Pretest Infectious Disease
Mumps
symptoms: fever, muscular pain (especially in the neck), headache, and malaise. In addition to the findings described, mumps typically swells to the opposite side in a day or so after symptoms appear on the first side. Other findings include redness and swelling at the opening of Stensen’s duct, edema and swelling in the pharynx, and displacement of the uvula on the affected side. A rash would not be expected.
Can have widespread effects and a variety of clinical presentations. Meningitis, pancreatitis, and renal involvement can occur as part of the disease.,
HIV mother
In certain situations, such as in an infant born to an HIV-positive mother, prophylaxis against P jiroveci (formerly known as P carinii) infection is instituted. While awaiting final determination of this infant’s HIV status, which can take several months, prophylaxis with trimethoprim-sulfamethoxazole starting at 6 weeks is usually appropriate.
DTAP, MMR, Hep B, HiB, Inactivated polio vaccine (IPV) is recommended in place of oral polio vaccine (OPV) for all patients now (not just immunosuppressed patients).
If children with HIV are exposed to measles, they should receive a protective dose of measles immunoglobulin regardless of their immunization history.
Pneumovax at age 2 and influenza vaccine are recommended annually.
Reye
path: acquired mitochondrial hepatopathy that results from the interaction of an influenza (or varicella) infection and aspirin use.
Symptoms: Patients initially present toward the end of a viral infection with sleepiness, emesis, and abnormal liver functions. As the disease progresses, the patient may develop seizures, coma, hyperventilation, and decorticate posturing. Ultimately they may develop respiratory arrest, loss of deep tendon reflexes (DTRs), and fixed and dilated pupils. Death is usually from cerebral edema and subsequent herniation.
labs: Liver enzymes and ammonia are elevated, but total bilirubin is not.
Shigellosis
symptoms:
watery stools for several days
severe infection with high fever
abdominal pain
generalized seizures
rare and fatal “toxic encephalopathy” known as Ekiri syndrome. In general, about 50% of infected children have emesis, greater than two-thirds have fever, 10% to 35% have seizures, and 40% have blood in their stool. Often, the seizure precedes diarrhea and is the complaint that brings the family to the physician. Fever usually lasts about 72 hours, and the diarrhea resolves within 1 to 2 weeks.,
diagnosis: clinical, confirmed with stool culture
treatment: Supportive care, including adequate fluid and electrolyte support, is the mainstay of therapy. Antibiotic treatment is problematic with resistance
Trichophyton Tonsurans
path: major cause of tinea capitis.
pt: infection within the hair follicle that is unresponsive to topical treatment alone and requires long-term oral therapy with griseofulvin or another antifungal for eradication.
symptoms: Scaliness and hair loss (kerion). Enlarged occipital lymph nodes are a common finding.
diagnosis: Fluorescence is absent on examination by Wood lamp. Diagnosis is made by microscopic examination of KOH preparation of infected hairs and by culture on appropriate media.,
Microsporum canis is an occasional cause of tinea capitis, and it does fluoresce under a Wood lamp.

sprinkling salt: Diagnosed with KOH prep of skin scrapings
lamps in woods in trees: "Wood's lamp can be used to diagnose Microsporum "
kerion:

Traction alopecia
Path: typically is seen in children who have their hair tied tightly in bows or braids
symptoms: the hair loss is linear following the area of traction, and is often associated with regional adenopathy.,

Alopecia areata
path: autoimmune
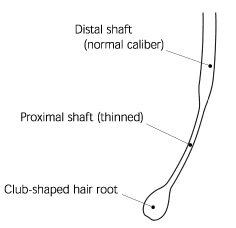
Symptoms: can appear similar to fungal infections, but the hairs near the active lesion often can be extracted with gentle traction resulting in an attenuated or catagen bulb at the termination of the hair shaft (exclamation hair); it does not produce a kerion as shown in the photograph.,

Leptospirosis
Leptospirosis is the most common zoonotic infection worldwide
pt: usually a history of exposure to dogs, cats, livestock, rats, or other wild animals is obtained.
symptoms: Two distinct courses of infection are described: “anicteric” and “icteric” (also called Weil syndrome). Both courses start with similar symptoms, as described in the case vignette, termed the “septicemic” phase.
The majority of cases are anicteric, and after a few days of symptom resolution, patients go on to the “immune” phase in which meningitic symptoms return and can last up to a month.
Less than 10% of leptospirosis cases are “icteric,” but these patients go on to have more severe symptoms involving liver and kidney dysfunction.
treatment: Penicillin and tetracycline (in children 10 years and older) are appropriate treatments, and seem to shorten the duration of the illness if started in the first week of symptoms. Some recommend prophylaxis with weekly doxycycline in endemic areas of the world.,
case: A 10-year-old boy was healthy until about 10 days ago when he developed 7 days of fever, chills, severe muscle pain, pharyngitis, headache, scleral injection, photophobia, and cervical adenopathy. After 7 days of symptoms he seemed to get better, but yesterday he developed fever, nausea, emesis, headache and mild nuchal rigidity. Cerebrospinal fluid (CSF) shows 200 white blood cells (WBC) per microliter (all monocytes) and an elevated protein.
EBV
Traditionally, heterophil antibodies can be detected when confirming a diagnosis of infectious mononucleosis. These antibodies may not be present, however, particularly in young children.
Alternatively, specific antibodies against viral antigens on the EBV can be measured.
Antibodies to viral capsid antigen (VCA) and to anti-D early antigen are elevated prior to the appearance of Epstein-Barr nuclear antigen (EBNA) and are therefore markers for acute infection.
IgG VCA and EBNA persist for life, whereas anti-D disappears after 6 months.

Osteomyelitis
cause: Although usually the result of hematogenous bacterial spread, particularly of S aureus, can follow an episode of deep cellulitis or septic joint and should be suspected whenever these occur.,
symptoms: Acute osteomyelitis tends to begin abruptly, with fever and marked, localized bone tenderness that usually occurs at the metaphysis. Redness and swelling frequently follow.
diagnosis: clinical, xray shows lytic lesions. Bone scans with radionuclides, however, can be useful in the diagnosis of osteomyelitis within 24 to 48 hours of symptoms and in its differentiation from cellulitis and septic arthritis. Magnetic resonance imagining (MRI) has become more widely used for the diagnosis of osteomyelitis, as it is very sensitive and specific.

TSST
Has been associated with the use of tampons and nasal packing.,
Pneumococcal bacteremia
pneumococcal: infant who appears otherwise normal, sudden onset of high fever, a marked elevation and shift to the left of the WBC count
Viral infections such as roseola occasionally can present in a similar fashion but without such profound shifts in the blood leukocyte count.
Neither typhoid fever nor diphtheria produces markedly high WBC counts; both are characterized by headache, malaise, and other systemic signs.
Dacrocystitis
path: infection of the nasolacrimal sac. In newborns it is associated with congenital nasolacrimal duct obstruction, which is seen in 6% of normal infants. Nasolacrimal duct obstruction is thought to be caused by the failure of epithelial cells forming the duct to canalize.
symptoms: swollen eyes, white exudate from punctum
treatment:
nasolacrimal massage and cleaning the area with warm washcloths
failure to open the duct by 6 months usually results in a referral to ophthalmology for surgical opening
antibiotics to clear the infection.,

Chalazion
Firm, nontender nodule that results from a chronic granulomatous inflammation of the meibomian gland.
The Meibomian glands are a special kind of sebaceous gland at the rim of the eyelids.,

Preseptal (periorbital) and orbital cellulitis may be distinguished by clinical examination.
Blood in the anterior chamber of the eye.,

Puncture Wound
Pseudomonas: Injuries through a tennis shoe are prone to pseudomonal infections because of the warm, moist nature of the shoe’s environment. Others: trauma, burns, swimming pools.
In contrast, a wound through a bare foot would be associated with cutaneous flora such as Staphylococcus
Dusty nails: tetanus
Last updated