Pretest
General Pediatrics
Bells Palsy
Cause: HSV, Herpes Zoster, Lyme, follow recent URI
Treatment consists of maintaining moisture to the affected eye (especially at night) to prevent keratitis.
Prognosis: Complete, spontaneous resolution occurs in about 85% of cases, 10% of cases have mild residual disease, and about 5% of cases do not resolve.
Infantile: Occasionally infants will have a facial nerve palsy at birth; this is usually related to compression from forceps and spontaneously resolves over several weeks.
Juvenile rheumatoid arthritis
Symptoms: asymmetrically involves swelling in large joints, especially the knee, and often has no other symptoms.
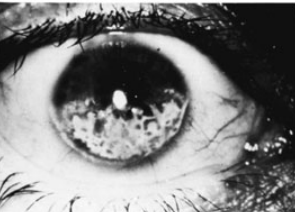
Association: A major morbidity is chronic uveitis, resulting in blindness. About 20% of girls who have the monoarthritis or pauciarticular form of juvenile rheumatoid arthritis have iridocyclitis (anterior uveitis) as their only significant systemic manifestation.
Because this eye disorder can require treatment with local or systemic steroids and develop without signs or symptoms, it is recommended that all children with this form of arthritis have frequent slit-lamp eye examinations.
Case:
A 4-year-old girl is noticed by her grandmother to have a limp and a somewhat swollen left knee. The parents report that the patient occasionally complains of pain in that knee. An ophthalmologic examination reveals findings as depicted in the photograph. Which of the following conditions is most likely to be associated with these findings?
SSSS
Demographic: seen most commonly in children less than 5 years of age.
Symptoms: The rash is preceded by fever, irritability, erythema, and extraordinary tenderness of the skin. Circumoral erythema; crusting of the eyes, mouth, and nose; and blisters on the skin can develop. Intraoral mucosal surfaces are not affected. Peeling of the epidermis in response to mild shearing forces (Nikolsky sign) leaves the patient susceptible to problems similar to those of a burn injury, including infection and fluid and electrolyte imbalance.
Labs: Cultures of the bullae are negative, but the source site or blood often may be positive.
Treatment includes antibiotics (to cover resistant S aureus) and localized skin care.
Prophylactic Heart Antibiotics
Among those currently recommended to receive antibiotic prophylactic treatment are patients for whom any heart infection would result in the highest incidence of adverse outcome:
previous history of endocarditis
prosthetic valve or material for repair
heart transplant patients
severe or partially repaired congenital heart defects
Human Bites
They can become infected with oropharyngeal bacteria, including S aureus, Streptococcus viridans, Bacteroidesspp, and anaerobes. A patient with an infected human bite of the hand requires hospitalization for appropriate drainage procedures, Gram stain and culture of the exudate, vigorous cleaning, debridement, and appropriate antibiotics.
The wound should be left open and allowed to heal by secondary intention (healing by granulation tissue rather than closure with sutures).
Animal Bites
Most experts suggest a short course of antibiotics should be started for cat, human, or monkey bites but not dog bites. Only 4% of dog bites become infected (and therefore do not necessarily need antibiotic prophylaxis), Pasteurella multocida is a common organism in infected cat and dog bites.Treatment with oral amoxicillin-clavulanate or erythromycin is recommended. Antibiotic prophylaxis is recommended.
Meningococcal vs HSP
HSP also has blood in urine.
Encopresis
definition: passage of feces in inappropriate locations after bowel control would be expected (usually older than 4 years).
demographics: Seen both with chronic constipation and overflow incontinence (retentive encopresis), and without constipation (nonretentive encopresis). Retentive encopresis is more common
There is leakage of liquid stool around a large fecal impaction, resulting in fecal soiling.
Treatment involves clearing the fecal mass, maintaining soft stools for a short period of time with mineral oil or stool softeners (3-6 months), and behavioral modification. Most children will grow out of this condition.
Genu varum
Bowlegs:
demographics: is a common finding in infants and toddlers younger than 2 years of age.
treatment: Improvement occurs spontaneously with time, and most children have straight legs by the time they are 2 years old.
Blount:
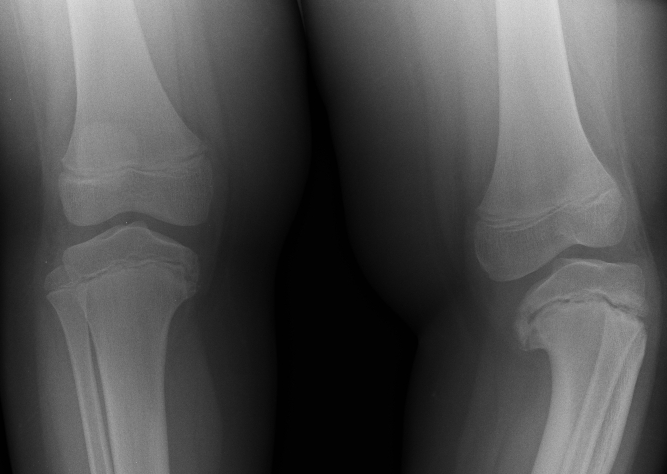
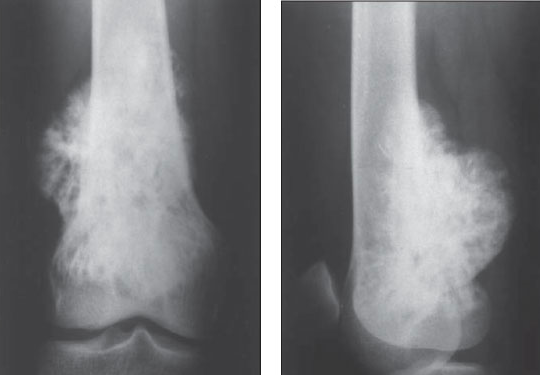
A few children with bowlegs, however, continue to progress and worsen, and in some cases the bowing is unilateral. This is termed Blount disease and is characterized by an abnormality in the medial aspect of the proximal tibial epiphysis.
Labs: Radiographically there is a prominent step abnormality with beaking at the proximal tibial epiphysis.
Treatment: Aggressive treatment is essential, as the disease can be rapidly progressive and lead to permanent growth disturbances. Bracing can be effective up to the age of 3; later correction may require surgery. Blount disease can occur in several forms: infantile (ages 1-3 years), juvenile (ages 4-10 years), and adolescent (age 11 years and older). Clinically, the findings are the same; in the adolescent group, radiograph findings are less prominent.

Legg-Calvé-Perthes disease
avascular necrosis of the femoral head
cause: Interruption of the blood supply by a currently unknown cause.
Demographics: Onset is usually between 2 and 12 years of age
symptoms: presents with a painless limp, although mild pain of the anterior thigh is common.,
Osgood-Schlatter
path: Repeated microfracture of the tibial tubercle at the insertion of the patellar tendon. This is an overuse injury
pt: young athletes
symptoms: presents with swelling and knee pain localized to the tubercle.
treatment: Improvement occurs with rest.,
Slipped capital femoral epiphysis (SCFE)
demographics: typically occurs in overweight adolescents or thin pt who had underwent rapid growth spurt
symptoms: presents with a limp. Pain when moving hips
labs: Radiographically, the capital femoral epiphysis is separated from the neck of the femur and remains in the acetabulum as the rest of the femur moves anteriorly.,
Gonococcal Arthritis
pt: adolescent
symptoms: arthritis and significant systemic signs and symptoms, including chills, fever, migratory polyarthralgia, and rash, are commonly seen
Breath Holding Spells
path
Cyanotic spells when upsetting or scolding the child.
Pallid breath-holding spells are less common and are usually caused by a painful experience (such as a fall)
pt: cyanotic spells are before 6 months of age, peak at about 2 years of age, and resolve by about 5 years of age.
symptoms: the child became cyanotic, unconscious, and had generalized clonic jerks. A few moments later the child awakened and had no residual effects.
treatment: Avoidance of reinforcing this behavior is the treatment of choice.
Diabetes
The criteria for diagnosis of diabetes:
a fasting glucose level ≥ 126 mg/dL
a 2-hour plasma glucose during an oral glucose tolerance test ≥ 200 mg/dL
symptoms of diabetes mellitus plus a random plasma glucose ≥ 200 mg/dL
Cyanide poisoning
pt: a rodenticide still found in some rural areas. A more common exposure occurs in fire victims
symptoms: The child first had a headache, but then became agitated and confused; while you are talking to the father in the ER the child begins to have a seizure and dysrhythmia on the cardiac monitor. The blood gas demonstrates a severe metabolic acidosis.
treatment: rapid treatment with antidote kit along with high levels of oxygen potentially are life saving.,
Neonatal Pneumonia
temperature instability, left shift CBC: infectious pneumonia instead of TTN or diaphgragmatic hernia
rapid onset of symptoms: chlamydia presents after weeks
syphilis causes pneumonia but has other features: hepatosplenomegaly, jaundice, rashes, hemolytic anemia, and others.
GBS
symptoms: The rapid onset of the symptoms (hours)
labs: low WBC count with left shift, and the depicted chest x-ray findings are typical of a patient with group B streptococcus (GBS) pneumonia
treatment: Appropriate management would include rapid recognition of symptoms, cardiorespiratory support, and rapid institution of appropriate antibiotics.
Strabismus
Light reflection
Infants can be screened for strabismus by observing the location of a light reflection in the pupils when the patient fixes on a light source. Normally, it should be in the center or just nasal of the center in each pupil.
Cover-Uncover
Another method of testing for strabismus is the “cover” or “coveruncover” test, using the principle that children with strabismus will use the “good” eye for fixation. By covering the good eye, the other eye will deviate.
Treatment
The aim of treatment is to prevent loss of central vision from foveal suppression of a confusing image in the deviating eye. This is accomplished by surgery, eyeglasses, or patching of the normal eye.
Persistence of a transient or fixed deviation of an eye beyond 4 months of age requires referral to an ophthalmologist.
Water temperature
Water temperature should be set to about 49°C (120°F); this will minimize the risk of accidental scald burns.
Milk consumption
In the older (2 yo) child, limiting fat to less than 35%, saturated fats and polyunsaturated fats each less than 10% of total calories, and cholesterol intake to less than 100 mg/1000 kcal/d usually results in switching from whole to skim or low-fat milk.
DTAP CI
For the DTaP, another contraindication is the occurrence of encephalopathy (such as coma, altered level of consciousness, or prolonged seizures) within 7 days of administration of the previous dose.
Head Lice
bug: peduculosis capitis
symptoms: intense itching
treatment
permethrin rinse. Do not use lindane for 2 month old because of neurotoxicity
Use of 1:1 vinegar-water rinse for hair for nit removal
Washing of all clothing and bedding in very hot water
Replacement of all commonly used brushes
Advice to the mother that treatment will again be necessary in 7 to 10 days

TB Meningitis
TB lingers for 3 weeks or longer
Cholesteaoma
path: A cholesteatoma may be congenital or acquired.
symptoms: It is a small sac lined with epithelium-containing debris. Acquired cholesteatoma can present in children with recurrent otitis media, or in the face of a chronically draining ear. The mass can grow aggressively, leading to CNS complications like facial nerve damage, hearing loss, and intracranial extension.
treatment: Referral to an otolaryngologist is required; a CT scan of the temporal bones can define the extent of disease.
Arsenic
Antidote is DMSA
Clonidine
miosis, bradycardia, and hypotension. Apnea, respiratory depression
Treatment includes aggressive PICU support and naloxone (which has variable effect).
Fragile X
The physical features become more obvious after puberty. They include a long face, large ears, prominent jaw, macroorchidism, hypotonia, repetitive speech, gaze avoidance, and hand flapping. Even in the absence of physical findings, boys of all ages with developmental delay, autism, and abnormal temperament of unknown cause probably should be tested.,
Seizures
path: The most helpful historical detail for acute management of this patient is the dilution of the formula, especially in light of the history of poor growth. Over time, inappropriate dilution can cause hyponatremia and water intoxication, leading to seizure activity.
treatment: Slow correction of the sodium is curative. The technique used to correct the patient’s hyponatremia depends on the etiology. In this case the child likely has chronic hyponatremia from poor intake. If the child continues to seize, 3% sodium chloride may be used to rapidly increase serum sodium and, theoretically, decrease cerebral edema. Otherwise, starting the child on a regular formula and eliminating excess water will correct the deficiency over time.
Craniotabes
sign of rickets
Soft occiptal bone, buckle under pressure like ping pong ball.,
Frost
Frostnip appears as blanching of the skin with transient numbness and paresthesias that resolves with rewarming. It is characterized by lack of ice crystal formation in the tissues and absence of tissue loss.
Trench foot results from prolonged exposure to a wet nonfreezing cold environment that produces peripheral neurovascular damage without ice crystal formation. This neurovascular damage manifests as pain, paresthesia, pallor, pulselessness, and paralysis. Trench foot is a reversible condition if diagnosed and treated early. Patients with trench foot have a better prognosis than patients with frostbite.
Frost bite: same as above two but with gangrene and ischemia of tissues.
Pernio (chilblains/cold sore) is less severe than trench foot and consists of painful inflammatory skin lesions caused by chronic repeated exposures to damp, nonfreezing cold temperatures. It is characterized by localized edema, erythema, plaques, nodules, vesicles, or bullae that appear as long as 12 hours after the injury. It is more common in young women.
Hypothermia, defined as core body temperature of less than 35°C, usually occurs as a concurrent disease.
Frostnip
Small, firm, white, cold patches of skin in exposed areas; treatment is rewarming the areas before they become numb.,

Trench Foot
Occurs with prolonged exposure to cold and/or moisture. The foot will become cold, numb, pale, edematous, and clammy. A prolonged autonomic disturbance after this condition can persist for years.,

Frostbite
Condition in which tissue is frozen and destroyed. There is initial stinging, followed by aching, culminating in numb areas. Once rewarmed, the area becomes red, blotchy, and painful. Gangrene may develop.,

Chilblains
path: Small, ulcerated lesions on exposed areas such as the ears and fingers. Lesions may last 1 to 2 weeks.
symptoms: symptoms of chilblains and frostnip are actually quite different. Chilblains presents with slight swelling of the toes and redness. The toes and forefoot have a dull ache that is not relieved by rest. With frostnip the affected skin blisters and has a red, brown or wheat colored crust. Pain is described as a burning type of pain.

Cold panniculitis
Destruction of fat cells caused by exposure to cold weather or a cold object; in this case, the child had “Popsicle panniculitis,” which is usually a benign condition that self-resolves.,
Popsicle panniculitis:

Vitamin Deficiencies
Riboflavin
path: It occurs because of poor intake, reduced absorption in patients with biliary atresia or hepatitis, or poor absorption in those receiving probenecid, phenothiazine, or oral contraceptives.
Signs and symptoms include cheilosis, glossitis, a variety of ocular problems (keratitis, conjunctivitis and corneal vascularization) and seborrheic dermatitis.,
Biotin
deficiency result in dermatitis/seborrhea.,
Pyridoxine
drugs: isoniazid, penicillamine, corticosteroids, and anticonvulsants
symptoms: Seizures, peripheral neuritis, dermatitis, and microcytic anemia are commonly seen evidence of deficiency.,
Folate
It produces megaloblastic anemia, glossitis, pharyngeal ulcers, and impaired immunity.,
Toxins
Phenothiazine
symptoms: can cause an idiosyncratic reaction causing extrapyramidal symptoms such as oculogyric crisis (prolonged involuntary upward deviation), tremors, torticollis, opisthotonus (arch back), and dysphagia. He is alert and oriented, but complains of a muscle spasm in his neck, making his head lean on his right shoulder.
treatment: These dystonic symptoms respond surprisingly quickly to the intravenous or intramuscular administration of diphenhydramine (Benadryl).,
Lead vs iron toxicity
Lead:
Ca DMSA, dimercaprol
Iron:
deferoxamine
Vitamin Excess
Vitamin A: slows normal growth and causes hyperostosis (excess bone growth), hepatomegaly, increased ICP (headache, vomiting), and drying of skin (desquamation, alopecia, itching).,
Nicotinic acid (niacin): a vasodilator, causes skin flushing and pruritus; long-term use can cause tachycardia, liver damage, hyperglycemia, and hyperuricemia.,
Vitamin C: in addition to causing kidney stones, diarrhea, and cramps, also causes an increase the normal requirement for the vitamin when large doses are discontinued.,
Vitamin D: can cause nausea, diarrhea, weight loss, polyuria, and soft-tissue calcification of heart (decreased Q-T interval), kidney, blood vessels, bronchi, and stomach.,
Pyridoxine (B6): can result in sensory neuropathy with altered sensation of touch (ataxia), pain, and fever.,
Isotretinoin
teratogenic effects including fetal death, hydrocephalus, CNS defects, microtia/anotia, small or missing thymus, conotruncal heart defect, and micrognathia.,
Microtia is a congenital deformity where the pinna (external ear) is underdeveloped:

Urinary Tract
Labial Adhesion
You are seeing a 4-year-old girl with the physical examination finding shown below. She has no significant past history. The most appropriate management is which of the following?
b. Estrogen cream
A usually benign condition in which the labia minora are fused. Fusion ranges from a small area to the entire area between the clitoris and the fourchette.
Cause and demographics: It is most common in young girls who are in the low estrogen state of preadolescence. Sometimes urine pooling can cause an increased risk of urinary tract infection.
Treatment can be merely observation, as the condition should resolve with the estrogenization that occurs with puberty. Nightly application of an estrogen cream for a week resolves this condition in the majority of patients. However, as recurrence is common, patients must be instructed to apply daily petrolatum for a month or two after separation.,
Estrogen Withdrawal
This patient has a physiologic discharge related to estrogen withdrawal. Examination can exclude vaginal trauma, and the history makes sexual abuse unlikely. Imaging is not indicated at this point. Parents should be reassured that it will resolve in a few weeks.
Prune Belly Syndrome
Demographics: a malformation that occurs mostly in males
Symptoms: characterized by a lax, wrinkled abdominal wall, a dilated urinary tract, and intra-abdominal testes. Additional urinary tract abnormalities include significant renal dysfunction or dysplasia. Oligohydramnios and commonly associated pulmonary complications, such as pulmonary hypoplasia and pneumothorax, are seen. Congenital hip dislocation, clubfeet, and intestinal malrotation with possible secondary volvulus can occur. Cryptoorchidism association.
Inheritance: There does not appear to be a genetic predisposition to prune belly syndrome.,
The delivery of a newborn boy is remarkable for oligohydramnios. The infant (pictured) is also noted to have undescended testes and clubfeet, and to be in respiratory distress. Which of the following is the most likely diagnosis to explain these findings?
A 17-year-old boy is brought to the emergency department by his parents with the complaint of coughing up blood. He is stabilized, and his hemoglobin and hematocrit levels are 11 mg/dL and 33%, respectively. During his hospitalization, he is noted to have systolic blood pressure persistently greater than 130 mm Hg and diastolic blood pressure greater than 90 mm Hg. His urinalysis is remarkable for hematuria and proteinuria. You are suspicious the patient has which of the following?
b. goodpastures
A 1-year-old child presents with failure to thrive, frequent large voids of dilute urine, excessive thirst, and three episodes of dehydration not associated with vomiting or diarrhea. Over the years, other family members reportedly have had similar histories. Which of the following is the most likely diagnosis?
c. DI
Fanconi Anemia
Symptoms: nonspecific findings of anorexia, polydipsia and polyuria, vomiting, and unexplained fevers,
Labs: Laboratory abnormalities of glucosuria, normal blood sugar, abnormally high urine pH in the face of mild or moderate serum hyperchloremic metabolic acidosis, and mild albuminuria in the presence of normal serum protein and albumin
Inheritance: FS can be hereditary or acquired; hereditary forms are usually secondary to a genetic abnormality such as cystinosis, galactosemia, Wilson disease, and some mitochondrial abnormalities.
Acquired: A number of agents can cause FS, including gentamicin (or other aminoglycosides), outdated tetracycline, cephalothin, cidofovir, valproic acid, streptozocin, 6-mercaptopurine, azathioprine, cisplatin, ifosfamide, heavy metals (eg, lead, mercury, cadmium, uranium, platinum), paraquat, maleic acid, and glue sniffing (toluene).
A 6-month-old infant has poor weight gain, vomiting, episodic fevers, and chronic constipation. Laboratory studies reveal a urinalysis with a pH of 8.0, specific gravity of 1.010, 1+ glucose, and 1+ protein. Urine anion gap is normal. Serum chemistries show a normal glucose and a normal albumin with a hyperchloremic metabolic acidosis. Serum phosphorus and calcium are low. What is the best diagnosis to explain these findings?
Glans Adhesion
Glans adhesion
In about 90% of boys during their first 3 years of life, adhesions between the glans and the prepuce lyse and the distal portion of the foreskin loosens, thus allowing the glans to be exposed. The collection of cellular debris under the foreskin, extruded from under the foreskin, is sometimes deemed abnormal by parents; it requires no treatment.
Phimosis
Phimosis (inability to retract the foreskin) is normal in the first years of life and is considered physiologic; inability to retract the foreskin after an age when it would be expected (about 3 years) is considered pathologic phimosis.
Paraphimosis
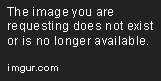
painful condition occurring when the foreskin gets retracted and trapped behind the glans and, because of edema and venous congestion, cannot be relocated into its normal position.,  ## Vesicoureteral Reflux After her first urinary tract infection, a 1-year-old has a voiding cystourethrogram with findings shown below. Which of the following is the most appropriate treatment option?

The radiograph shows reflux into the ureters and into the kidney, with dilation of the renal pelvis, making the diagnosis of vesicoureteral reflux. The higher the reflux into the renal system, especially if the renal pelvis is dilated, the more likely it is for renal damage to occur; the grading system is based upon these radiographic observations.
Grade I VUR is reflux of urine into an undilated ureter.
Reflux into the ureter and collecting system without dilatation is called grade II.
Grade III lesions have dilatation of the ureter and collecting system without blunting of the calyces.
Grade IV lesions are characterized by blunting of the calyces
Grade V lesions demonstrate even more dilatation and tortuosity of the ureter.
Low-grade lesions (grade I and grade II) are conservatively managed with close observation, daily low-dose antibiotics, and urinalyses and cultures every 3 to 4 months. Grade V lesions (and some grade IV lesions) require surgical reimplantation of a ureter if the findings persist. Lesions in between these two extremes are treatment dilemmas.
Physical examination of a baby boy shortly after birth reveals a large bladder and palpable kidneys. The nurses note that he produces a weak urinary stream. A voiding cystourethrogram is shown below. He appears to be otherwise normal. Which of the following is the most likely diagnosis?
b. posterior urethral valve
Acute Lobar Nephronia
The middle of the spectrum between pyelonephritis and renal abscess.
Symptoms: Patients have prolonged fever curves despite appropriate antibiotics.
Diagnosis: A CT scan is most useful in diagnosing nephronia, but a renal ultrasound can identify the process as well.
Treatment is prolonged IV and then PO antibiotics. Shorter courses like the typical treatment for pyelonephritis can lead to recurrence and renal abscess.
A 5-year-old girl without past history of UTI is in the hospital on antibiotics for Escherichia coli pyelonephritis. She is still febrile after 4 days of appropriate antibiotics. A renal ultrasound revealed no abscess, but a focal enlargement of one of the lobes of the right kidney. CT of the abdomen reveals a wedgeshaped area in the right kidney distinct from the normal tissue with minimal contrast enhancement. Appropriate management of this patient includes which of the following interventions?.,
Headache and BP
Routine BP measurement is performed on children of age 3 and beyond and for subgroups of children at younger ages, including children who were premature, had frequent urinary tract infection, had umbilical artery catheters, and so on.
Hypertension is usually asymptomatic, but with marked hypertension (that which is demonstrated by this 4-year-old) children can develop headache, dizziness, visual disturbances, irritability, and nocturnal wakening.
Hypertensive encepha-lopathy can be preceded or accompanied by vomiting, hyperreflexia, ataxia, and focal or generalized seizures. Isolated facial nerve palsy can be the sole manifestation of severe hypertension.
Isolated left ventricular hypertrophy, decreased urine output, and abdominal bruits are possible.
Case: A 4-year-old boy, whose past medical history is positive for three urinary tract infections, presents with a blood pressure of 135/90 mm Hg. He is likely to exhibit which of the following symptoms or signs?
b. headache
Cryptoorchidism Risks
Risk of testicular malignancy not eliminated by orchiplexi
Whether the testes are brought into the scrotum or not, the sperm count can be reduced.
Torsion of the testis due to excessive mobility of the undescended testis. Orchiopexy helps to
eliminate this problem.
The incidence of UTI and epididymitis are not affected by the position of the testes.
The failure of the testes to develop, and their subsequent atrophy, can be detected by 6 months of age.
HUS Symptoms
Ischemic changes result in renal cortical necrosis and damage to other organs such as colon, liver, heart, brain, and adrenal.
Gastrointestinal bleeding and obstruction, ascites, and central nervous system findings such as somnolence, convulsions, and coma can occur.
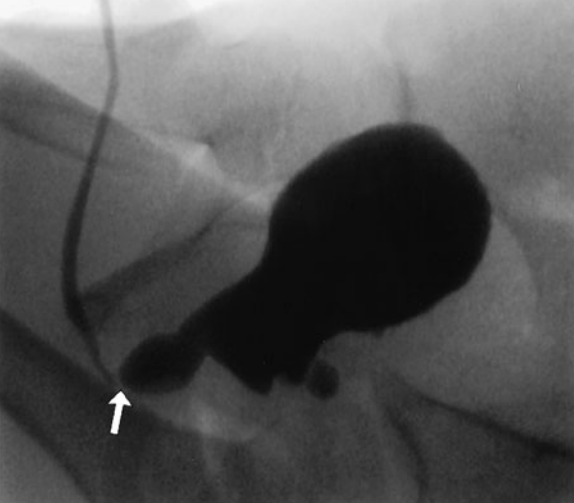
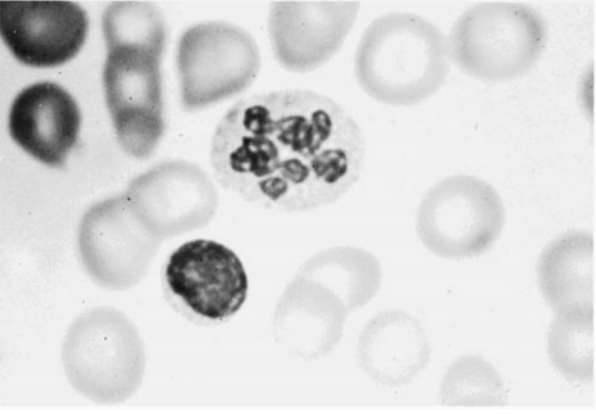
Lab: hemolyticuremic syndrome include low hemoglobin level, decreased platelet count, hypoalbuminemia, and evidence of hemolysis on peripheral smear (burr cells, helmet cells, schistocytes). Urinalysis reveals hematuria and proteinuria. A marked reduction of renal function leads to oliguria and rising levels of blood urea nitrogen (BUN) and creatinine.
Red Urine
A number of pH-dependent substances can impart a red color to urine. Use of phenolphthalein, a cathartic agent, or phenindione, an anticoagulant, can cause red urine; ingestion of blackberries, red Kool-Aid, or beets also can lead to red coloration (“beeturia”).
Vulvovaginitis
Symptoms: The discharge in nonspecific vulvovaginitis is usually brown or green and with a fetid odor. Burning with urination occurs because of contact between raw skin and urine.
Causes: tight-fitting clothing (including swimsuits or dance outfits), nylon undergarments, prolonged bubble baths with contamination of the vagina with soap products, use of perfumed lotions in the vaginal area, or improper toilet habits (wiping of fecal material toward rather than away from vagina).
Treatment: Mothers should be counseled to use only cotton underwear for young children, stop bubble baths (or at least splash fresh, clean water in the vaginal area at the end of a bath), and reemphasize wiping front to back after urination or bowel movements.
Foreign Body
A vaginal examination under general anesthesia is usually required when a vaginal foreign body is suspected. ## Varicocele pically, this condition is not painful but can become tender with strenuous exercise..  ## Torsion
emergent surgical consult
A Doppler flow study of testes or a radionuclide scan might be indicated if the area were painful and the diagnosis of a torsion were being entertained.
Hydrocele
Small hydroceles usually resolve spontaneously in the first year of life. Larger ones or those that have a variable fluid level with time will likely need surgical repair.
Nocturnal Enuresis
Involuntary voiding at night at an age when control of micturition is expected. Demographics: The condition is more common in boys than in girls.
Normal: By 5 years of age, most children (90%-95%) are completely dry during the day, and 80% to 85% are dry during the night.
Primary nocturnal enuresis: when the child has never been dry at night
Secondary: when the child has had a few months of dry nights before developing enuresis.
Cause: In most cases, no etiology is found. A family history is common.
Labs: Minimal laboratory testing beyond screening urinalysis is indicated.
Treatment: Desmopressin is not a cure, and episodes frequently return when the medication is stopped. Spontaneous cure rates are high regardless of therapy. Therapy is aimed at reassurance to the parents that the condition is self-limited, avoidance of punitive measures, and consideration of purchasing a bed-wetting alarm.
Idiopathic Hypercalciuria
Recurrent gross hematuria, persistent microscopic hematuria, and complaints of dysuria or abdominal pain (burning on urination) without initial stone formation. Over time, however, stones may form in 15% of cases.,
Albumin Diuretics Combo
Hypertension commonly accompanies glomerulonephritis, but only occasionally accompanies nephrotic syndrome. Diuretics are sometimes used in both nephrotic syndrome and glomerulonephritis with temporary effect, but are not curative. A combination of albumin infusions followed by a diuretic also has been used to temporarily decrease the edema in patients with nephrotic syndrome.
Bartter Syndrome
labs: hypokalemia, hypercalciuria, alkalosis, hyperaldosteronism, and hyperreninemia; blood pressure is usually normal.
Symptoms: Clinical presentations occurring frequently between 6 and 12 months of age include failure to thrive with constipation, weakness, vomiting, polyuria, and polydipsia.
Treatment is aimed at preventing dehydration, providing nutritional support, and returning the potassium level to normal.,
Hematology
Two weeks after a viral syndrome, a 2-year-old child develops bruising and generalized petechiae, more prominent over the legs. No hepatosplenomegaly or lymph node enlargement is noted. The examination is otherwise unremarkable. Laboratory testing shows the patient to have a normal hemoglobin, hematocrit, and white blood cell (WBC) count and differential. The platelet count is 15,000/μL. Which of the following is the most likely diagnosis?
ITP
Iron vs. Lead Toxicity
An 11-month-old African American boy has a hematocrit of 24% on a screening laboratory done at his well-child checkup. Further testing demonstrates: hemoglobin 7.8 g/dL; hematocrit 22.9%; leukocyte count 12,200/μL with 39% neutrophils, 6% bands, 55% lymphocytes; hypochromia on smear; free erythrocyte protoporphyrin (FEP) 114 μg/dL; lead level 6 μg/dL whole blood; platelet count 175,000/μL; reticulocyte count 0.2%; sickle-cell preparation negative; stool guaiac-negative; and mean corpuscular volume (MCV) 64 fL. Which of the following is the most appropriate recommendation?
When the iron available for production of hemoglobin is limited, free protoporphyrins accumulate in the blood. Levels of erythrocyte protoporphyrin (EP) are also elevated in lead poisoning. Iron-deficiency anemia can be differentiated from lead intoxication by measuring blood lead, which should be less than 10 μg/dL.
TEC, Transient erythroblastopenia
The parents of a previously healthy 2-year-old child note her to be pale and bring her to your clinic for evaluation. She currently has no fever, nausea, emesis, bone pain, or other complaints. Her examination is significant for pallor, tachycardia, and a systolic ejection murmur, but she has no organomegaly. Her complete blood count (CBC) reveals a hemoglobin of 4 g/dL, normal indices for age, a WBC count of 6.5/μL, and a platelet count of 750,000/μL. Her reticulocyte count is 0%. Coombs test is negative. Her peripheral blood smear shows no blast forms and no fragments. Red blood cell (RBC) adenosine deaminase levels are normal. A bone marrow reveals markedly decreased erythroid precursors. Which of the following is this child’s likely diagnosis?
Epidemiology: most common acquired RBC aplasia in children.
Demographics: This condition is commonly diagnosed between the ages of 1 to 3 years and some affected children have a history of a recent viral infection; however, no specific virus has been implicated (parvovirus B19 is usually specifically excluded).
Symptoms: Physical findings are minimal and include pallor and tachycardia.
Labs: Laboratory studies reveal a profound anemia and reticulocytopenia with a marked reduction in erythrocyte precursors in the marrow. RBC adenosine deaminase (ADA) levels are normal.
Treatment: The condition lasts for several months, and may require 1 or 2 transfusions, but ultimately is selflimited. Steroids are not helpful.,
Diamond-Blackfan
Demographics: Congenital and usually presents in infancy;
Labs: RBC ADA levels are usually elevated.
Associations: In addition, about half of patients will have congenital anomalies including short stature, cranial abnormalities, and upper extremity abnormalities.,
Pearson marrow-pancreas
is a mitochondrial disease characterized by sideroblastic anemia and exocrine pancreas dysfunction.
demographics: congenital
symptoms: including poor growth, pancreatic fibrosis with insulin-dependant diabetes, and muscle and nerve involvement. Early death is typical.,
On a routine-screening CBC, a 1-year-old is noted to have a microcytic anemia. A follow-up hemoglobin electrophoresis demonstrates an increased concentration of hemoglobin A2. The child is most likely to have which of the following?
B-thalassemia trait
A 4-year-old previously well African American boy is brought to the office by his aunt. She reports that he developed pallor, dark urine, and over the past few days. He stays with her, has not traveled, and has not been exposed to a jaundiced person, but he is taking trimethoprim sulfamethoxazole for otitis media. The CBC in the office shows a low hemoglobin and hematocrit, while his “stat” serum electrolytes, blood urea nitrogen (BUN), and chemistries are remarkable only for an elevation of his bilirubin levels. His aunt seems to recall his 8-year-old brother having had an “allergic reaction” to aspirin, which also caused a short-lived period of anemia and jaundice. Which of the following is the most likely cause of this patient’s symptoms?
Glucose-6-phosphate dehydrogenase deficiency
Your sister who lives in another state sends via e-mail photographs of her 6-month-old infant. You note the child has a white reflection from one of his eyes. You hastily assist in arranging an urgent pediatric ophthalmologic evaluation. Your sister immediately accesses the Internet and begins to ask questions of you. Which of the following statements found by your sister is correct?
With early detection, more than 90% of cases can be cured
Fetomaternal Transfusion
The absence of a major blood group incompatibility and the finding of a normal reticulocyte count argue strongly in favor of a recent fetomaternal transfusion, probably at the time of delivery. A Kleihauer-Betke stain for fetal hemoglobin-containing RBCs in the mother’s blood would confirm the diagnosis.
Fetomaternal tranfusion: the loss of fetal blood cells into the maternal circulation
Case: A 2950-g (6.5-lb) black baby boy is born at home at term. On arrival at the hospital, he appears pale, but the physical examination is otherwise normal. Laboratory studies reveal the following: mother’s blood type A, Rh-positive; baby’s blood type O, Rh-positive; hematocrit 38%; and reticulocyte count 5%. Which of the following is the most likely cause of the anemia?
Physiologic anemia of infancy
After birth, erythropoiesis ceases, and the progressive decline in hemoglobin values, reaching a nadir at 6 to 8 weeks of age, has been termed physiologic anemia of infancy.
Iron-deficiency anemia can be seen in the term infant between 9 and 24 months of age when the iron stores derived from circulating hemoglobin have been exhausted and an exogenous dietary source of iron has not been provided. The manifestations of sickle-cell disease do not appear until 4 to 6 months of life, coincident with the replacement of fetal hemoglobin with sickle hemoglobin.
A father brings his 3-year-old daughter to the emergency center after noting her to be pale and tired and with a subjective fever for several days. Her past history is significant for an upper respiratory infection 4 weeks prior, but she had been otherwise healthy. The father denies emesis or diarrhea, but does report his daughter has had leg pain over the previous week, waking her from sleep. He also reports that she has been bleeding from her gums after brushing her teeth. Examination reveals a listless pale child. She has diffuse lymphadenopathy with splenomegaly but no hepatomegaly. She has a few petechiae scattered across her face and abdomen and is mildly tender over her shins, but does not have associated erythema or joint swelling. A CBC reveals a leukocyte count of 8,000/μL with a hemoglobin of 4 g/dL and a platelet count of 7,000/μL. The automated differential reports an elevated number of atypical lymphocytes. Which of the following diagnostic studies is the most appropriate next step in the management of this child?
Leukemia, bone marrow biopsy
While bathing her newly-received 2-year-old son, a foster mother feels a mass in his abdomen. A thorough medical evaluation of the child reveals aniridia, hypospadias, horseshoe kidney, and hemihypertrophy. Which of the following is the most likely diagnosis for this child?
Wilms
Neuroblastoma should be considered in the differential diagnosis of abdominal mass, especially if fever, irritability, bone pain, limp, and diarrhea are present
A healthy 1-year-old child comes to your office for a routine checkup and for immunizations. His parents have no complaints or concerns. The next day, the CBC you performed as customary screening for anemia returns with the percentage of eosinophils on the differential to be 30%. Which of the following is the most likely explanation?
Helminth infestation
A 2-year-old child in shock has multiple nonblanching purple lesions of various sizes scattered about on the trunk and extremities; petechiae are noted, and oozing from the venipuncture site has been observed. The child’s peripheral blood smear is shown below. Clotting studies are likely to show which of the following?
DIC
A male infant was found to be jaundiced 12 hours after birth. At 36 hours of age, his serum bilirubin was 18 mg/dL, hemoglobin concentration was 12.5 g/dL, and reticulocyte count 9%. Many nucleated RBCs and some spherocytes were seen in the peripheral blood smear. The differential diagnosis should include which of the following?
b. hereditary sphereocytosis
On a routine well-child examination, a 1-year-old boy is noted to be pale. He is in the 75th percentile for weight and the 25th percentile for length. Results of physical examination are otherwise normal. His hematocrit is 24%. The answer to which of the following questions is most likely to be helpful in making a diagnosis?
on-deficiency anemia..
A 10-year-old boy is admitted to the hospital because of bleeding. Pertinent laboratory findings include a platelet count of 50,000/μL, prothrombin time (PT) of 15 seconds (control 11.5 seconds), activated partial thromboplastin time (aPTT) of 51 seconds (control 36 seconds), thrombin time (TT) of 13.7 seconds (control 10.5 seconds), and factor VIII level of 14% (normal 38%-178%). Which of the following is the most likely cause of his bleeding?
c. DIC
A 17-year-old adolescent comes to your office seeking help for “heavy” menses. Your review of systems also reveals weekly epistaxis. Her only significant past history includes a tonsillectomy at age 6 after which she required blood transfusion for excessive bleeding. Her family history includes several people who seem to bleed and bruise more easily than others. The patient’s mother required a hysterectomy after child birth for excessive hemorrhage. You order a variety of laboratory tests. The patient has a hemoglobin of 6.5 mg/dL with an MCV of 60%; her platelet count is 350,000/μL. Her von Willebrand antigen and her von Willebrand factor (vWF) activity (ristocetin cofactor activity) are decreased. Her vWF is reported as normal but in decreased amounts. You have been unable to reach her to report the findings, but when she calls about 1 week later she reports she is having a mild to moderate nosebleed. You initiate therapy with which of the following?
d. DDAVP
Osteosarcoma
Demographics: Occurs most commonly in the second decade of life, and a bit more commonly in boys than in girls. It occurs in all ethnic groups (in contrast, Ewing sarcoma, another bone malignancy, rarely occurs in blacks).
Symptoms: The lesion is found in the metaphyses of long bones, and usually presents with local pain and swelling.
Labs: Radiograph shows the expected “sunburst” pattern of bone formation.
Risks: Predisposing factors include a history of retinoblastoma, Li-Fraumeni syndrome, Paget disease, or radiotherapy. Any bone or joint “injury” not responding with conservative therapy within a short period of time should be evaluated.,
Osteo: 
Ewing: 

Over the previous 2 to 3 weeks, a very active 13-year-old white boy is noted by his family to have developed deep pains in his leg that awaken him from sleep. The family brings him to your office with a complaint of a swelling over his distal leg, which he attributes to his being kicked while playing soccer about 1 week ago. He has had no fever, headaches, weakness, bruising, or other symptoms. A radiograph of the leg is shown below. Which of the following is the most likely explanation for his pain?
Growing Pain
Demographics: Commonly seen in the school-age child.
Symptoms: They present with deep, aching pain, usually in the muscles of the leg. They are most common in the evening, gone by the morning, and do not cause joint swelling, redness, heat, or systemic signs or symptoms.,
Pathogenesis: The etiology is unknown, but, despite the name, it is not related to growing.
Hodgkin
Demographics: Children under 10 years of age; however, in developed countries, the peak incidence occurs in late adolescence and young adulthood.
Symptoms: Systemic symptoms include fever, night sweats, malaise, weight loss, and pruritus.
First step: Although a biopsy of the node may prove to be necessary at some point, the first step would involve a radiograph, which may show mediastinal mass suspicious for the disease. Depending on the results of the radiograph, a biopsy of a node may be indicated.,
Case: An otherwise healthy 17-year-old complains of swollen glands in his neck and groin for the past 6 months and an increasing cough over the previous 2 weeks. He also reports some fevers, especially at night, and possibly some weight loss. On examination, you notice that he has nontender cervical, supraclavicular, axillary, and inguinal nodes, no hepatosplenomegaly, and otherwise looks to be fairly healthy. Which of the following would be the appropriate next step?
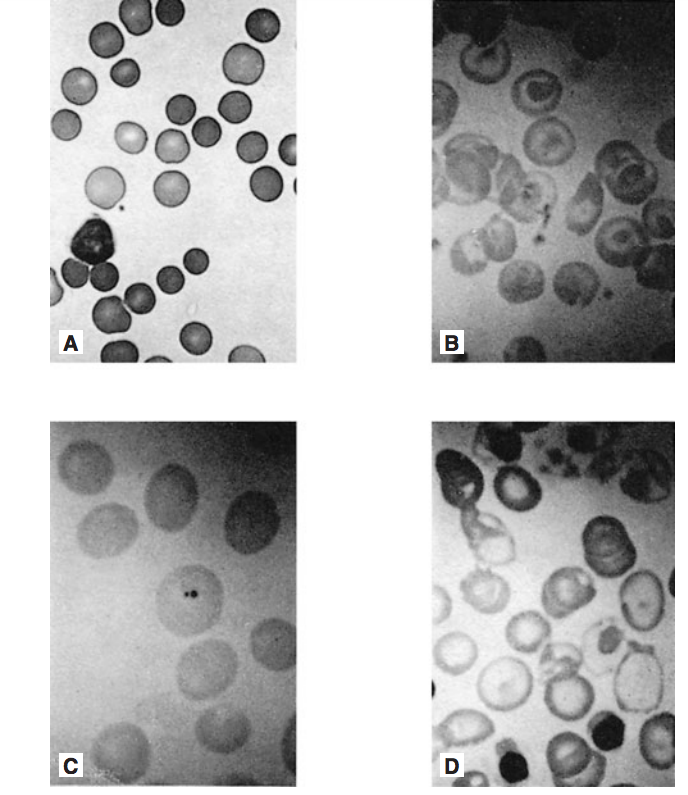
An otherwise healthy child has on his 1-year-old routine CBC the polymorphonuclear neutrophil shown below. This child likely has which of the following?
c. Folic acid deficiency
Sickle Cell Anemia
An 8-year-old patient with sickle-cell anemia
C. Howell-Jolly bodies
Target Cell
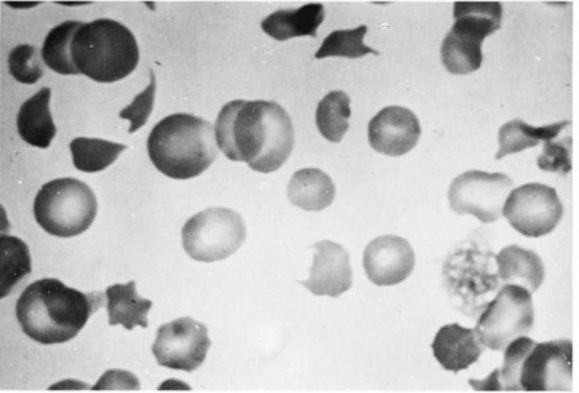
A 7-month-old boy with severe anemia requiring transfusions, heart failure, hepatosplenomegaly, and weakness.
D. A target cell is an erythrocyte with a membrane that is too large for its hemoglobin content; a thin rim of hemoglobin at the cell’s periphery and a small disk in the center give the cell a target-like appearance.
seen in children who have α-thalassemia, hemoglobin C disease, or liver disease (eg, obstructive jaundice or cirrhosis).
Hereditary Sphereocytosis
A 3-day-old newborn with anemia and pathologic hyperbilirubinemia requiring phototherapy
A. Uniformly small microspherocyte (less than 6 μm in diameter) are typical of hereditary spherocytosis (slide A). Because of a decreased surface to volume ratio, these osmotically fragile RBCs have an increased density of hemoglobin. Although spherical RBCs also can appear in other hemolytic states (eg, immune hemolytic anemia, microangiography, ABO incompatibility, and hypersplenism), their cellular volume is only irregularly augmented. Patients with hereditary spherocytosis can present in the newborn period with anemia, hyperbilirubinemia, and reticulocytosis. They may remain asymptomatic until adulthood, when they develop symptoms. After infancy, hepatosplenomegaly and gallstones are common.
HB C
A completely asymptomatic, healthy 1-year-old whose routine CBC reveals an abnormality
B. Although hemoglobin C disease (slide B) is frequently a mild disorder, target cells constitute a far greater percentage of total RBCs than in thalassemia major. In the heterozygous state, no anemia or disease is noted, but target cells are seen. In the homozygous state, a moderately severe hemolytic anemia, reticulocytosis, and splenomegaly are seen, along with a smear containing a large number of target cells.
Last updated