranoproliferative glomerulonephritis, dense deposit disease
Granular green glow: immunofluorescence shows a granular pattern in the mesangium due to IgA immune complex deposition. Granular = immune complex
Moon-face shield: IgA nephropathy can be treated with glucocorticoids
PSGN
_..

Pyogenes pie: post-streptococcal glomerulonephritis (PSGN)
Pie on face and neckerchief: PSGN can occur after group A strep (Strep. pyogenes) infection, including pharyngitis OR skin infection
Pie in mesangial field: PSGN is associated with immune complex deposition in the mesangium
Pie behind endothelial soldiers: PSGN is associated with subendothelial immune complex deposition
Pie landing on the back hump of epithelial foot soldier: PSGN is associated with subepithelial (humps) immune complex deposition
“Week 3” on calendar: post-streptococcal glomerulonephritis (PSGN) occurs 1-3 weeks after a skin or pharyngeal infection with nephritogenic strains of group A strep
Cola bottles: hematuria in PSGN is often described as “cola-colored”
Proliferating army in the field: focal or diffuse mesangial proliferation (IgA nephropathy, post-strep, diffuse proliferative, membranoproliferative glomerulonephritis, dense deposit disease
First responders with blueberry pie: in PSGN, light microscopy shows marked leukocyte infiltration (lots of nuclei present) in the mesangium and endothelium
Granular green pie tins: in PSGN, immunofluorescence microscopy shows granular pattern (due to IC deposition)
Lysed donuts and helical donuts: serum antistreptolysin-O (ASO) and anti-DNase B titers may be elevated after a group A strep infection (ASO less likely with skin infection)
DPGN
_..

Diffusely proliferating lupus wolves: diffuse proliferative glomerulonephritis is the most common presentation of lupus nephritis
Antibody posts holding double helix: DNA anti-DNA immune complexes (seen in diffuse proliferative glomerulonephritis)
Double helical fence around endothelial soldiers: DNA anti-DNA immune complexes deposit in the subendothelial space (diffuse proliferative glomerulonephropathy)
Looped wire around endothelial soldiers: light microscopy shows “wire looping” of the capillaries due to subendothelial immune complex deposition (diffuse proliferative glomerulonephritis)
Green granular glow: immunofluorescence shows a granular pattern due to immune complex deposition
Moon-face shield: treatment of diffuse proliferative glomerulonephritis with glucocorticoids and cyclophosphamide may slow progression to chronic kidney disease
MPGN
_..

Membranous sash along wall: membranoproliferative glomerulonephritis (MPGN) causes diffuse GBM thickening
Lobulated shovel: light microscopy shows hypercellularity and enlarged, lobular glomeruli (MPGN)
Wall splitting: electron and light microscopy show splitting of the glomerular basement membrane due to ingrowth of mesangium (“tram tracking”) (MPGN)
Viral, bacterial, and antibody lanterns: MPGN can be caused by viral infections (hepatitis B or C), bacterial infections (endocarditis, shunt nephritis), or autoimmune diseases (due to chronic IC formation)
IC lanterns behind endothelial soldiers: immune complexes deposit in subendothelial space (MPGN)
DDD
Dense bomb deposits: dense deposit disease involves deposition of a material of unknown composition in the basement membrane
Dense ribbon: the GBM eventually transforms into a long irregular and extremely electron-dense ribbon (DDD)
Excessive complements: dense deposit disease is associated with overactivation of the alternative complement pathway
3 friendship bracelets: dense deposit disease is associated with the formation of the autoantibody, C3 nephritic factor → stabilized C3 convertase → overactive alternative pathway (low C3 with normal C4)
RPGN
_..

Deadly crescent weapon: rapidly progressive glomerulonephritis (RPGN) causes crescents in the glomerulus (rapid decline in kidney function)
Deadly IC mace: immune-complex mediated glomerulonephritides ( e.g. PSGN, diffuse proliferative glomerulonephritis, IgA nephropathy, HSP) can lead to RPGN
Decaying break in wall: on light microscopy, RPGN glomeruli will show segmental necrosis and breaks in the glomerular basement membrane
Scattered fibrous twigs: plasma proteins and fibrin deposit in the crescents formed in RPGN
Advancing epithelial army: crescent formation in RPGN is caused by epithelial cell proliferation from the capsule (parietal) → obliteration of Bowman’s space
Green granular glow: immunofluorescence microscopy shows a granular pattern in the immune complex glomerulonephritides progressing to RPGN
Crescent warrior shooting ankle: pauci-immune RPGN (no IC deposition) may be associated with anti-neutrophilic autoimmune vasculitides like Wegener’s granulomatosis (c-ANCA) and microscopic polyangiitis (p-ANCA)
Crescent warrior shooting wall: anti-GBM antibody-mediated RPGN (e.g. Goodpasture’s disease) is caused by antibodies directed against antigens in the GBM
Linear layer of green arrows: anti-GBM antibody-mediated RPGN shows a linear pattern on immunofluorescence microscopy
Blood on chest: while anti-GBM can be isolated to the kidney, involvement of the pulmonary capillary bed leads hemoptysis (Goodpasture’s syndrome)
“IV”: anti-GBM antibody-mediated RPGN involves IgG autoantibodies directed against type IV collagen in the GBM (also pulmonary capillaries in Goodpasture’s)

Horseshoe game: horseshoe kidney (the most common congenital renal malformation)
Caught on inferior post: during embryologic ascent, a horseshoe kidney gets stuck at the inferior mesenteric artery
X shaped pinwheel toys: Turner syndrome (monosomy X) is associated with horseshoe kidney
Cancer crab toy: horseshoe kidney increases risk of Wilms tumor
Stones in the dunk tank: congenital and cystic disorders of the kidney (e.g polycystic kidney disease) increased risk of kidney stones
Red dunk tank water: congenital and cystic disorders of the kidney (e.g polycystic kidney disease) can present with hematuria and flank pain (due to kidney stones)
Infected bladder cup: congenital and cystic disorders of the kidney (e.g polycystic kidney disease) can increase risk of urinary tract infections
Recurring bacterial lanterns: congenital and cystic disorders of the kidney (e.g polycystic kidney disease) can cause recurrent urinary tract infections
Dysplastic bunch of balloons: renal dysplasia (abnormal development of one or both kidneys) is the most common cystic disease in children
Dysplastic shark toy: renal dysplasia is associated with abnormal mesenchymal tissue (e.g. cartilage and bone)
Popped kidney balloon: renal agenesis (congenital absence of renal parenchyma)
Tightly wrapped Potter the bear: bilateral renal agenesis can result in oligohydramnios → Potter sequence (flattened nose, clubfeet, lung hypoplasia)
Kid hiding from bunch of kidney balloons: autosomal recessive polycystic kidney disease (ARPKD - symptomatic in early childhood)
Balloon with little cysts: ARPKD can present with bilaterally enlarged kidneys with diffuse small cysts on fetal ultrasound
Corduroy fibers: ARPKD is caused by a mutation in PKHD1 (fibrocystin gene)
Stepping in collecting duct: in ARPKD, cysts develop in the collecting ducts
Square tiles lining collecting duct: in ARPKD, cysts are lined by cuboidal epithelium
Tightly wrapped Potter the bear: ARPKD can cause oligohydramnios → Potter sequence (flattened nose, clubfeet, lung hypoplasia)
Bulging flank: ARPKD can present with bilateral flank masses
High pressure steam: ARPKD can cause hypertension in first months of life
Balloons caught in liver tree: ARPKD can cause cystic dilation of intrahepatic bile ducts, hepatomegaly, and hepatic fibrosis
Domino: autosomal dominant polycystic kidney disease (ADPKD - usually presents in adulthood)
Polygon pattern: ADPKD is caused by a mutation in PKD1 or PKD2 (less common) which code for polycystin-1 and polycystin-2
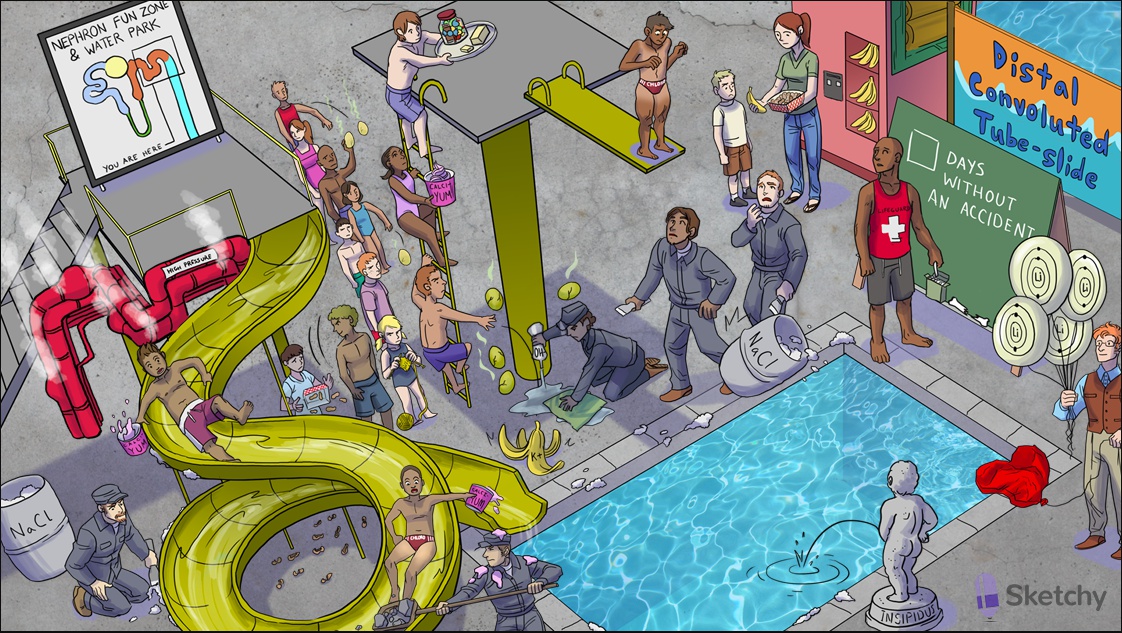
Nephron fun zone sign: cysts in ARPKD develop throughout the nephron
Growing balloons: cysts in ARPKD grow larger over time
High pressure steam: ADPKD can cause hypertension
Popping balloon hat: ADPKD can cause berry aneurysms in the circle of willis → subarachnoid hemorrhage
Balloons caught in liver tree: ADPKD can also present with hepatic cysts
Pancreatic balloon bag: ADPKD can also present with pancreatic cysts
Balloon belt: ADPKD can also present with diverticulosis
Central sponge gloves: medullary sponge kidney (multiple cysts in renal medulla)
Cleaning the end of the collecting duct: the cysts in medullary sponge kidney develop along the terminal collecting duct
Dilated kidney water balloon: horseshoe kidney can cause hydronephrosis

Fossilized kidney-shaped eggs: chronic kidney disease (CKD) (kidneys appear bilaterally shrunken with a red-brown, diffusely granular surface)
Empty grounds filter rate: CKD presents with decreased GFR
Coffee levels 1-5: the 5 stages of CKD are defined by GFR, with stage 5 being end-stage renal disease requiring dialysis
Credit card: CKD presents with increased creatinine (decreased GFR → decreased Cr clearance)
Photo album: CKD presents with albuminuria due to kidney damage
3 month expedition: CKD is diagnosed by 3 months of reduced GFR or elevated urine albumin
DiaSweeties candies: poorly controlled diabetes one of the MOST COMMON causes of CKD (due to microvascular damage)
High pressure steam: chronic hypertension is one of the MOST COMMON causes of CKD (due to microvascular damage)
Frayed glomerular knots: chronic glomerulonephritis can cause CKD
Kidney shaped bunch of balloons: polycystic kidney disease can cause CKD
Constricting red kidney straps: bilateral renal artery stenosis can cause CKD (due to ischemic nephropathy)
Pineapples: chronic pyelonephritis can cause CKD (due to progressive renal scarring)
Chomping glomerular reeds: initial injury leading to CKD
Mesozoic om nom nom
Tall glomerular reeds in the river: the remaining healthy glomeruli increase filtration to preserve GFR (adaptive hyperfiltration)
Dead glomerular reeds: the remaining hyperfunctioning glomeruli eventually become damaged by the extra load (labs start to show CKD)
Dry sclerotic glomerular reeds: CKD shows advanced scarring of the glomeruli on histology
Fibrotic kidney-shaped nest: CKD eventually leads to interstitial fibrosis
Acid volcano: CKD can cause metabolic acidosis due to impaired hydrogen excretion, impaired bicarbonate reabsorption, and accumulation of uric acid
Elevated bananas: CKD can cause hyperkalemia (due to decreased filtration of potassium due to decreased filtration of potassium and the H+/K+ buffering system with metabolic acidosis)
Wet body: CKD can cause fluid retention (leading to both diffuse and pulmonary edema)
Wax arm in water: CKD can present with waxy casts in the urine
High pressure steam: CKD can cause hypertension (due to volume overload)
Cracked draining kidney: CKD can cause a normocytic anemia (due to decreased erythropoietin production)
“P” fossils: CKD can cause hyperphosphatemia (due to decreased filtration and increased bone resorption in CKD-bone mineral disease)
Falling calci-yum ice cream: CKD can cause hypocalcemia (due to decreased vitamin D production and hyperphosphatemia)
Falling "D”: CKD can cause hypovitaminosis D (due decreased activity of 1-alpha-hydroxylase, and decreased production of 1,25-dihydroxyvitamin D)
PthD paleontologist: CKD can cause secondary hyperparathyroidism (hypocalcemia stimulates the parathyroid gland to release parathyroid hormone (PTH))
Bone fossil with dirt-filled holes: secondary hyperparathyroidism causes CKD-mineral and bone disorder (CKD-MBD) → osteitis fibrosa cystica (bone resorption causes cystic “brown tumors” that fill with fibrosis and hemosiderin)
Crumbling skeleton from Malaysia: secondary hyperparathyroidism and decreased vitamin D causes CKD-MBD → osteomalacia (decreased mineralization of bone osteoid)
“JUREASSIC”: CKD can cause uremia (elevated BUN)
Vomiting: uremia can cause nausea and vomiting
Flapping wings: uremia can cause asterixis (tremulousness) and other serious neurologic effects
Broken plates: uremia can cause platelet dysfunction → pathologic hemorrhage throughout the body
Cracked heart shell: uremia can cause serous pericarditis (or hemorrhagic if comorbid with platelet dysfunction)
Brain-head dino: uremia can cause significant neurologic symptoms (e.g. peripheral neuropathy, encephalopathy, seizure, coma, death)
Little itchy mammal: uremia can cause severe pruritis
Clogged coronary crown: CKD is an independent risk factor for developing coronary artery disease

Dilated pelvic and calyceal hoses: hydronephrosis (dilated renal pelvis and calyces)
Crushed deflated tire: hydronephrosis can cause pressure atrophy of the renal medulla and cortex
Tarnished papillary hubcap: sudden onset hydronephrosis can cause renal papillary necrosis
Horn sound: hydronephrosis can be diagnosed with ultrasound
Abdominal pocket mass: newborns with hydronephrosis can present with an abdominal mass
Kid kinking proximal hose: ureteropelvic junction obstruction is the most common cause of unilateral fetal hydronephrosis
Puddle girl spraying back water: vesicoureteral reflux (VUR) can cause hydronephrosis in children (unilateral or bilateral)
Right angled spray nozzle: perpendicular insertion of the ureters into the bladder can predispose to vesicoureteral reflux
Bladder juice boxes: VUR predisposes to recurrent urinary tract infections (UTIs)
Renal pineapple: VUR predisposes to chronic pyelonephritis → scarring
High pressure steam: VUR can cause hypertension (scarring from chronic pyelonephritis leads to renal insufficiency)
Obstructing top of urethral pole: posterior urethral valve can cause urinary tract obstruction in boys → hydronephrosis (bilateral)
Oh by all means, eat your fast food, enjoy your foam finger! Hey, even hack at a wall with a scalpel, guys...don't worry about this over here
Manly wolf shirt: posterior urethral valve is made up of a wolffian duct remnant
Tightly wrapped Potter the bear: posterior urethral valve can cause oligohydramnios → Potter sequence (flattened nose, clubfeet, lung hypoplasia)
Second dilated fire truck: obstruction distal to the ureters can cause bilateral hydronephrosis (e.g. VUR, posterior urethral valve, BPH)
Falling stones obstructing hose: urolithiasis is the most common cause of urinary tract obstruction in adults (can cause unilateral hydronephrosis)
Slashing scalpel axe: the ureters can become damaged or unintentionally ligated after pelvic surgery (causing urinary tract obstruction and unilateral hydronephrosis)
Recurrent bacterial lanterns: urinary tract outflow obstruction can cause recurrent UTIs
Stone striking flank: acute urinary tract obstruction (e.g. urolithiasis, surgical injury) can present as sharp flank pain radiating to the ipsilateral groin
Bleeding down pant leg: acute urinary tract obstruction (e.g. urolithiasis, surgical injury) can present with gross hematuria
Nauseated firefighter: acute urinary tract obstruction (e.g. urolithiasis, surgical injury) can present with nausea and vomiting
Crab buckle: pelvic and abdominal cancers (e.g. bladder cancer, uterine cancer) can cause chronic urinary tract obstruction and hydronephrosis (unilateral or bilateral)
Fibrous back wall of trees: retroperitoneal fibrosis can cause chronic urinary tract obstruction and hydronephrosis (unilateral or bilateral)
4 IgG lights: retroperitoneal fibrosis is associated with IgG-4 related systemic disease (including autoimmune pancreatitis, Riedel's thyroiditis, sclerosing aortitis)
Enlarged fire chief grabbing urethral pole: benign prostatic hyperplasia (BPH) is a common cause urinary tract obstruction in older men (can cause bilateral hydronephrosis)
Broken spinal power lines: neurogenic bladder (e.g. due to spinal cord injury, diabetes) can cause bilateral hydronephrosis
Fast food BUN bag and credit card: BILATERAL urinary tract obstruction can cause elevated serum BUN and creatinine (postrenal azotemia)
Calcium Oxalate Stones
_..
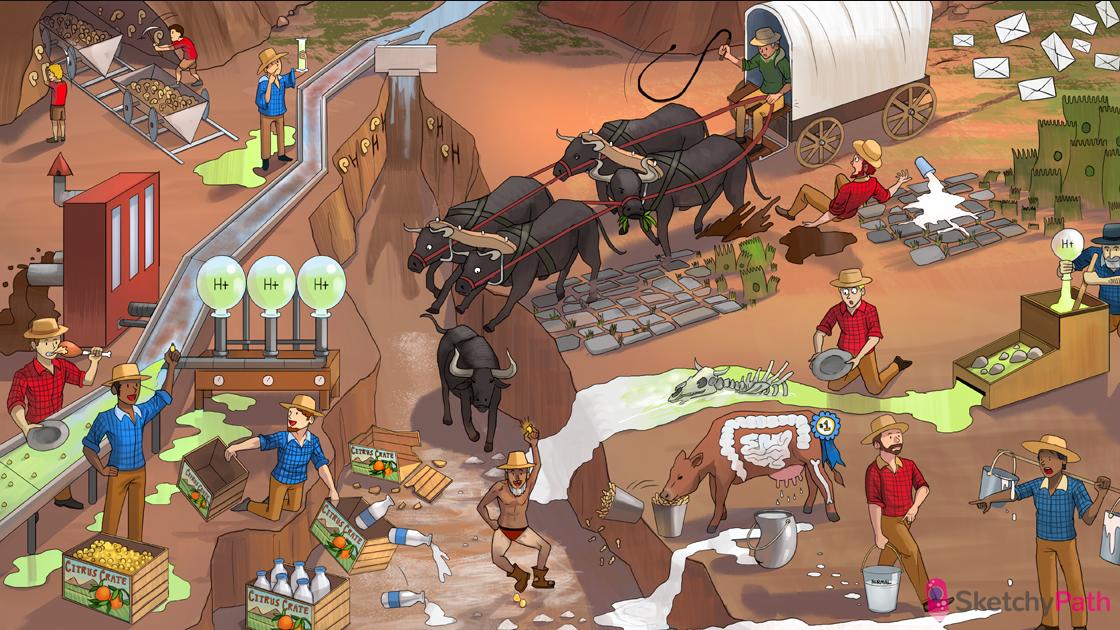
Dried up river deposits: all renal stones form due to supersaturation (adequate hydration is cornerstone of treatment)
Pale thighs: hydrochlorothiazide can help prevent calcium stone formation by increasing reabsorption of calcium in the distal tubule
Removing tube slide stones: thiazide diuretics can be used to prevent calcium stones (increased calcium reabsorption causes hypocalciuria)
_..
Milk dripping into river bed: high concentration of calcium in the renal tubule → calcium stones (calcium oxalate most common)
Ox in river bed: too much oxalate in the renal tubule → calcium oxalate stones
Milk dripping from udders: hypercalciuria (e.g. idiopathic, or due to hypercalcemia, chronic acidosis) can cause calcium stones
_..
Normal milk bucket: hypercalciuria with normocalcemia → calcium stones
First place dairy cow: hypercalciuria with normocalcemia is the most common metabolic abnormality causing calcium stones
GI cow spot: absorptive hypercalciuria (excessive gut absorption of calcium) is the most common cause of hypercalciuria with normocalcemia
Leaking kidney milk bucket: renal hypercalciuria (defect in proximal reabsorption of calcium) can cause hypercalciuria with normocalcemia
Bone cow spot: resorptive hypercalciuria (excess resorption of calcium from the bone) can cause hypercalciuria with normocalcemia
Elevated milk buckets: hypercalcemia (e.g. due to PHPT, cancer) can cause hypercalciuria and calcium stones
_..
Acid on bones: acidosis can cause hypercalciuria and calcium stones (calcium-phosphate buffer system)
Citrus crate with milk: citrate binds calcium in the renal tubules (soluble complex prevents stone formation
Acid miners: acidosis can cause calcium stones (due to hypocitraturia)
Acid miner grabbing citrus crate: acidemia promotes resorption of citrate from tubule → less citrate bound to calcium in tubule → calcium stones
_..
Spewing mud: diarrhea can cause calcium stones (due to volume depletion, and acidemia with hypocitraturia)
Meat eater: high protein diets can cause calcium stones (acidemia causes hypocitraturia)
Crushed citrus crate: vitamin C deficiency can cause calcium stones (due to hypocirtaturia)
Cow eating salty peanuts: increased dietary sodium intake can cause calcium stones (reduced Na+ and Ca2+ reabsorption in the nephron through their symporter)
Milk collecting in damaged GI path: fat malabsorption (e.g. Crohn's, short gut) binds calcium in the gut → GI absorption of unbound oxalate → calcium oxalate stones
_..
Spilling milk: decreased dietary calcium promotes calcium oxalate stone formation (due to increased GI absorption of unbound oxalate)
Oxen stampede: increased oxalate GI absorption (e.g. due to decreased dietary Ca2+, vegan diet, malabsorption) promotes calcium oxalate stone formation
Ox eating plants: pure vegan diets (without calcium supplementation) can cause calcium oxalate stones
_..
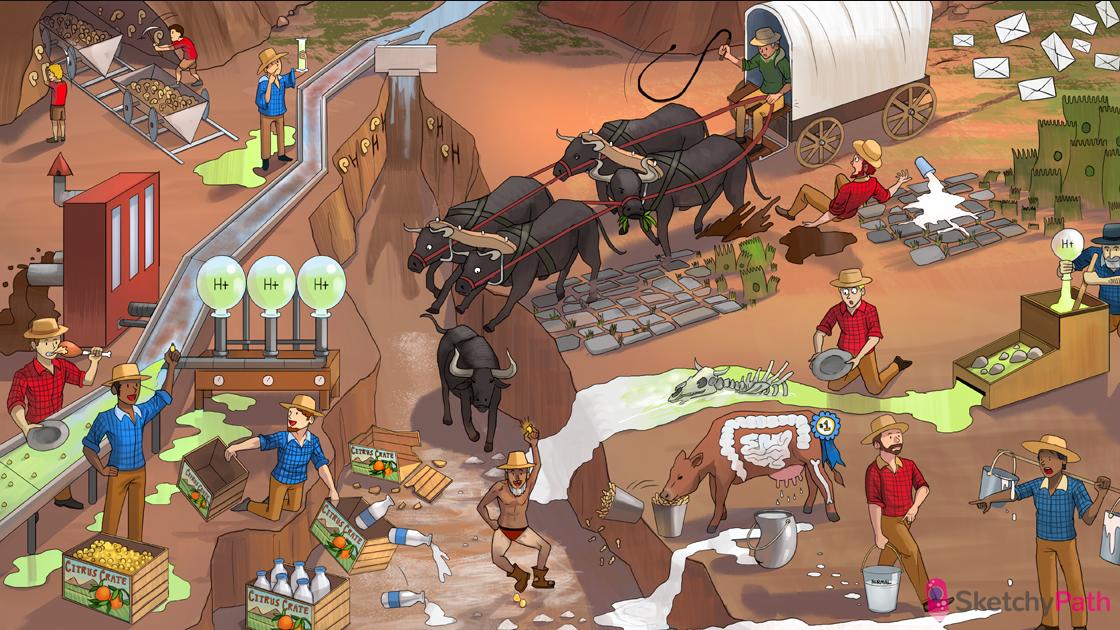
Fossil mining kids: calcium phosphate stones are the most common stone found in children
Acid cylinder: type 1 renal tubular acidosis (RTA) promotes calcium phosphate stone formation (acidemia, plus alkaline urine environment). Can also form with hyperparathyroidism
Elevated “pH” shape: alkaline urine environment promotes calcium pHosphate stone formation
Rocks on the inside track: CA inhibitors promote the formation of calcium phosphate stones (insoluble at high pH)
_..
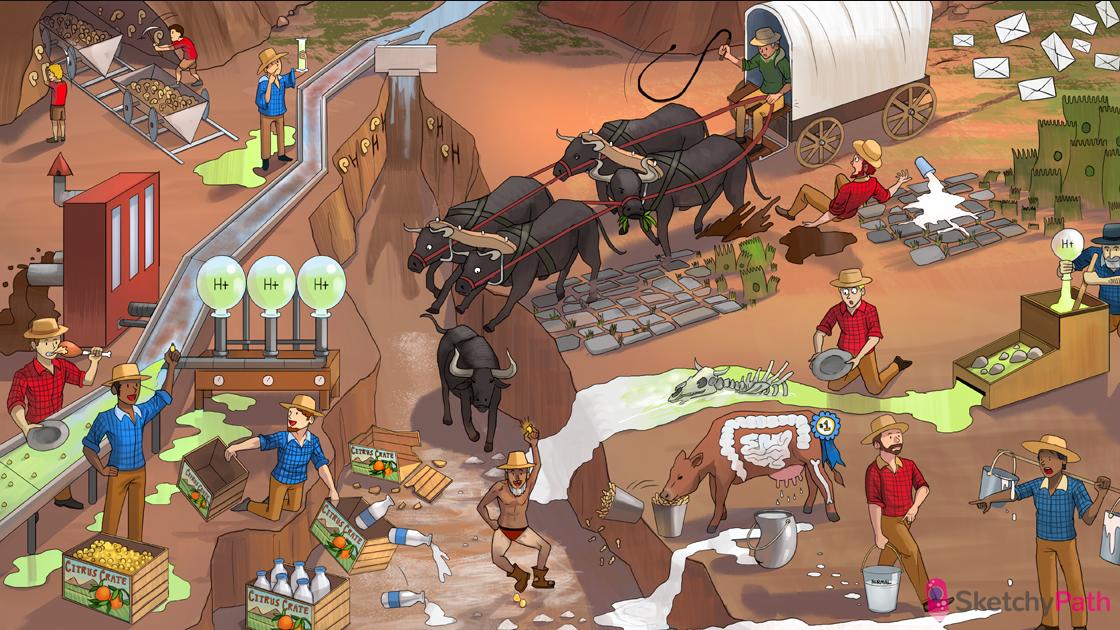
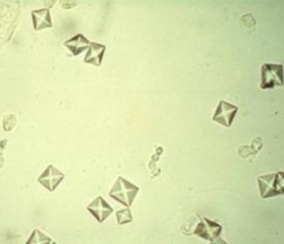
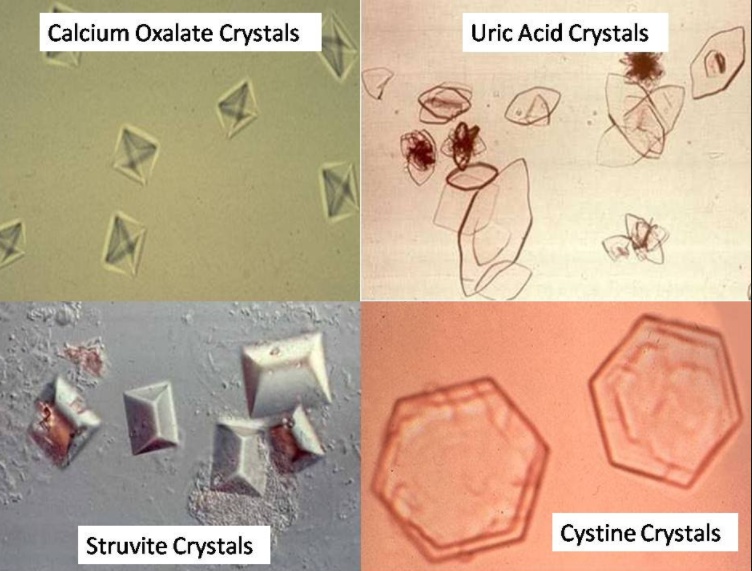
Envelopes from ox cart: calcium oxalate crystals have an “envelope” shape on microscopy
Wedge shaped fossil mine car: calcium phosphate crystals have an “elongated wedge” shape on microscopy

Mg stones
_..
Frontier MAP: magnesium-ammonium-phosphate (MAP) renal stones (second most common in adult)
Stag antlers: MAP stones can present as “struvite” or “staghorn” calculi
Urease spray: MAP stones can form during UTI with urease positive organism (urea → ammonium + CO2)
Blue puddles: basic urine decreases the solubility of phosphate → MAP stone formation
Goblet with ureteral straws: MAP stones can form during a UTI with a urease positive organism (e.g. Proteus, S. Saprophyticus, Klebsiella)

NH3: Urease positive, makes ammonium/CO2, alkaline environment, responsible for struvite stones precipation
horn of stag: Forms staghorn calculi in renal stones
Stone in hand: Alkaline environment can cause struvite stone production

_..
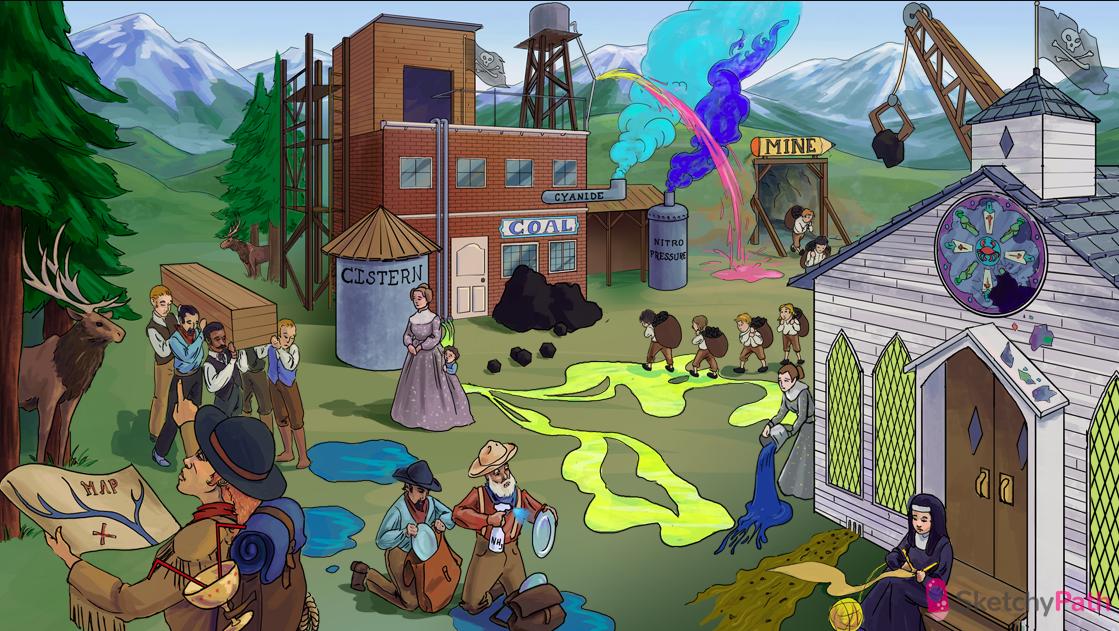
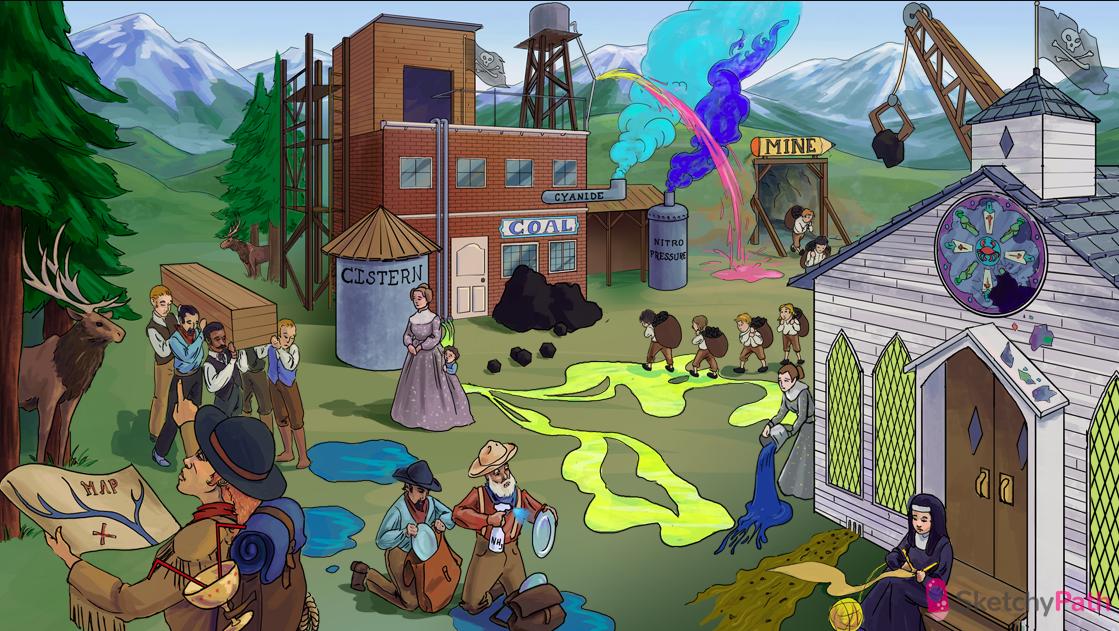
Needles in uric acid yarn: uric acid (urate) stones
Yarn ball on toe: gout causes hyperuricemia → uric acid stones
Raised white archers and knights: conditions with rapid cell turnover (e.g. leukemia and lymphoma) can cause hyperuricemia → uric acid stones
Falling shards: tumor lysis syndrome can cause hyperuricemia and uric acid stones
Mysterious acid secretions: idiopathic acidic urine (50% of patients with uric acid stone)
Acid puddles: uric acid stones preferentially form in an acidic urine environment
Draining mud: metabolic acidosis (e.g. caused by chronic diarrhea) → increased H+ excretion → uric acid stones
Dumping alkaline fluid: alkalinization of the urine (e.g. with potassium citrate, potassium bicarb) can effectively treat and prevent uric acid stones (acetazolamide)
Pure nun: allopurinol can prevent uric acid stones (with high cell turnover, or high purine metabolism)
_..
“Cistern”: cystine stones (occur in cystinuria)
Acid pools: cystine stones form preferentially in an acidic urine environment
COAL: cystinuria is caused by a defect in PCT reabsorption of cystine, ornithine, arginine, and lysine
Receding shy kid: cystinuria is caused by an autosomal recessive defect of resorption of amino acids in the PCT
Kids carrying coal: cystinuria usually presents in childhood with recurrent, non-calcium, renal stones
Stag antler: cystine stones can also present as “stag-horn” calculi
_..
Diamond windows: uric acid stones have characteristic diamond-shaped, yellow-brown crystals on microscopy
Coffin lid: MAP crystals have a characteristic “coffin lid” or rectangular prism shape on microscopy
Hexagonal coal briquettes: cystine crystals have a characteristic hexagonal shape on microscopy
_..
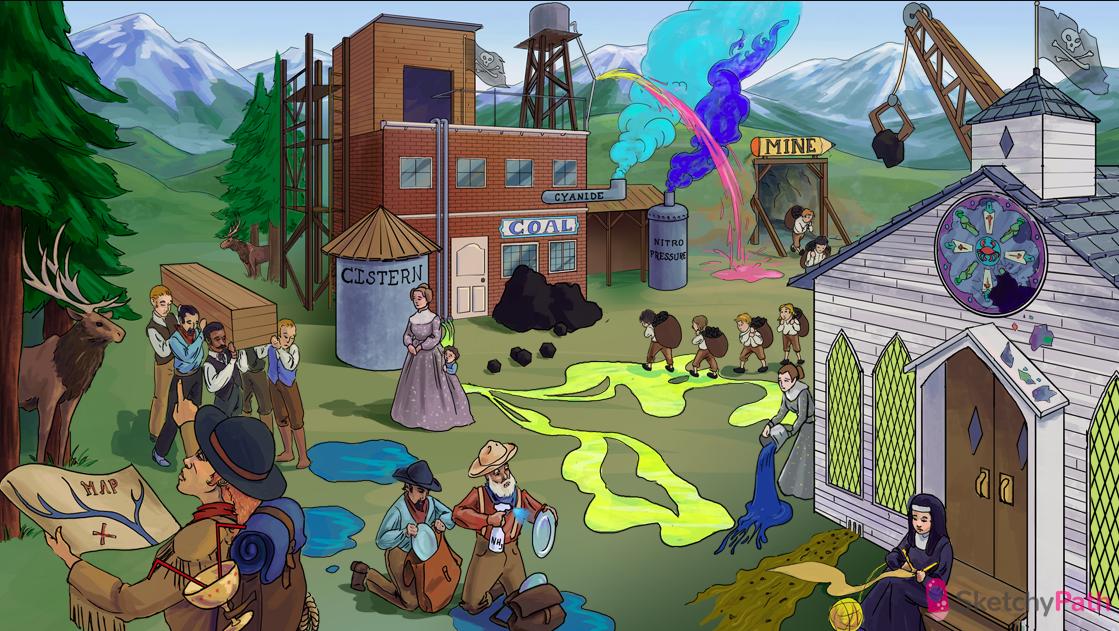
Blue “Nitro-pressure” smoke: the diagnostic test for cystinuria is the sodium cyanide-nitroprusside urine test
Pink stream in the smoke: urine of a patient with cystinuria will turn red-purple in a positive sodium cyanide-nitroprusside test
_..
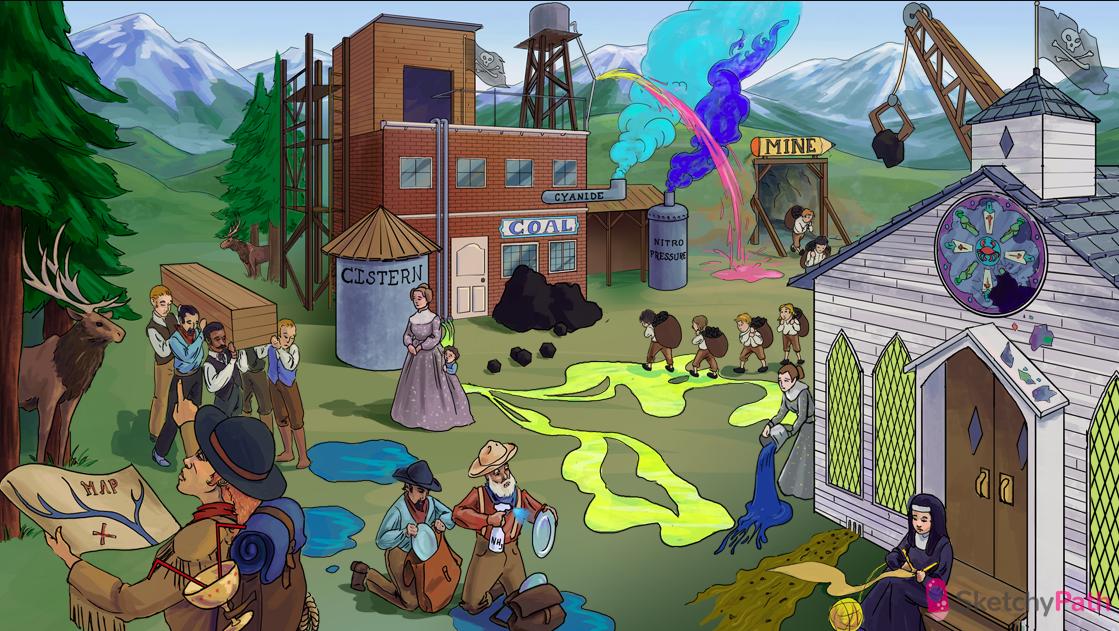
Pencil MINE: in severe cases, penicillamine can be used to chelate and lower cystine levels (prevent cystine stones)
Grasping crane: chelating agent (penicillamine)
_..
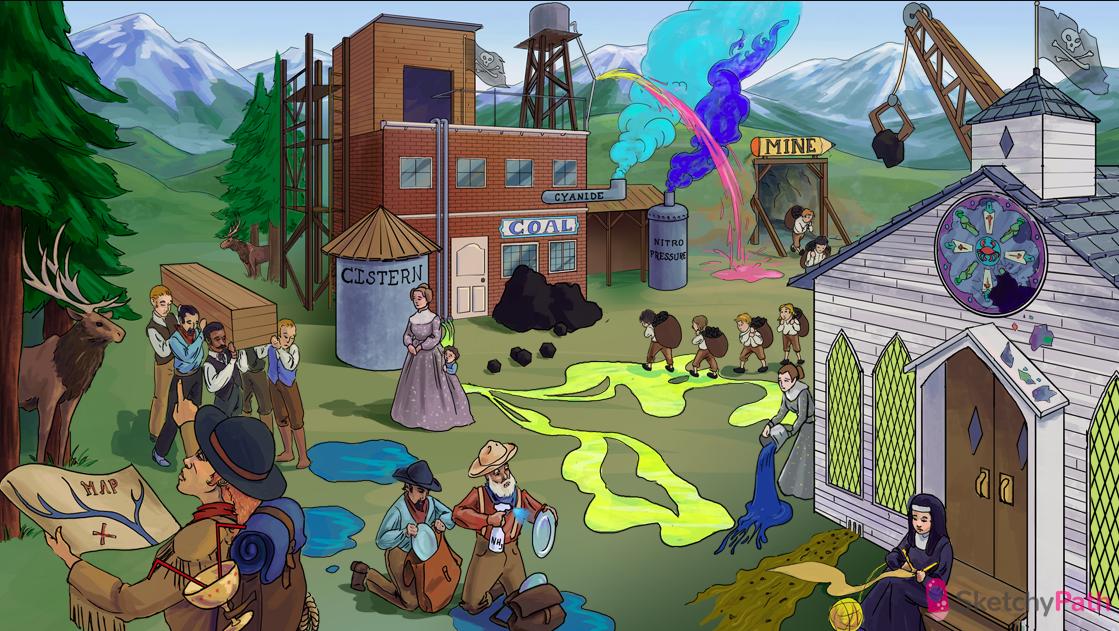
Translucent X-ray flag on church: uric acid and cystine stones are radiolucent (Calcium and MAP stones are radiopaque)
Translucent X-ray flag on COAL mine: uric acid and cystine stones are radiolucent (Calcium and MAP stones are radiopaque)
Last updated