Neonatal Rashes
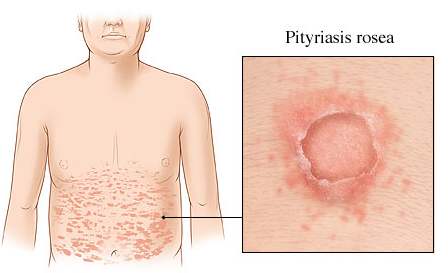
Pityriasis rosea
Symptoms: usually presents with a herald patch, a single round or oval lesion appearing anywhere on the body. Usually about 5 to 10 days after the appearance of the herald patch, a more diffuse rash involving the upper extremities and trunk appears. These lesions are oval or round, slightly raised, and pink to brown in color. The lesion is covered in a fine scale with some central clearing possible. The rash can appear in the Christmas tree pattern on the back, identified by the aligning of the long axis of the lesions with the cutaneous cleavage lines. The rash lasts 2 to 12 weeks and can be pruritic. This rash is commonly mistaken for tinea corporis, and the consideration of secondary syphilis is important.
Benign. Treatment is usually unnecessary but can consist of topical emollients and oral antihistamines, as needed. More uncommonly, topical steroids can be helpful if the itching is severe.,


Lichen Planus
rare in children.
Symptoms: It is intensely pruritic, and additional lesions can be induced with scratching. The lesion is commonly found on the flexor surfaces of the wrists, forearms, inner thighs, and occasionally on the oral mucosa.,
Seborrheic dermatitis
can begin anytime during life;
Symptoms: It frequently presents as cradle cap in the newborn period. This rash is commonly greasy, scaly, and erythematous and, in smaller children, involves the face, neck, axilla, and diaper area. In older children, the rash can be localized to the scalp and intertriginous areas. Pruritus can be marked.,
Wash with mild shampoo
Erythema toxicum
path: unknown etiology.
pt: It is found in about 50% of term newborns.
symptoms: Lesions are yellow-white and 1 to 2 mm in size, with a surrounding edge of erythema. This rash waxes and wanes over the first days to weeks of life. Examination of the fluid from these lesions demonstrates eosinophils.
treatment: benign, self-limited condition. No therapy is indicated.,

Pustular Melanosis
path: unknown etiology of the newborn period.
pt: It is more common in blacks than in whites.
symptoms: These lesions are usually found at birth and consist of 1- to 2-mm pustules that result in a hyperpigmented lesion upon rupture of the pustule. The pustular stage of these lesions occurs during the first few days of life, with the hyperpigmented stage lasting for weeks to months.
treatment: benign, self-limited disease. No therapy is indicated.,
Sebaceous Nevi
path:
pt:
symptoms: small, sharply edged lesions that occur most commonly on the head and neck of infants. These lesions are yellow-orange in color and are slightly elevated. They usually are hairless. Malignant degeneration is possible, most commonly after adolescence (remove before adolescents).,

Kasabach-Merritt
Seen with large vascular anomalies (ie, kaposiform hemangioendothelioma and tufted angioma).
Platelet and RBC sequestration within the vascular tumor causes peripheral thrombocytopenia, coagulopathy, and microangiopathic hemolytic anemia.
Treatment options include corticosteroids, α-interferon, and vincristine. Surgery frequently results in excessive bleeding.,
Case: After being delivered following a benign gestation, a newborn infant is noted to have a platelet count of 35,000/μL, decreased fibrinogen, and elevated fibrin spilt products. On examination you note a large cutaneous hemangioma on the abdomen that is purple and firm. Which of the following anomalies might also be expected in this infant?
Salmon Patches


A common minor vascular malformation seen on the glabella, eyelids, and nape of the neck in newborns; such lesions on the face are also called “angel kiss,” while lesions on the back of the neck are called “stork bite.”
Salmon patches (aka nevus simplex or flameus) are flat vascular lesions that occur in the listed regions and appear more prominent during crying. The lesions on the face fade over the first weeks of life. Lesions found over the nuchal and occipital areas often persist. No therapy is indicated.
Nevus Flammeus

Or port wine stain, is a large sharply demarcated pink to purple vascular malformation that can occur anywhere. Port wine stain involving the V1 distribution of the trigeminal nerve should raise the suspicion of Sturge-Weber syndrome.,
PHACE
posterior fossa malformations, large facial hemangiomas, arterial abnormalities, coarctation of the aorta, eye abnormalities, and sternal defects.
Infantile Fibrosarcoma
a malignant congenital tumor that can be easily mistaken for an infantile hemangioma; a high index of suspicion is required to investigate further if a “hemangioma” is not resolving as expected.,

Neonatal Acne
path: The condition results from maternal hormone transmission.
pt: which peaks at 2 to 4 weeks of age.
treatment: It resolves in a few weeks to months, and occasionally is severe enough to require treatment with agents such as tretinoin or benzoyl peroxide

.,
Milia
Path: cysts that contain keratinized material
symptoms: benign, tiny white bumps on the nose. Fine, yellowish white, 1- to 2-mm lesions scattered over the face and gingivae of the neonate. When on the palate, they are called Epstein pearls.
treatment: Commonly, these lesions resolve spontaneously without therapy.

.,
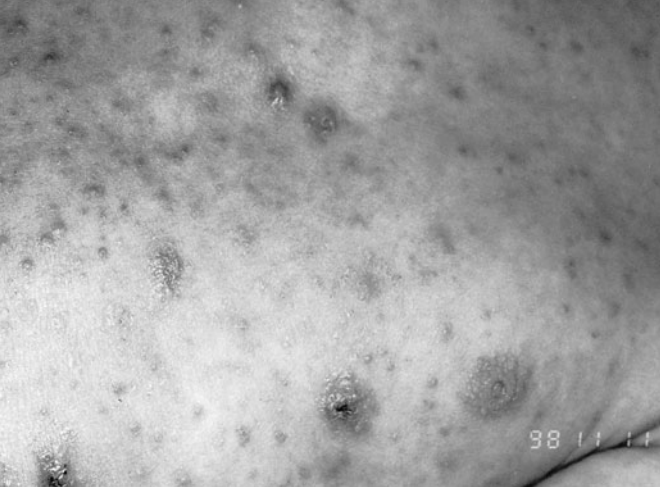
Scabies
path: Scabies is caused by the mite Sarcoptes scabiei var. hominis. Contagious
symptoms
Most older children and adults present with intensely pruritic and threadlike burrows in the interdigital areas, groin, elbows, and ankles; the palms, soles, face, and head are spared.
Infants, however, usually present with bullae and pustules, and the areas spared in adults are often involved in infants. The clinical manifestations closely resemble those of atopic dermatitis.
treatment: Gamma benzene hexachloride (lindane) can cause neurotoxicity through percutaneous absorption, especially in small infants and those with abnormal skin (impetigo, etc), and is, therefore, not recommended in children as first-line therapy for scabies. An excellent alternative—5% permethrin cream (Elimite)—is safer and is more often recommended.
Larva Migrans
aka creeping eruption
path: is caused primarily by dog or cat hookworms
cause: After exposure (such as walking barefoot on a beach and stepping where an infected dog has recently been) the larvae penetrate the skin at the epidermal-dermal junction and migrate at about 1 to 2 cm/d.
symptoms: The result is an intensely pruritic lesion as described in the vignette. a. He has an intensely pruritic lesion on his foot. The lesion is raised, red, serpiginous, and has a few associated bullae.
treatment: Left untreated the larvae die, but treatment with antihelminthic medications hastens resolution of symptoms.,

Chronic Seborrheic Dermatitis
if it is associated with failure to thrive, can result from histiocytosis X.,
Last updated