OB Uworld
Colposcopy
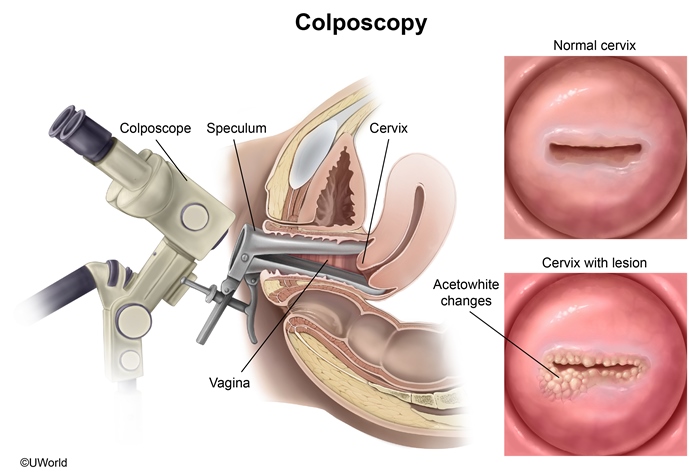
A Pap test is a screening examination for precancerous lesions of the uterine cervix. High-grade squamous intraepithelial lesions (HSILs) on Pap testing are concerning for underlying severe neoplasia (eg, CIN2, CIN3) or invasive cervical cancer, and all patients require evaluation with immediate colposcopy. Repeat Pap testing is not appropriate.
Colposcopy evaluates the cervix and vagina under magnification after application of acetic acid to contrast and identify abnormal (eg, aceto-white changes) from normal cells; abnormal vessels (a sign of high-grade lesions) also become more visible. Cervical neoplasia typically occurs at the transformation zone or squamocolumnar junction. If these areas are not visualized during colposcopy (eg, an "inadequate" colposcopy), an endocervical curettage is performed to evaluate the endocervical canal. Endocervical curettage is an invasive procedure and is deferred during pregnancy due to risk of miscarriage and preterm delivery. Cervical biopsy is performed even in pregnancy if a lesion has high-grade features (eg, abnormal vessels).
Kleihauer-Betke
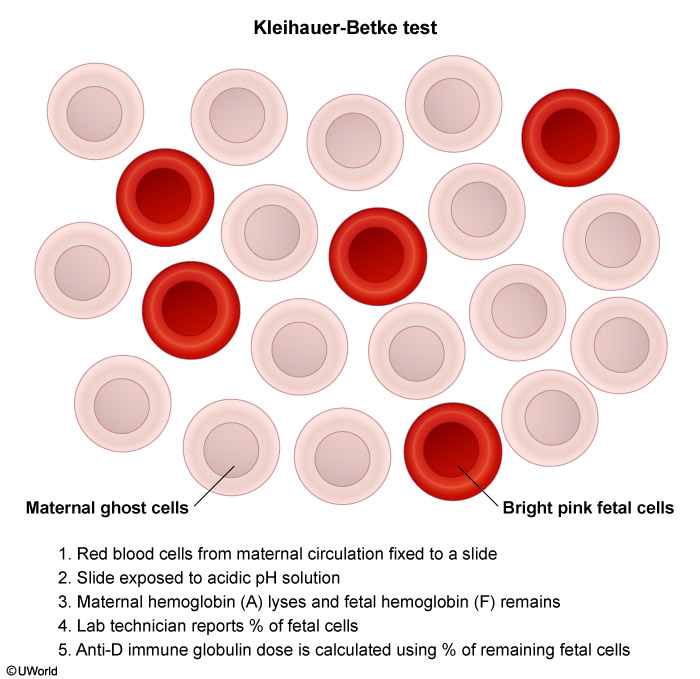
The Kleihauer-Betke (KB) test is commonly used to determine the dose. Red blood cells from the maternal circulation are fixed on a slide. The slide is exposed to an acidic solution and adult hemoglobin lyses, leaving "ghost" cells. The dose of anti-D immune globulin is calculated from the percentage of remaining fetal hemoglobin.
A standard dose of 300 µg at 28 weeks gestation can usually prevent alloimmunization. However, 50% of Rh-negative women will need a higher dose after delivery, placental abruption, or procedures.
Neonatal Thyrotoxicosis
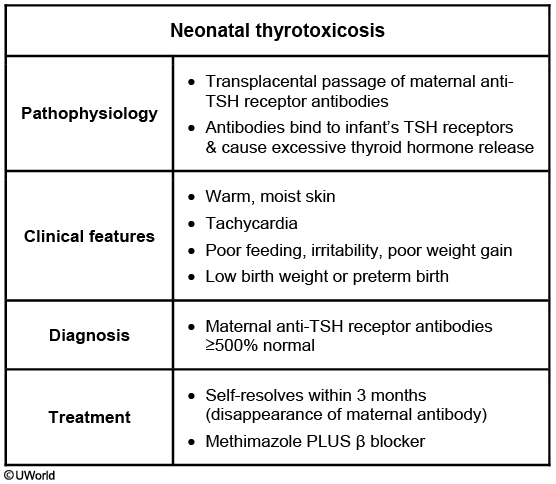
This neonate's presentation (maternal history of Graves' disease, low birth weight, tachycardia, warm skin, irritability) is characteristic of neonatal thyrotoxicosis (neonatal Graves' disease). Thyrotoxicosis results from transplacental passage of anti-TSH receptor antibodies during the third trimester. Elevated anti-TSH receptor antibody levels can occur despite maternal treatment for Graves' disease and euthyroidism or hypothyroidism during pregnancy. Neonates born to women with anti-TSH receptor antibodies >5 times the upper limit of normal are at greatest risk.
Most infants with thyrotoxicosis are born to mothers known to have Graves' disease. The most severe cases of thyrotoxicosis result in symptomatic fetuses (fetal tachycardia, hydrops, growth restriction.) Symptomatic patients require short-term treatment with methimazole plus a β blocker as neonatal hyperthyroidism has adverse effects on the developing nervous system (eg, growth retardation, developmental/behavioral problems). The condition generally self-resolves over the first few weeks to months of life as maternal antibody disappears from the infant's circulation.
Placenta Previa
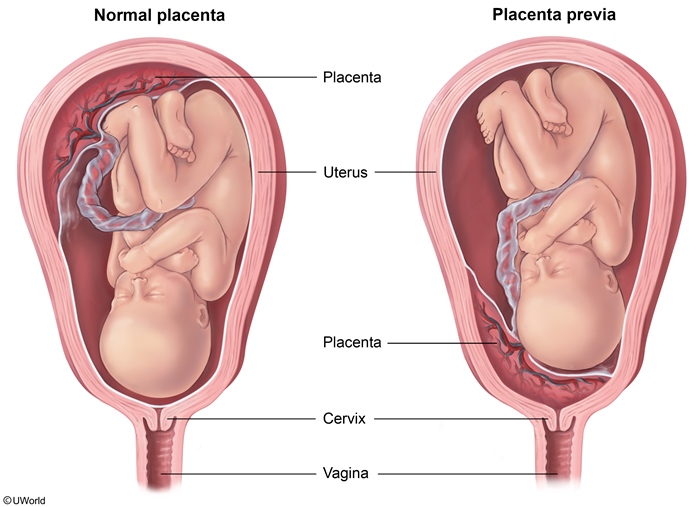
This patient's ultrasound is consistent with placenta previa, which occurs when the placenta implants over the internal cervical os. Risk factors for placenta previa include multiparity and advanced maternal age (>35). Patients with this condition are at risk for antepartum bleeding, which is typically painless and occurs with or without contractions on the tocodynamometer.
Placenta previa is usually diagnosed during a routine antenatal ultrasound. Pelvic rest is recommended for the duration of the pregnancy as intercourse can cause contractions, which in turn can lead to bleeding (as seen in this patient) by shearing the placenta off the cervix and lower uterine segment.
No digital cervical exam, no intercourse
Patients diagnosed antenatally undergo cesarean delivery at 36-37 weeks (late preterm/early term) to avoid risks associated with labor and to minimize prematurity complications.
Although this patient has stable vital signs and a normal fetal heart rate tracing, cesarean delivery should be performed urgently given the patient's vaginal bleeding at 37 weeks in the setting of placenta previa. Labor and expectant management are contraindicated due to the risk of hemorrhage. Vaginal delivery would require the placenta to detach and deliver before the fetus, which would deprive the fetus of oxygen.
Placenta previa
Risk factors
Prior placenta previa Prior cesarean delivery Multiple gestation
Clinicalfeatures
Painless vaginal bleeding >20 weeks gestation
Diagnosis
Transabdominal followed by transvaginal sonogram
Management
No intercourse No digital cervical examination Inpatient admission for bleeding episodes
Mg toxicity

Magnesium sulfate is the treatment of choice for the prevention of eclamptic seizures. It is also administered to patients for whom preterm delivery is imminent as it decreases the risk for cerebral palsy in premature infants. Common adverse effects of magnesium sulfate include headache, nausea, fatigue, and diaphoresis. Signs of magnesium toxicity include loss of deep tendon reflexes, somnolence, and respiratory depression.
Because magnesium is solely excreted by the kidneys, a common risk factor for magnesium toxicity is renal insufficiency, as seen in this patient. Patients with an elevated serum creatinine may need a lower magnesium dose and close observation. Magnesium levels should be checked after initiation of the infusion and the infusion rate adjusted accordingly. Calcium gluconate is the first-line treatment for magnesium toxicity.
Concomitant use of calcium channel blockers (eg, nifedipine) and magnesium can potentiate hypotension. This patient is hypertensive.
AFP
Maternal serum alpha-fetoprotein screening
↑ MSAFP
↓ MSAFP
Open neural tube defects (eg, anencephaly, open spina bifida) Ventral wall defects (eg, omphalocele, gastroschisis) Multiple gestation Fetal demise Hepatocellular carcinoma Yolk sac tumor
Aneuploidies (eg, trisomy 18 & 21)
MSAFP = maternal serum alpha-fetoprotein.
Alpha-fetoprotein (AFP) is a major protein produced by the fetal yolk sac, liver, and gastrointestinal tract. Maternal serum AFP (MSAFP) is measured at 15-20 weeks gestation (optimally at 16-18 weeks) to screen for fetal anomalies. MSAFP is used primarily to screen for open neural tube defects. Increased levels are also associated with fetal abdominal wall defects (eg, gastroschisis, omphalocele) and multiple gestation. Less commonly, an increased MSAFP can be seen in fetal congenital nephrosis and benign obstructive uropathy.
An elevated MSAFP warrants careful ultrasound evaluation of the fetal anatomy. In addition, the number of fetuses should be clarified as multiple gestations produce more AFP. Gestational age is also confirmed as interpretation of AFP level depends on an accurate gestational age.
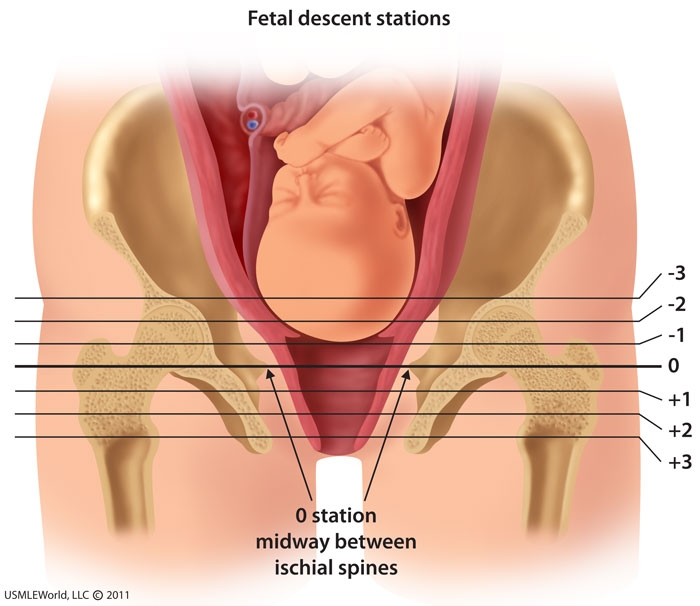
Endometriosis
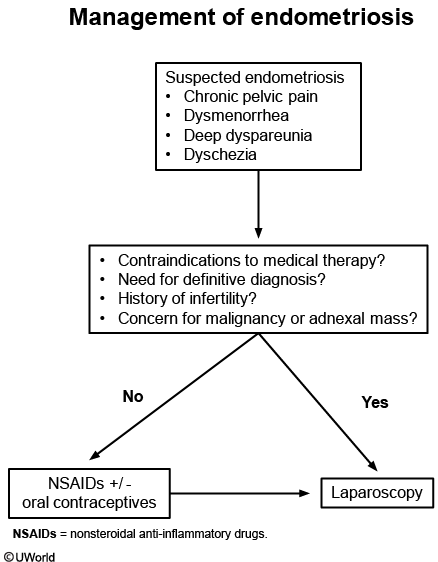
Endometriosis is an estrogen-dependent condition that affects reproductive-age women. Ectopic endometrial glands and stroma cause pain due to cyclic hemorrhage and accumulating fibrosis. Patients can be asymptomatic or develop dysmenorrhea, dyspareunia, and chronic pelvic pain that worsens before the onset of menses. Typical examination findings are tenderness of the recto-vaginal area, tenderness with movement of the uterus, and thickening of the uterosacral ligaments caused by endometrial implants on the recto-vaginal septum, pelvic peritoneum, anterior and posterior cul-de-sac, and uterosacral ligaments. Negative laboratory testing and normal ultrasound exclude other etiologies of chronic pelvic pain.
Treatment with nonsteroidal anti-inflammatory drugs and/or oral contraceptives can be initiated empirically in patients with suspected endometriosis. Laparoscopy is indicated after failure of empiric therapy, as in this patient. Laparoscopy allows for direct visualization, biopsy, and removal of endometriotic lesions. Unless estrogenic stimulation is suppressed, symptoms eventually return with the regrowth of endometriosis. Definitive treatment in women who have completed childbearing is with hysterectomy and oophorectomy.
Infertility is commonly the sole presenting symptom of endometriosis, which is present in one quarter of all patients with infertility. Cyclic accumulation of ectopic foci of hemorrhage and adhesions can distort pelvic anatomy and impair fertility by obstructing oocyte release or sperm entry. The presence of an endometrioma (ovarian endometriosis cyst) is also associated with impaired ovarian function. Laparoscopic resection of endometriosis, especially ovarian endometriomas, improves conception rates.
Cervical Mucous
Cervical mucus secretion close to ovulation (late follicular phase) increases in quantity and can be perceived by patients as vaginal discharge. This mucus is clear, elastic, thin in consistency, and described similar in appearance to an uncooked egg white. It is thought to facilitate sperm transport into the uterus for conception. After ovulation occurs, the mucus becomes thick and less hospitable to sperm.
A cervical mucus plug serves as barrier to ascending infection during pregnancy. This brown, red, or yellowish thick mucus is typically shed before or during labor.
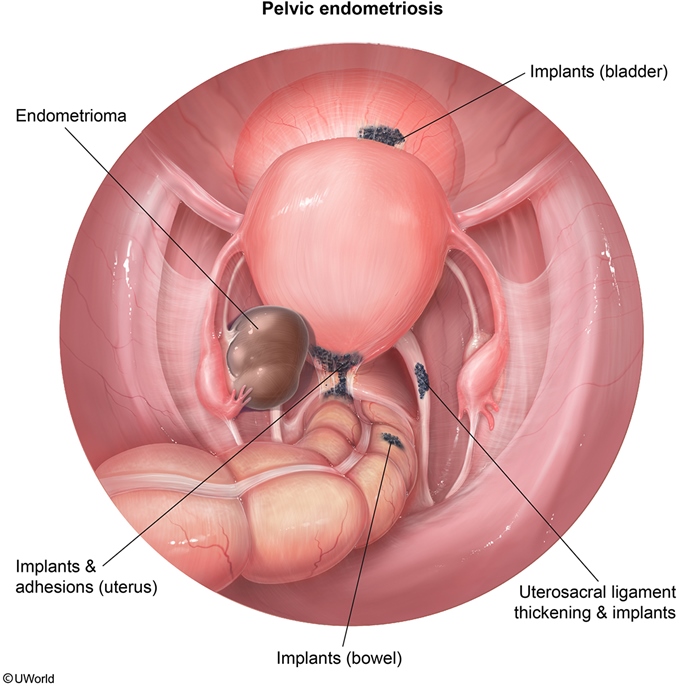
HELLP
This patient's clinical features are most consistent with HELLP syndrome (Hemolysis, Elevated Liver enzymes, Low Platelet count). HELLP syndrome may be a variation of severe preeclampsia and affects 10%–20% of women with preeclampsia. Serious liver problems include centrilobular necrosis, hematoma formation, and thrombi in the portal capillary system. These processes can cause liver swelling with distension of the hepatic (Glisson's) capsule, resulting in right upper quadrant or epigastric pain. The diagnosis is based on clinical presentation and laboratory findings (Table). This patient is hypertensive and has signs of hemolysis (anemia with indirect hyperbilirubinemia), elevated hepatic transaminases, and thrombocytopenia. Alkaline phosphatase is normally elevated in pregnancy.
This patient's sudden-onset dyspnea, hypoxia, and crackles are most likely due to acute pulmonary edema, a rare and life-threatening complication of severe preeclampsia. Preeclamptic patients have generalized arterial vasospasm leading to increased systemic vascular resistance and high cardiac afterload. The heart becomes hyperdynamic to try to overcome the systemic hypertension. Additional factors that may contribute to pulmonary edema include decreased renal function, decreased serum albumin, and endothelial damage leading to increased capillary permeability.
Management includes supplemental oxygen, fluid restriction, and diuresis in severe cases. Fluid restriction and diuresis must be used with caution as plasma volume is effectively decreased through third-spacing and placental perfusion can be compromised.
Second Stage of Labor
Second stage arrest of labor
Definition
Insufficient fetal descent after pushing for: >3 hours if nulliparous >2 hours if multiparous
Risk factors
Maternal obesity Excessive pregnancy weight gain Diabetes mellitus
Etiology
Cephalopelvic disproportion Malposition Inadequate contractions Maternal exhaustion
Management
Operative vaginal delivery Cesarean delivery
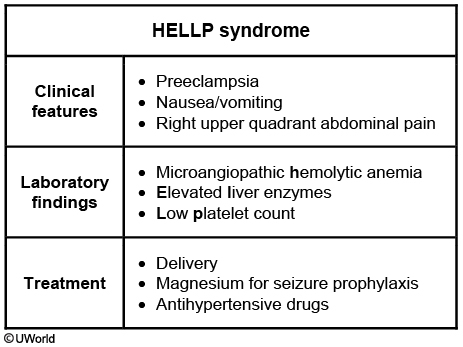
The second stage of labor begins when the cervix is 10 cm dilated and ends with fetal delivery. The duration of the second stage is affected by parity and use of neuraxial anesthesia. Progression during the second stage is evaluated by determining the fetal station, which measures the descent of the presenting part through the pelvis.
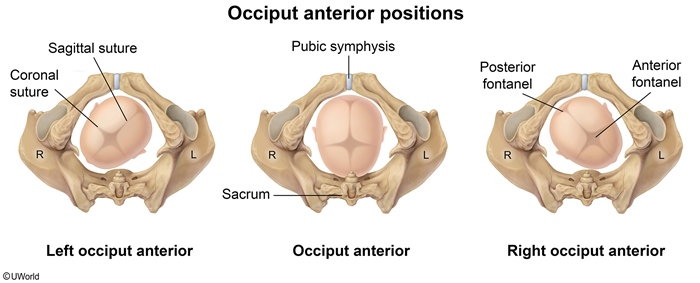
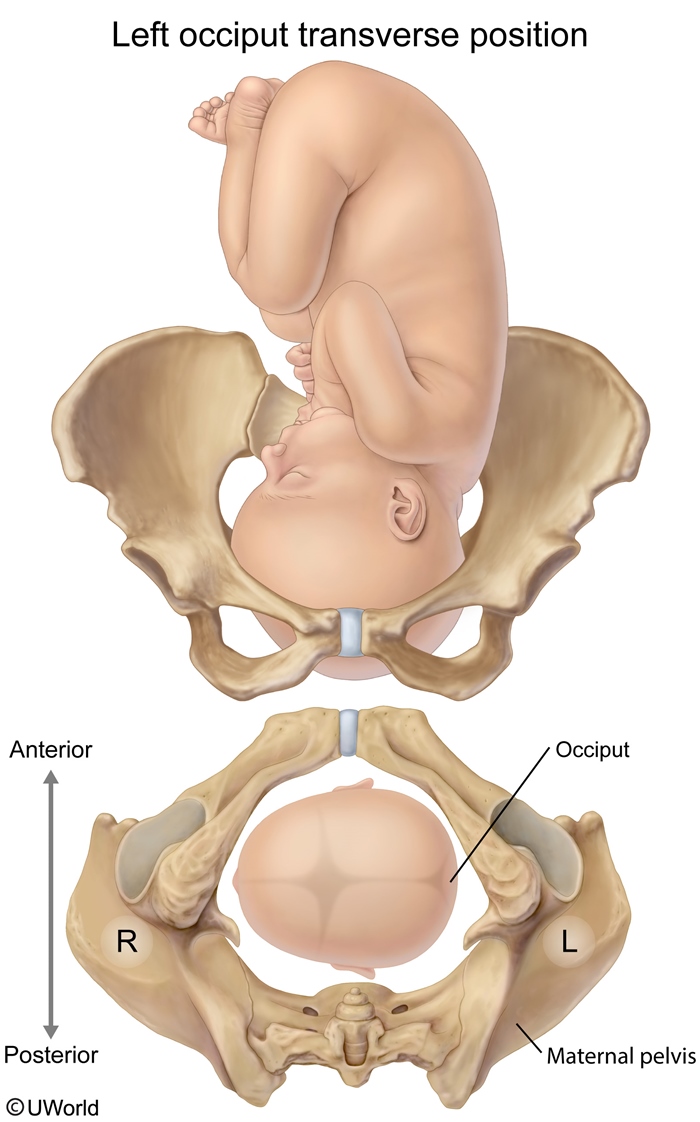
An arrested second stage occurs when there is no fetal descent after pushing for >3 hours in nulliparous patients or >2 hours in multiparous patients. The most common cause of a prolonged or arrested second stage is fetal malposition. The fetal position is the relationship of the fetal presenting part to the maternal pelvis. The optimal fetal position is occiput anterior as it facilitates the cardinal movements of labor. Deviations from this position (eg, occiput transverse, occiput posterior) can cause cephalopelvic disproportion and arrest of the second stage.
Breech
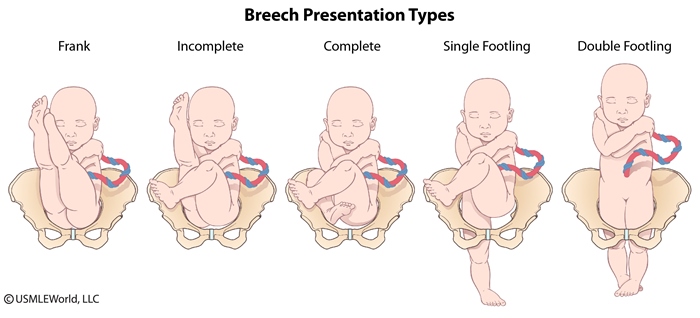
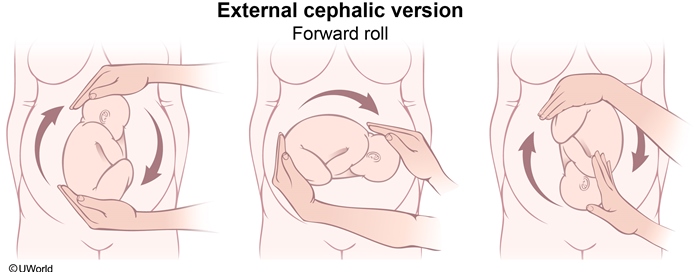
External cephalic version (ECV) involves maneuvers to convert a breech into a vertex presentation for delivery. It can be performed between 37 weeks gestation and the onset of labor and has been shown to reduce the rate of cesarean deliveries.
Fetal well-being must be documented by a nonstress test and there should be no contraindications to a vaginal delivery. As ECV has the potential to cause fetal distress, it should be performed only when arrangements have been made for a back-up emergency cesarean delivery. Contraindications to ECV include ruptured membranes, hyperextended fetal head, fetal/uterine abnormalities, and non-reassuring fetal monitoring (Table).
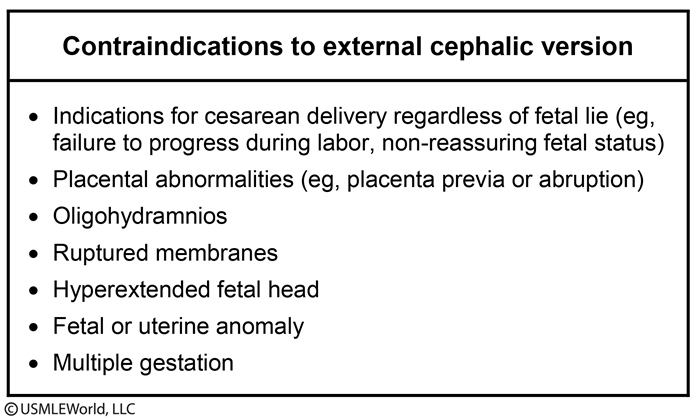
Cesarean delivery is indicated for breech presentations when vaginal delivery is not safe (eg, placental abnormalities, incomplete breech, estimated fetal weight >4 kg [8.8 lb]).
Internal Podalic Version
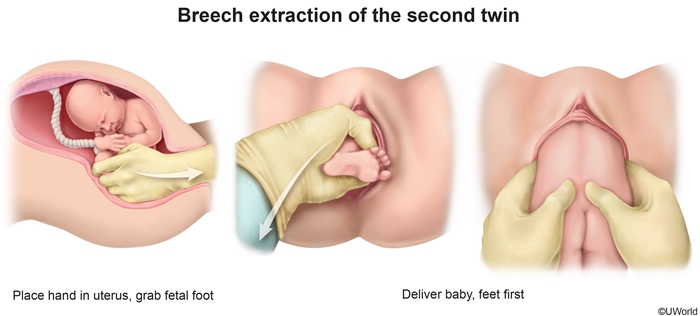
Internal podalic version is performed in twin delivery to convert the second twin from a transverse/oblique presentation to a breech presentation for subsequent delivery.
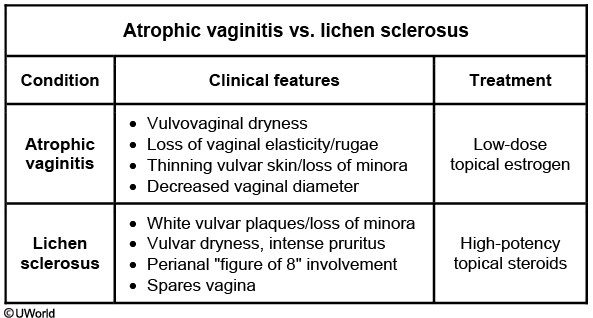
Hypoestrogenism
Vulvovaginal atrophy is also known as atrophic vaginitis and menopausal genitourinary syndrome due to estrogen deficiency. The bladder trigone, urethra, pelvic floor muscles, and endopelvic fascia possess estrogen receptors and are maintained by adequate estrogen levels. Hypoestrogenemia results in atrophy of the superficial and intermediate layers of the vagina and urethral mucosal epithelium. Diminished urethral closure pressure and loss of urethral compliance contribute to urgency, frequency, urinary tract infections, and incontinence (stress and urge).
This patient's urinary symptoms in the setting of vulvovaginal atrophy are consistent with either urgency incontinence or a recurrent urinary tract infection. A urinalysis and urine culture should be ordered to distinguish between these 2 conditions. Use of moisturizers and lubricants is the first step in management of mild atrophic vaginitis. For moderate to severe cases with predominant urinary symptoms, as in this patient, treatment is low-dose vaginal estrogen therapy.
Vesicovaginal Fistula
Lichen Sclerosis
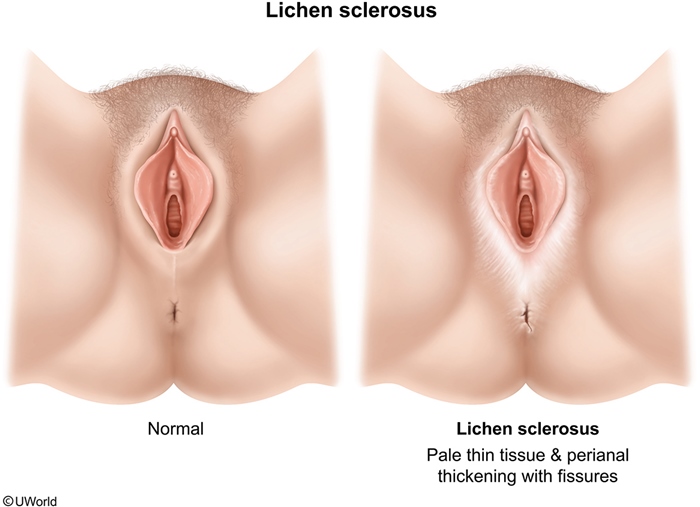
Lichen sclerosus (LS) is a chronic inflammatory condition of the anogenital region that can affect women at any age. This condition can have an autoimmune pathogenesis and often coexists with other autoimmune conditions (eg, type 1 diabetes mellitus, thyroid abnormalities). Extragenital involvement (eg, buttocks, lower back, abdomen, under breasts, shoulders, armpits) is also possible. The perianal skin may also be involved, resulting in a "figure of 8" appearance. Anogenital symptoms include intense pruritus, dyspareunia, dysuria, and painful defecation.
Physical examination reveals porcelain-white polygonal patches with atrophy (eg, regression, obliteration) of normal genital structures. The skin is classically described as "cigarette paper" quality (eg, thin, white, crinkled). Sclerosus and scarring lead to obliteration of the labia minora and clitoris and a decrease in the diameter of the introitus, all findings seen in this patient. Although the diagnosis can be made clinically, a punch biopsy is recommended for definitive diagnosis. LS is a vulvar premalignant lesion as vulvar squamous cell carcinoma (SCC) occurs with greater frequency in these patients. A vulvar punch biopsy can rule out vulvar malignancy.
Intraductal Papilloma
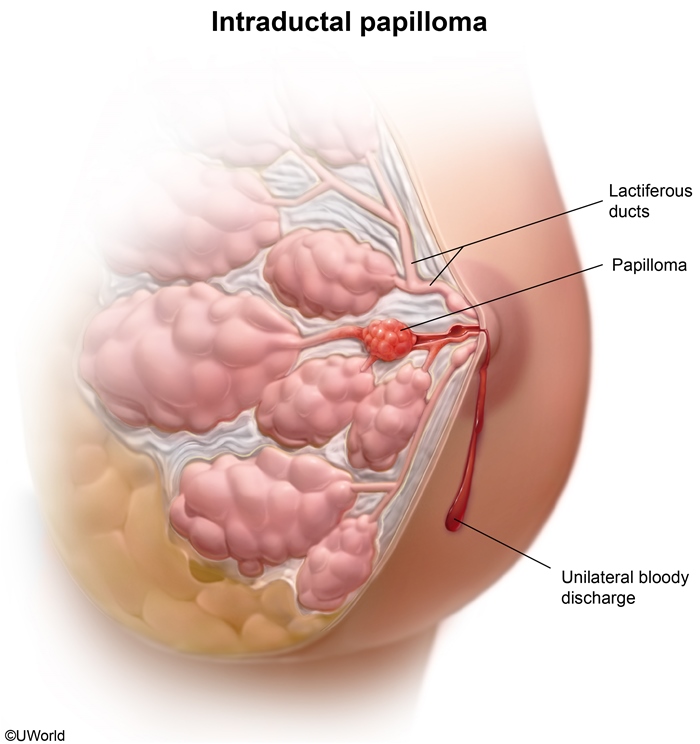
Imaging with breast mammography and ultrasound would reveal normal breast tissue or a single dilated breast duct. Confirmation of the diagnosis is with biopsy or duct excision and subsequent pathologic evaluation.
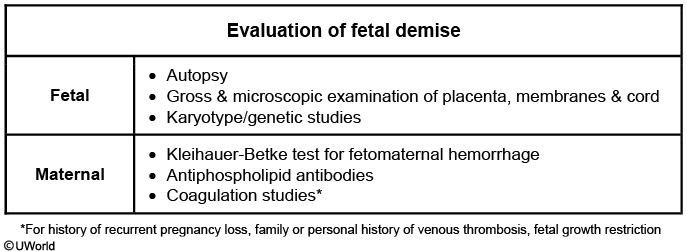
Prenatal Test
Prenatal testing
Test
Timing (weeks)
Advantages
Disadvantages
First-trimester combined test*
9-13
Early screening
Not diagnostic
Cell-free fetal DNA
≥10
High sensitivity & specificity for aneuploidy
Not diagnostic
Chorionic villus sampling
10-13
Definitive karyotypic diagnosis
Invasive; risk of spontaneous abortion
Second-trimester quadruple screen**
15-22
Screens for neural tube defects & aneuploidy
Not diagnostic
Amniocentesis
15-20
Definitive karyotypic diagnosis
Invasive; risk of membrane rupture, fetal injury & pregnancy loss
Second-trimester ultrasound
18-20
Measures fetal growth, evaluates fetal anatomy, confirms placenta position
Cannot identify all abnormalities; some findings are of uncertain significance
Pregnancy-associated plasma protein, β-hCG, nuchal translucency.*Maternal serum alpha-fetoprotein, estriol, β-hCG, inhibin A.
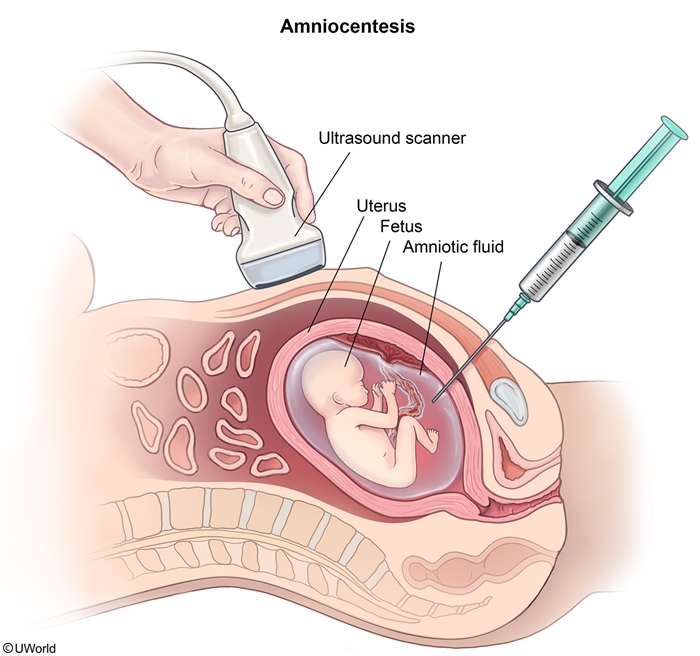
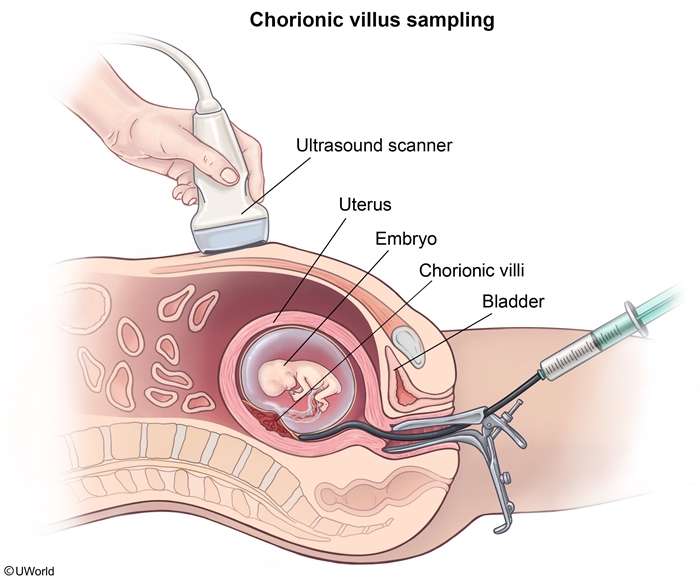
If the patient declines invasive testing, an anatomy ultrasound and cell-free fetal DNA test (which has a higher sensitivity and specificity than the first-trimester screen) can be used to further analyze the risk for fetal aneuploidy.
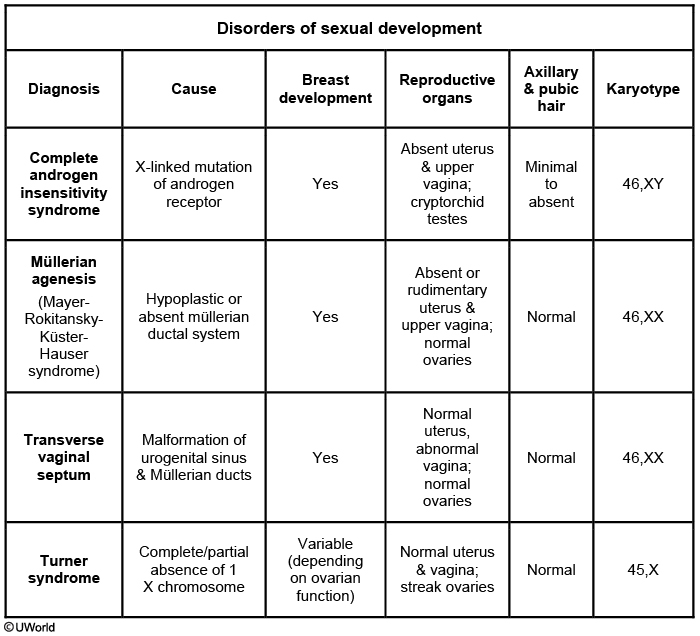
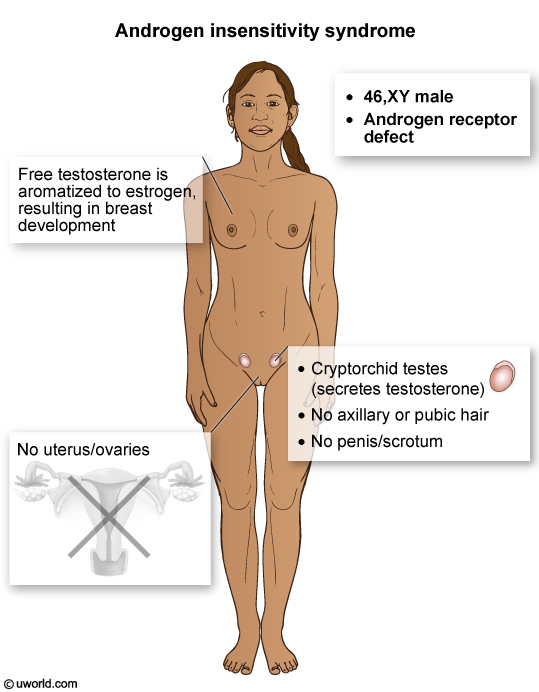
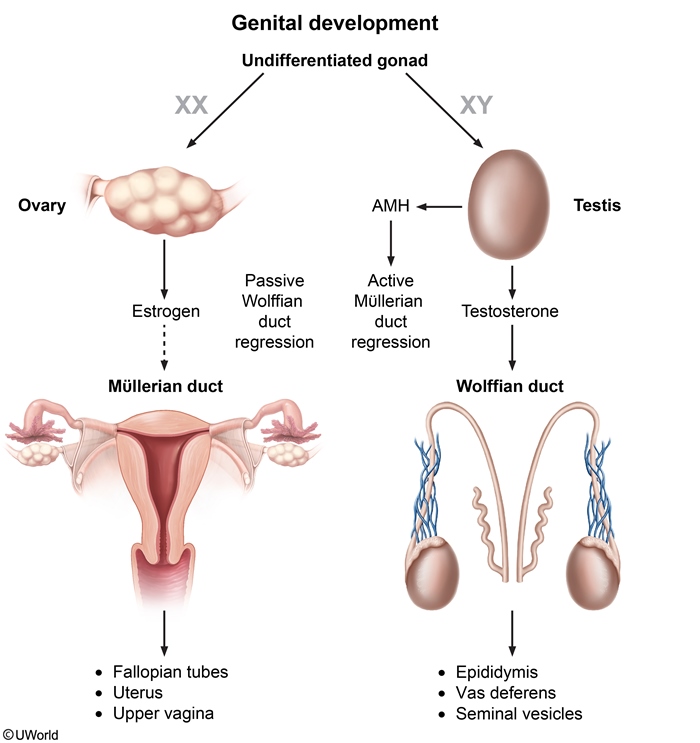
Sexual Disorder Differentiation
Gonococcal Pharyngitis
Pharyngitis with fever and lower abdominal pain in a young, sexually active patient is suggestive of gonococcal pharyngitis with pelvic inflammatory disease (PID). Neisseria gonorrhoeae is a common sexually transmitted infection that can cause cervicitis (eg, mucopurulent discharge, irregular bleeding) and lead to PID (eg, fever, lower abdominal pain). Gonococcal pharyngitis occurs due to inoculation of the pharynx during orogenital contact. Although pharyngeal involvement is typically asymptomatic, it may present with pharyngeal edema and nontender cervical lymphadenopathy, as seen in this patient. Diagnosis is confirmed by nucleic acid amplification testing for gonorrhea.
Postpartum vaccine
To decrease the risk of CRS, all women are tested for rubella immunity at the initial prenatal visit by measuring antirubella IgG antibody concentration. The MMR vaccine, a live-attenuated vaccine, is contraindicated during pregnancy due to a theoretical risk of CRS; however, it is safe for breastfeeding mothers. All rubella-nonimmune patients should be vaccinated during the immediate postpartum period.
Vaccines during Pregnancy
Vaccines during pregnancy
Recommended
Tdap Inactivated influenza Rho(D) immunoglobulin
Indicated for high-risk patients
Hepatitis B Hepatitis A Pneumococcus Haemophilus influenzae Meningococcus Varicella-zoster immunoglobulin
Contraindicated
HPV MMR Live attenuated influenza Varicella
Electrophoresis
Screening for hemoglobinopathies via hemoglobin electrophoresis during pregnancy is indicated for patients with anemia (hemoglobin <11 g/dL in pregnancy) and a mean corpuscular volume <80 fL.
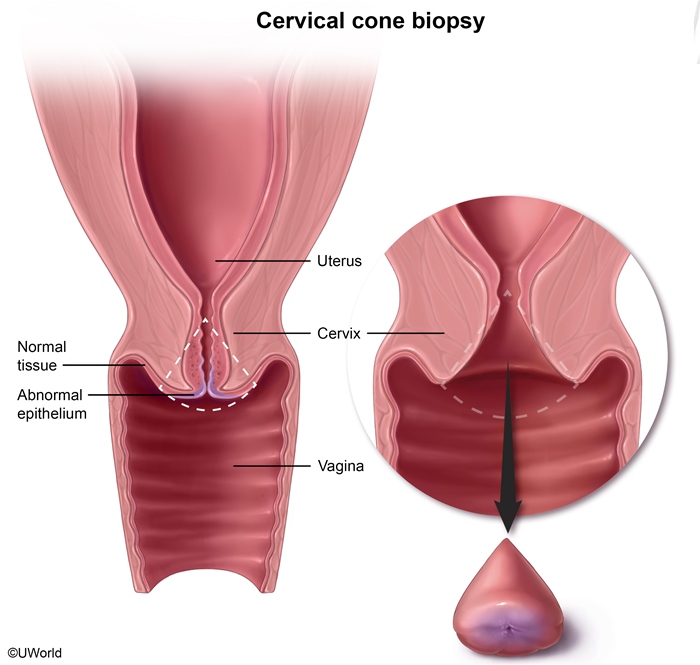
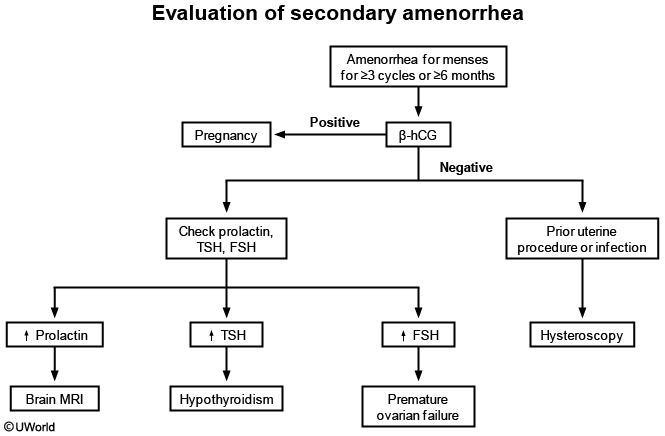
CIN 3
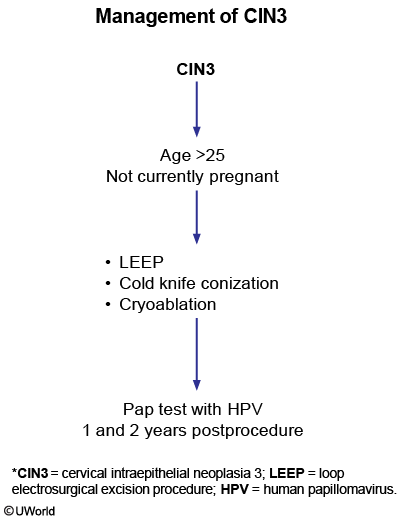
All nonpregnant patients age >25 with CIN3 require excision of the transformation zone (eg, cone biopsy) due to the high risk of progression to invasive squamous cell cervical carcinoma.
Cervical conization is both a diagnostic and therapeutic procedure, typically removing the entire lesion and allowing for examination of the full depth of invasion. Treatment for invasive carcinoma includes hysterectomy, radiation, and chemotherapy, depending on disease stage. If the specimen margins are clear of disease and no evidence of invasion is found, Pap testing with HPV co-testing in 1 and 2 years postprocedure is required.
HPV infection is the cause of the high-grade lesions on Pap tests; therefore, HPV co-testing is not performed.
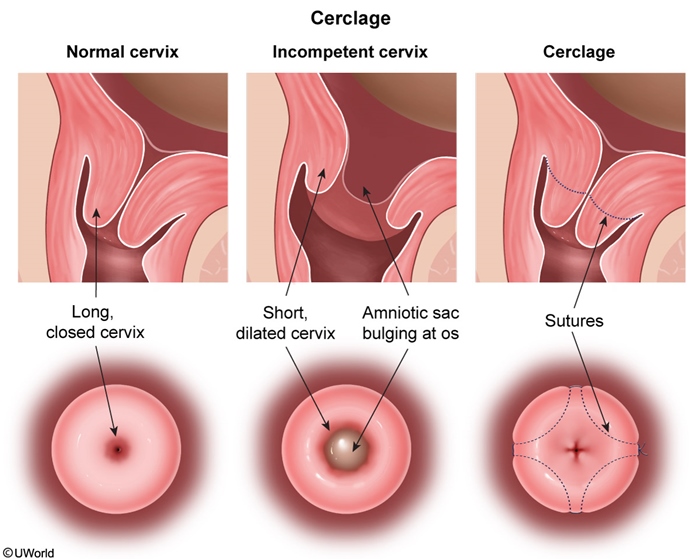
In particular, removal of part of the cervix by cold knife conization for cervical intraepithelial neoplasia can cause cervical scarring/stenosis and incompetence.
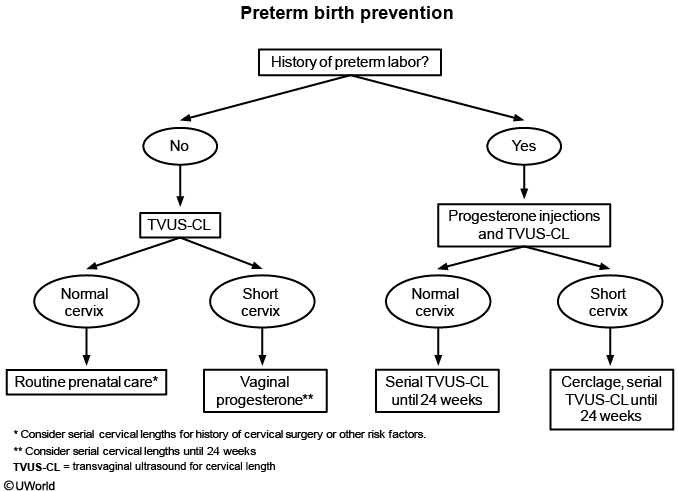
The first step in evaluating the risk of preterm labor is transvaginal ultrasound (TVUS) measurement of cervical length in the second trimester. A short cervical length is a strong predictor of preterm labor.
Human papillomavirus infection and tobacco use are important risk factors for cervical intraepithelial neoplasia (CIN) and squamous cell carcinoma (SCC). Colposcopy is the gold standard method of diagnosing CIN. CIN 3 is a premalignant cervical lesion at high risk of progressing to SCC, and cervical conization, excision of the intact transformation zone, is the recommended treatment. Cervical conization may be performed with a scalpel (cold knife conization) or via electrocautery, also known as a loop electrosurgical excision procedure (LEEP).
Cervical stenosis, an abnormal stricture of the cervical canal, is a potential complication of cervical conization due to scar tissue. Cervical stenosis may impede menstrual flow and cause secondary dysmenorrhea or amenorrhea. The obstruction of the cervical outlet may prevent sperm entry, resulting in impaired fertility.
Cervical conization carries additional risks, including cervical incompetence and preterm delivery due to weakened cervical stroma. These risks are related directly to the amount of cervical tissue removed.
Septic Thrombophlebitis
Septic pelvic thrombophlebitis
Risk factors
Cesarean delivery Pelvic surgery Endometritis Pelvic inflammatory disease Pregnancy Malignancy
Pathophysiology
Hypercoagulability Pelvic venous dilation Vascular traumaInfection
Presentation
Fever unresponsive to antibiotics No localizing signs/symptoms Negative infectious evaluation Diagnosis of exclusion
Treatment
Anticoagulation Broad-spectrum antibiotics
This patient's presentation is consistent with septic pelvic thrombophlebitis (SPT), a complication associated with either pelvic surgery or the postpartum period. SPT is a thrombosis of the deep pelvic or ovarian veins (as seen in this patient's bilateral lower quadrant tenderness) that becomes infected. Several factors predispose postpartum patients to thrombosis:
Hypercoagulable state of pregnancy
Pelvic venous stasis and dilation
Endothelial damage from infection and/or trauma during delivery
Because the most common etiology for puerperal fever is endometritis, patients are initially treated empirically with antibiotics. Persistent fever unresponsive to broad-spectrum antibiotic therapy and a negative infectious evaluation (eg, blood and urine cultures, urinalysis) suggest SPT, which is a diagnosis of exclusion. Risk factors include cesarean delivery and chorioamnionitis/endometritis. Treatment is with anticoagulation and broad-spectrum antibiotics.
Postpartum Hemorrhage
Postpartum hemorrhage (PPH) is an obstetrical emergency and a major cause of maternal mortality. Hemostasis after placental delivery is achieved by clotting and by compression of the placental site blood vessels by myometrial contraction. Disruption of either of these processes can lead to PPH.
Primary PPH occurs less than 24 hours after delivery and is most commonly caused by uterine atony. Atony occurs when the uterus becomes fatigued (eg, prolonged labor), fast delivery, over-distended (eg, fetal weight >4000 g [8.8 lb], multiple gestation), or unresponsive to oxytocin from oxytocin receptor saturation. Other risk factors for atony include operative (eg, forceps-assisted) vaginal delivery and hypertensive disorders. The uterus fails to contract and is soft ("boggy") and enlarged (eg, above the umbilicus) on physical examination.
Because ultrasound showed a thin endometrial stripe, suggesting an empty and normal uterine cavity, retained placenta is unlikely.
Other causes of PPH:
Retained placenta
Genital tract laceration
Uterine rupture
Coagulopathy
The management of postpartum hemorrhage (PPH) begins with assessment of vital signs, intravenous fluids to maintain systolic blood pressure, and often transfusion of appropriate blood products. Treatment also begins with bimanual massage and uterotonic medications. Bimanual massage involves one hand massaging the uterine fundus abdominally and the other hand compressing and massaging the uterus vaginally. The first-line uterotonic is oxytocin, which is generally administered via intravenous infusion.
If oxytocin and bimanual massage fail, the next step is to administer other uterotonic agents. Methylergonovine is an uterotonic drug that causes smooth muscle constriction, uterine contraction, and vasoconstriction. Because vasoconstriction can cause hypertension, a history of hypertension is a contraindication to methylergonovine. Carboprost is a synthetic prostaglandin that stimulates uterine contraction. Carboprost causes bronchoconstriction, and asthma is a contraindication to its use in this patient.
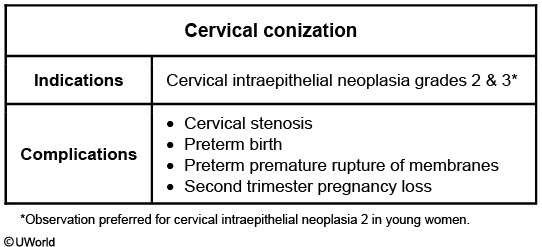
Epithelial Ovarian Carcinoma
Epithelial ovarian carcinoma refers to a malignancy involving the ovary, fallopian tube, and peritoneum. Histologically, abnormalities can begin at any of these sites and present with the hallmark large ovarian mass and widespread pelvic and abdominal metastasis regardless of primary origin.
Ultrasound is the first-line imaging modality to investigate pelvic pain and/or an adnexal mass. This patient's findings of a large ovarian mass with thick septations, solid components, and peritoneal free fluid (ascites) are concerning for malignancy rather than a benign or infectious etiology. The presence of peritoneal fluid in a postmenopausal woman is pathologic and is the origin of the typical symptoms of bloating, pain, early satiety/anorexia, and abdominal distension seen in ovarian cancer.
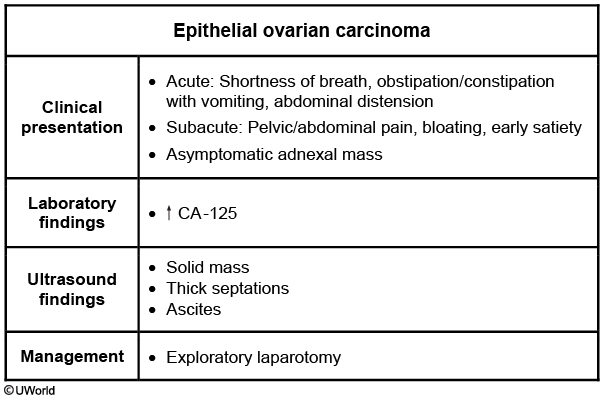
Secondary Amenorrhea
This patient's presentation is consistent with secondary amenorrhea, defined as theabsence of menses for >3 cycles or >6 months in women who menstruated previously. When the etiology is unknown, patients require a stepwise approach in evaluation to rule out treatable causes and aid in future management.
The first step is detailed history and examination followed by a pregnancy test. A patient's menstrual patterns, amount of stress and exercise, medical problems, medications (eg, hormonal contraception, dopamine antagonists), and family history of early menopause should be explored. The examination should assess for signs of hyperandrogenism and other systemic illnesses.
This patient has a negative pregnancy test and no obvious explanation for secondary amenorrhea from her history and examination. Therefore, prolactin, TSH, and FSH should be ordered to differentiate between the most common causes of secondary amenorrhea (hyperprolactinemia, thyroid dysfunction, premature ovarian failure).
Patients with a history of uterine procedures or infection may have scarring of the uterine cavity (eg, Asherman syndrome). Diagnostic workup includes hormonal therapy to test for the ability to grow uterine lining and hysteroscopy to visualize uterine adhesions.
Benign breast
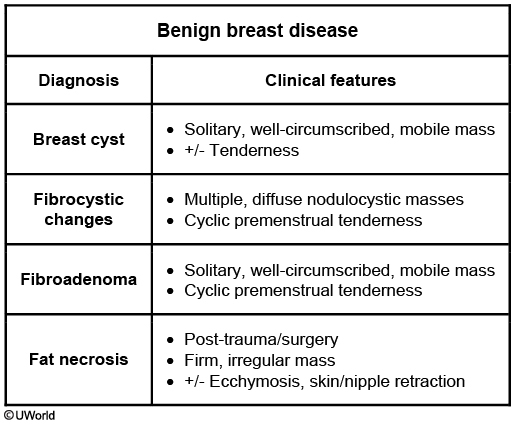
Palpable breast masses are common in adolescents and women age <30, especially immediately prior to menses due to estrogen stimulation. The ideal time to examine the breast is 5-10 days after menses (eg, follicular phase) when hormonal stimulation is minimal. Some masses may be re-evaluated in the next menstrual cycle if not well palpated in the luteal phase.
Small size, regular texture, round shape, and mobility characterize a benign process presenting as a breast cyst (eg, soft, fluid-filled, mobile structure) or fibroadenoma (eg, firm, solid, mobile mass). Both cysts and fibroadenomas may increase in size with estrogen use (eg, combined oral contraceptives) and are associated with premenstrual discomfort. These benign structures may occur anywhere in the breast but are usually in the upper outer quadrants.
Despite this patient being premenstrual, her breast lesion is easily palpated. As fibroadenoma is most common before age 30 and cyst incidence peaks after age 30, fibroadenoma is the most likely diagnosis based on this patient's age.
A palpable breast mass may be evaluated using the "triple diagnostic" (clinical breast examination, imaging studies, biopsy) approach, based on the patient's age and risk factors for breast cancer. This patient's young age and palpable mass with benign features are most suggestive of fibroadenoma. Reassurance may be appropriate for an adolescent with benign findings that include a decrease in the size of a mass after a menstrual period. However, further evaluation is needed to confirm a diagnosis of a new breast mass in an adult as the incidence of cancer increases with age.
Although imaging tests (eg, ultrasound and/or mammogram) are appropriate next steps in management, only a biopsy will confirm the diagnosis. A needle aspiration is performed for small cystic or solid lesions, while core biopsy is preferred for larger solid masses.
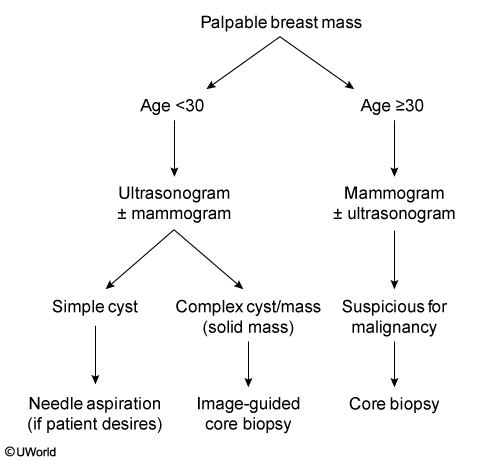
Intrauterine Fetal Demise
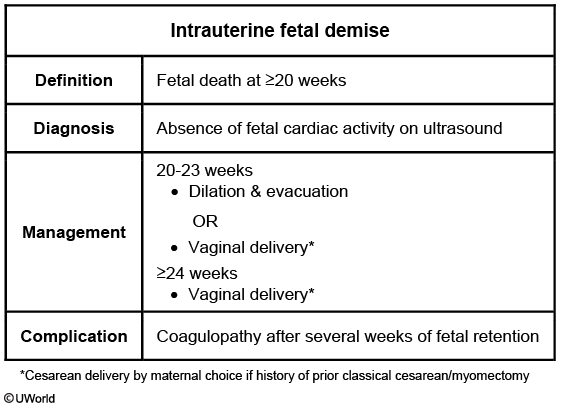
Stillbirth or intrauterine fetal demise (IUFD) refers to fetal death at >20 weeks that occurs prior to expulsion from the mother. Risk factors for IUFD include nulliparity, obesity, hypertension, and diabetes mellitus. Patients typically present with decreased or absent fetal movement. As with this patient, fetal Doppler ultrasound fails to detect a fetal heart rate. Inability to find the fetal heart rate by Doppler sonography is not diagnostic and can be due to fetal malpresentation or maternal obesity. The diagnosis of IUFD must be confirmed by absence of fetal cardiac activity on ultrasound. Vaginal delivery >24 weeks regardless of presentation (breech or vertex). C section for breech is only good for baby and not mom. Perform when patient is ready.
Thorough maternal, fetal, and placental evaluations are necessary to determine the etiology of intrauterine fetal demise (IUFD). After delivery, the fetus should be examined for dysmorphic features and undergo an autopsy. Fetal karyotype should be performed and other genetic studies should be considered. A gross and microscopic placental evaluation is necessary to evaluate for signs of abruption (eg, clotted blood) or infection. The membranes and umbilical cord should also be inspected (eg, nuchal cords, true knots).
Maternal evaluation should include laboratory testing for antiphospholipid antibody syndrome and fetomaternal hemorrhage. A thrombophilia evaluation can be considered for patients with histories that suggest this etiology (eg, recurrent pregnancy loss, family or personal history of venous thrombosis, intrauterine growth restriction.)
Although determination of IUFD etiology can assist with anticipatory guidance in future pregnancies, often no etiology is found.
Fetal Growth Restriction
Fetal growth restriction
Symmetric
Asymmetric
Definition
Ultrasound estimated fetal weight <10th percentile for gestational age
Onset
1st trimester
2nd/3rd trimester
Etiology
Chromosomal abnormalities Congenital infection
Utero-placental insufficiency Maternal malnutrition
Clinical features
Global growth lag
"Head-sparing" growth lag
Management
Weekly biophysical profiles Serial umbilical artery Doppler sonography Serial growth ultrasounds
Fetal growth restriction (FGR) is defined as an estimated fetal weight <10th percentile for gestational age. Fetuses with growth restriction have increased risk of intrauterine demise and neonatal morbidity/mortality (eg, preterm delivery).
FGR can be characterized as symmetric or asymmetric. Congenital disorders or insults during the first trimester (eg, aneuploidy, infections) are the most common causes of symmetric FGR (eg, the entire fetus is affected). Asymmetric FGR, the result of placental dysfunction during the second and/or third trimester, is associated with conditions that cause placental insufficiency (eg, hypertension, pregestational diabetes). In normal fetal development, the fetal abdomen grows exponentially during the second and third trimester. Insults (eg, hypoxemia) at this stage of pregnancy cause fetal blood flow to be redistributed to the vital organs (eg, brain) and away from the abdomen, resulting in an asymmetric, or "head-sparing," growth pattern.
In this patient, the fetal head is 2 weeks smaller and the abdomen is 7 weeks smaller than expected for gestational age, indicating asymmetric FGR. The patient's hypertension is the most likely cause. Even when well controlled, hypertension can cause underdevelopment of the spiral arteries in the placenta, resulting in increased vascular resistance. These vascular alterations can cause placental insufficiency and, subsequently, asymmetric FGR.
Placenta Accreta
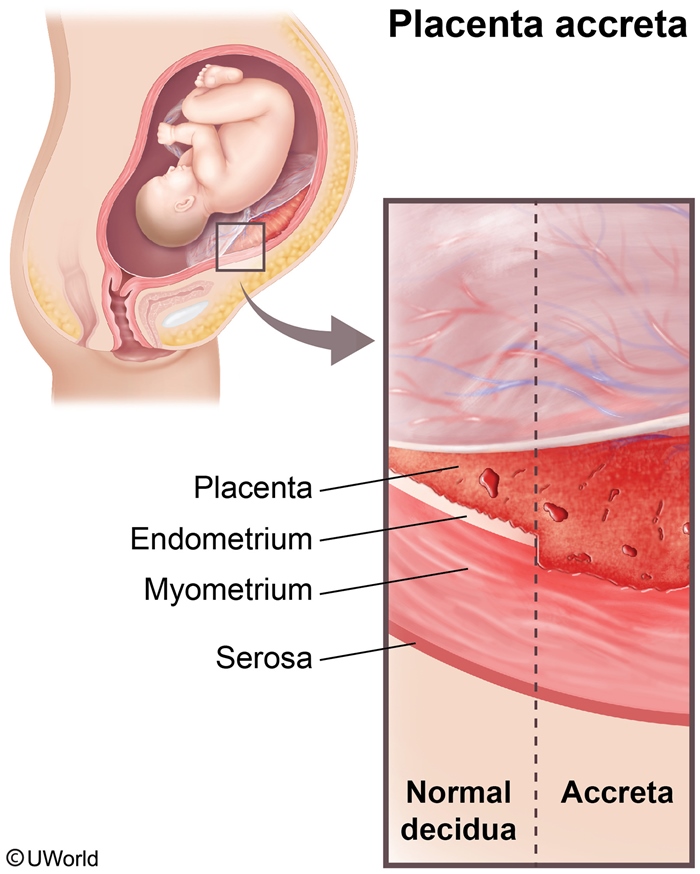
Placenta accreta occurs when uterine villi attach directly to the myometrium instead of the decidua. Risk factors for placenta accreta include a prior cesarean delivery, a history of dilation and curettage, and maternal age >35. Placenta accreta is typically diagnosed by antenatal ultrasound findings that include irregularity or absence of the placental-myometrial interface and intraplacental villous lakes. Antenatally diagnosed placenta accreta is delivered by planned cesarean hysterectomy.
Undiagnosed placenta accreta presents as difficulty with placental delivery. The placenta does not detach from the uterus, and this often results in cord avulsion and necessitates a manual extraction, which is then complicated by placental adherence and severe hemorrhage (as seen in this patient).
Vasa Previa
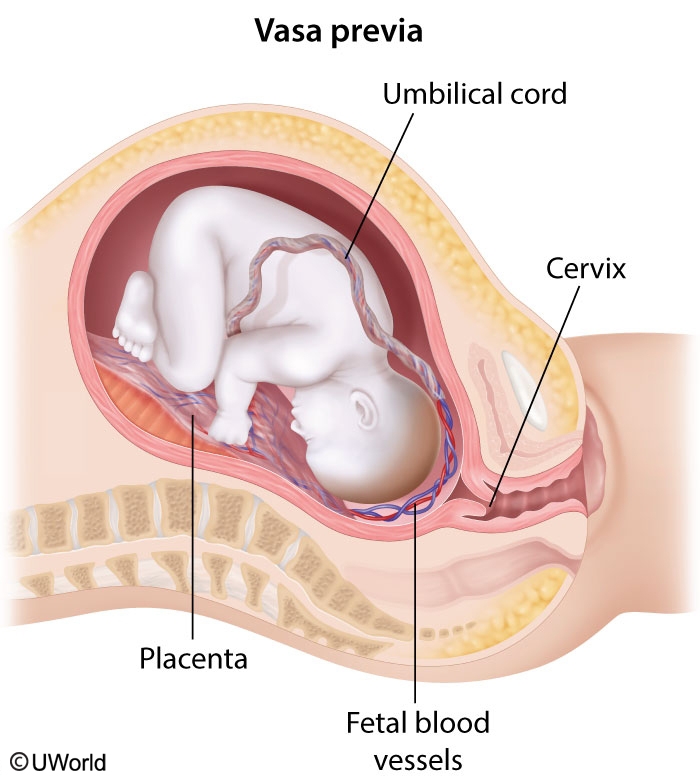
Vasa previa occurs when fetal vessels traverse the amniotic membranes over the internal cervical os. It presents with painless antepartum bleeding and fetal heart rate abnormalities just after the rupture of membranes. Should these vessels break during membrane rupture, fetal exsanguination can occur in minutes. Vasa previa presents with painless vaginal bleeding on membrane rupture in addition to fetal bradycardia or a sinusoidal heart rate tracing.
Lactation Suppression
Lactation suppression is accomplished by wearing a comfortable, supportive bra, avoidance of nipple stimulation and manipulation, application of ice packs to the breasts, and nonsteroidal anti-inflammatory drugs to reduce inflammation and pain. Breast binding is not recommended for lactation suppression due to the risk of mastitis, plugged ducts, and increased pain. In addition, a tight bra or binder may lead to inadvertent nipple stimulation.
Engorgement itself creates a chain of events that lead to cessation of the lactation process due to negative inhibition of prolactin release. Current evidence does not support the use of medications for lactation suppression.
Herpes
Cesarean delivery is recommended to all women who are in labor with active genital HSV lesions or prodromal symptoms (eg, burning, pain).
Pregnant women with a history of genital HSV infection should receive prophylactic acyclovir or valacyclovir beginning at 36 weeks of pregnancy. This reduces the risk of an outbreak around the time of delivery and therefore reduces the risk for needing a cesarean delivery. However, neither therapy at the time of delivery nor prophylactic antiviral therapy has been shown to decrease the risk for neonatal HSV infection.
Preterm Labor Prevention
Uterine Inversion
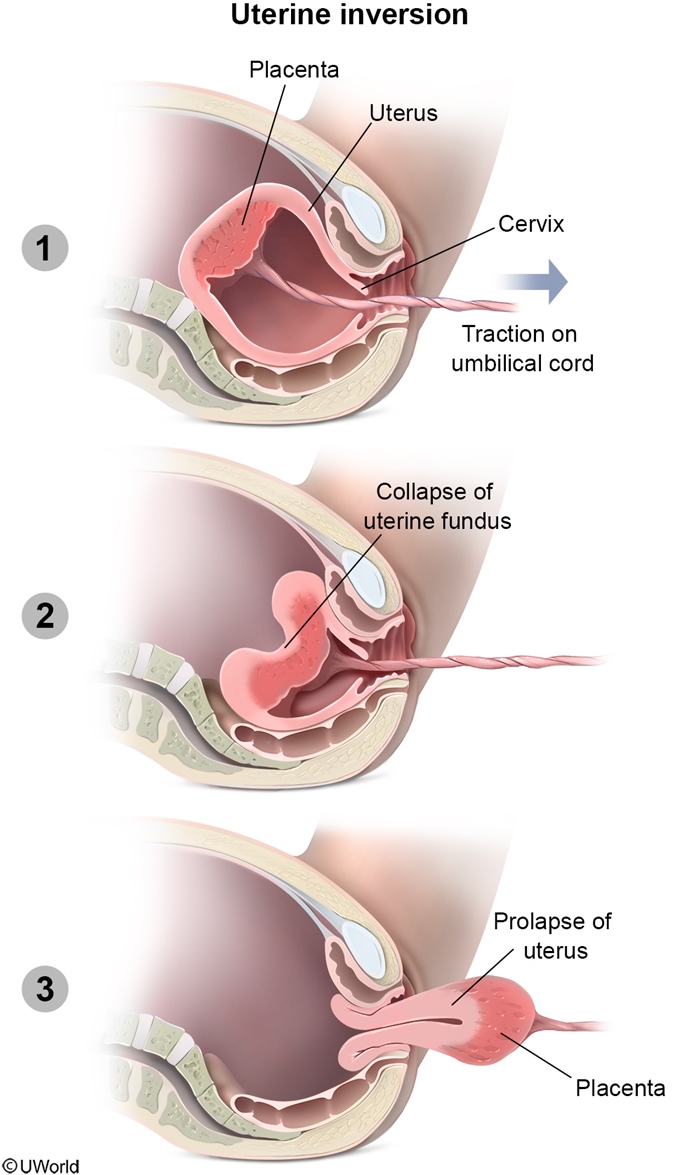
Uterine inversion is an uncommon but potentially fatal cause of postpartum hemorrhage. Risk factors for uterine inversion include nulliparity, fetal macrosomia, placenta accreta, and a rapid labor and delivery.
Uterine inversion can result from excessive fundal pressure and traction on the umbilical cord before placental separation. The fundus collapses into the endometrial cavity and prolapses through the cervix, resulting in a smooth, round mass protruding through the cervix or vagina. The uterine fundus is no longer palpable transabdominally. Uterine inversion is typically accompanied by hemorrhagic shock and lower abdominal pain, as seen in this patient.
Management:
Manual replacement of the uterus
Placental removal & uterotonic drugs after uterine replacement
Fibroids
Choriocarcinoma
Choriocarcinoma is a form of gestational trophoblastic neoplasia, a malignancy that arises from placental trophoblastic tissue and secretes β-hCG. Although it most commonly follows a hydatidiform mole, choriocarcinoma can occur after a normal gestation or spontaneous abortion. Choriocarcinoma typically presents <6 months after a pregnancy. Presenting symptom include irregular vaginal bleeding, an enlarged uterus, and pelvic pain. Choriocarcinoma is an aggressive type of gestational trophoblastic neoplasia; the most common site of metastatic spread is to the lungs. Symptoms of pulmonary metastasis include chest pain, hemoptysis, and dyspnea. When choriocarcinoma is suspected, obtaining a quantitative β-hCG level helps to confirm the diagnosis.
CA 125
Cancer antigen 125 (CA-125) is a biomarker for epithelial ovarian cancer. Elevations are also caused by common gynecologic conditions (eg, leiomyomata, endometriosis) that are more likely present in premenopausal patients; therefore, the specificity of CA-125 levels is much greater in postmenopausal women.
CA-125 levels are measured in conjunction with pelvic ultrasonography findings to categorize an ovarian mass as likely malignant or benign. This postmenopausal patient has no medical conditions that may cause a false elevation of CA-125, so measurement is the best next step to investigate the risk of malignancy for this ovarian cyst. CA-125 levels can also be used to monitor for recurrence of a proven malignancy after treatment.
In a postmenopausal patient, an elevated CA-125 level in the context of any adnexal mass is highly suspicious for malignancy. If the adnexal mass has no malignant features on ultrasound (eg, small size, simple cyst) and the CA-125 level is normal, the patient can be observed with periodic ultrasound, but observation without further workup is inappropriate in a postmenopausal patient. If there are suspicious features on ultrasound (eg, large mass, solid components, septations) and/or if the CA-125 level is elevated, the patient should undergo further imaging (eg, MRI, CT scan) to assess the extent of disease. Knowledge of the presence of metastatic implants from imaging is important to guide surgical exploration, which is recommended if malignancy is suspected based on clinical, CA-125, and imaging findings.
Incontinence
Etiology
Symptoms
Stress
↓ Urethral sphincter tone Urethral hypermobility
Leakage with coughing, lifting, sneezing
Urge
Detrusor hyperactivity
Sudden, overwhelming urge to urinate
Overflow
Impaired detrusor contractility Bladder outlet obstruction
Incomplete emptying & persistent involuntary dribbling
Stress: kegel, pessary, pelvic floor surgery
Urge: Antimuscarinic (Oxybutynin)
Overflow: Muscarinc (Bethanechol, catherterization)
Theca Lutein Cyst
Theca lutein cysts typically form due to ovarian stimulation by high β-hCG levels (eg, molar pregnancy) and resolve after these levels decline. On ultrasound, they appear as multiseptated bilateral cystic masses and do not have calcifications or hyperechoic nodules. These cysts do not present outside of pregnancy.
Dermoid cysts in particular have a higher likelihood of torsion than other types of ovarian masses. A mass on the ovary puts weight on the adnexa and makes it vulnerable to twisting around its supporting structures (infundibulopelvic ligament or utero-ovarian ligament), which contain the ovarian blood supply.
OCP SE
Breakthrough bleeding
Breast tenderness, nausea, bloating
Amenorrhea
Hypertension
Venous thromboembolic disease
Decreased risk of ovarian & endometrial cancer
Increased risk of cervical cancer
Liver disorders (eg, hepatic adenoma)
Increased triglycerides (due to estrogen component)
CI with breast cancer
Early side effects of OCPs include nausea, bloating, and breast tenderness, which usually improve with continued use. Breakthrough bleeding is the most common side effect and is usually associated with lower estrogen doses. Adverse effects include hypertension, increased risk of cervical cancer, and venous thromboembolism. Although weight gain as a side effect is a common perception, several studies have shown no significant weight gain, particularly with low-dose formulations. As a result, this patient can be reassured that weight gain is not associated with continued OCP use.
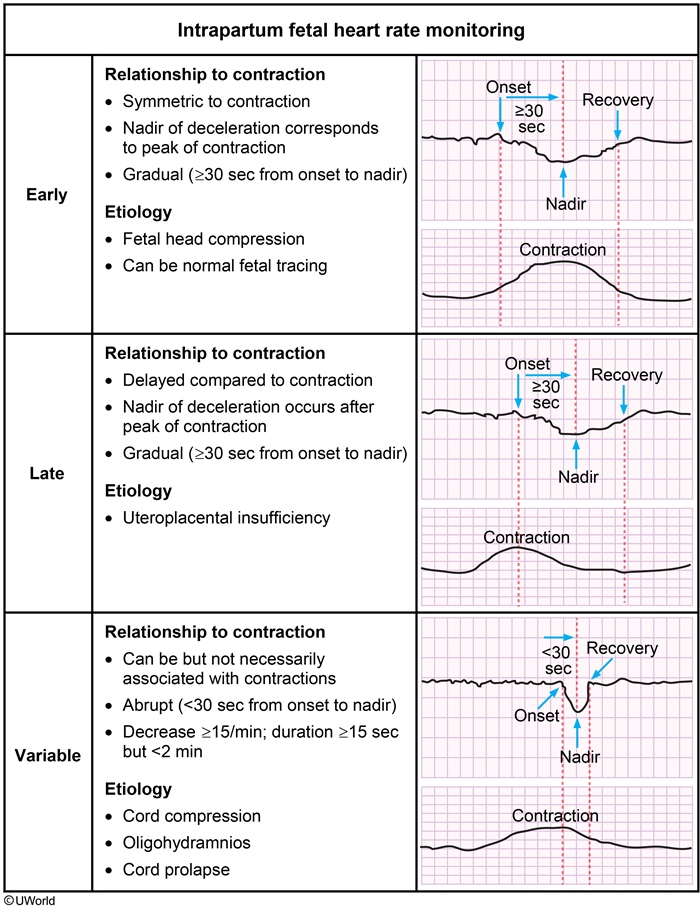
Deceleration
Epidural SE
Hypotension occurs when the sympathetic nerve fibers responsible for vascular tone are blocked, resulting in vasodilation (venous pooling), decreased venous return to the right side of the heart, and decreased cardiac output. Persistent, untreated hypotension can result in decreased placental perfusion and can lead to fetal acidosis. It can be prevented by aggressive intravenous fluid volume expansion prior to epidural placement. Treatment includes left uterine displacement (positioning patient on the left side) to improve venous return, additional intravenous fluid bolus, or vasopressor administration.
Depression of cervical spinal cord and brainstem activity occurs when local anesthesia ascends toward the head, also known as a "high spinal" or "total spinal," a dangerous complication of epidural anesthesia. It may happen with intrathecal injection or overdose of the anesthetic. First signs include hypotension, bradycardia, and respiratory difficulty, and later, diaphragmatic paralysis and possibly cardiopulmonary arrest.
Leakage of cerebral spinal fluid may occur if the dura is inadvertently punctured during epidural placement. This results in leakage of spinal fluid and is known as a "wet tap." Patients may experience postural headaches that are worse with sitting up and improved with lying down after delivery. Hypotension is not characteristic.
Fetal Growth Restriction
Definition
Weight <10th percentile for gestational age
Risk factors
Maternal hypertension Pregestational diabetes mellitus Genetic abnormalities Congenital infection
Appearance
Large anterior fontanel Thin umbilical cord Loose, peeling skin Minimal subcutaneous fat
Evaluation
Placenta histopathology Consider karyotype, urine toxicology, serology
Neonatal complications
Polycythemia Hypoglycemia Hypocalcemia Poor thermoregulation
Fetal growth restriction (FGR) is defined as an ultrasound-estimated fetal weight <10th percentile for gestational age. At delivery, infants with FGR have thin, loose skin; a thin umbilical cord; and a wide anterior fontanel. Other common features at delivery include meconium-stained amniotic fluid and decreased subcutaneous fat.
Although the underlying cause of FGR can be of fetal, maternal, or placental origin, the results are usually utero-placental insufficiency and poor fetal growth. Therefore, the placenta should undergo histopathologic examination to evaluate for the presence of infarction and/or infection (eg, spirochetes). FGR can be caused by maternal substance abuse, genetic abnormalities, and congenital infection. Consequently, a neonatal urine toxicology screen and serology (eg, for cytomegalovirus, toxoplasmosis, and rubella) can be performed. If physical examination of the infant suggests a syndromic etiology, a karyotype may be indicated.
Intrahepatic Cholestatsis
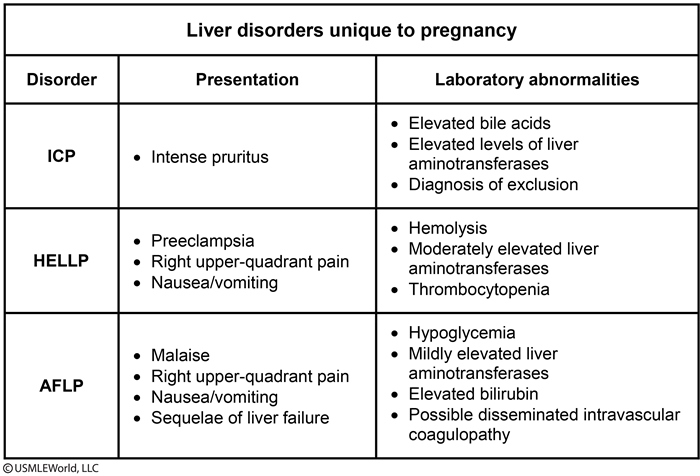
This patient's presentation is most consistent with intrahepatic cholestasis of pregnancy (ICP). ICP is a functional disorder of bile formation that develops in the second and third trimesters. The etiology is unclear, but it is thought that hormonal (eg, higher levels of estrogen or progesterone later in pregnancy), genetic, and environmental factors influence its development.
Clinical manifestations of ICP include intense, often intolerable, generalized pruritus that is especially significant on the palms and soles and worsens at night. Evidence of skin excoriations may be present on examination. Fewer than 10% of patients have jaundice. Serum total bile acids are typically increased and may be the only abnormal laboratory finding. Liver function studies are sometimes suggestive of cholestasis, with alkaline phosphatase and the total and direct bilirubin increased (although alkaline phosphatase is elevated in normal pregnancy). Serum aminotransferases may be 10 times normal (sometimes >1000 U/L), which requires that viral hepatitis be ruled out.
Treatment is based on symptom relief, and pruritus resolves in the weeks following delivery. Ursodeoxycholic acid is commonly prescribed to increase bile flow and relieve itching. Maternal prognosis is generally good. However, early delivery is recommended once fetal maturity is achieved to avoid fetal complications (eg, intrauterine demise, neonatal respiratory distress syndrome).
Fetal Surveillance
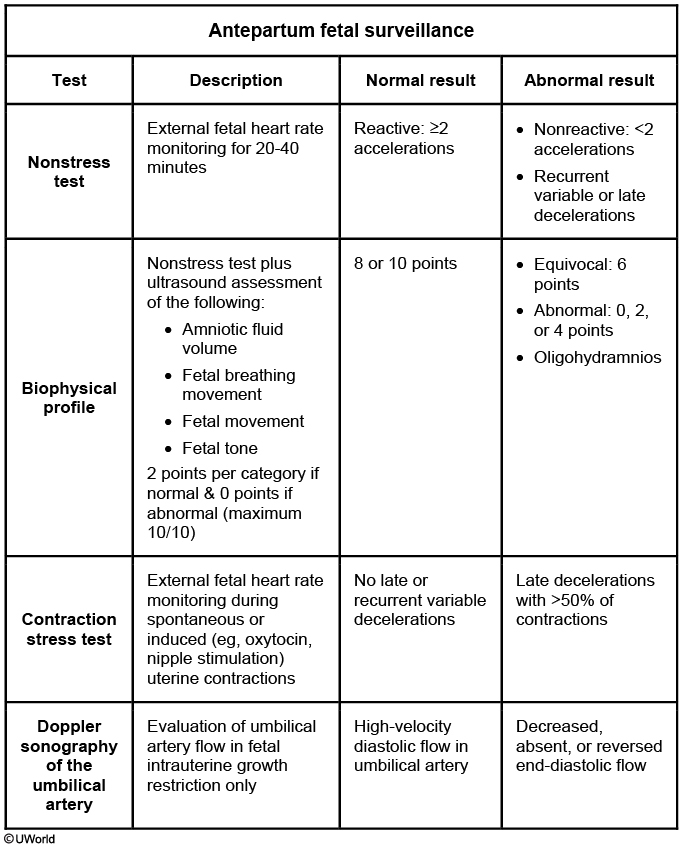
Component
Normal finding
Nonstress test
Reactive fetal heart rate monitoring
Amniotic fluid volume
Single fluid pocket ≥2 cm × 1 cm or amniotic fluid index >5
Fetal movements
≥3 general body movements
Fetal tone
≥1 episodes of flexion/extension of fetal limbs or spine
Fetal breathing movements
≥1 breathing episode for ≥30 seconds
This patient presents with decreased fetal movement, a subjective and nonspecific symptom that may be benign (eg, normal fetal sleep cycle) or ominous (eg, central nervous system hypoxia). A nonstress test (NST) is performed to assess fetal status and identify fetuses at risk of adverse outcomes. During an NST, the heart rate of a well-oxygenated fetus rises with fetal movement (accelerations). A reactive NST(>2 accelerations) has a high negative predictive value to rule out fetal acidemia. A nonreactive NST has a high false-positive rate and low positive predictive value and cannot rule in fetal acidemia.
A nonreactive NST requires further evaluation with a biophysical profile (BPP) or contraction stress test (CST). These tests are equivalent in assessing fetal status and are selected based on available resources and relevant contraindications. A BPP includes an NST plus an ultrasound evaluation of the amniotic fluid index as well as fetal movement, tone, and breathing. A CST is performed by administering oxytocin or using nipple stimulation until 3 contractions occur every 10 minutes. Contraindications to CST include contraindications to labor (eg, placenta previa, prior myomectomy). Therefore, a BPP is more appropriate for this patient.
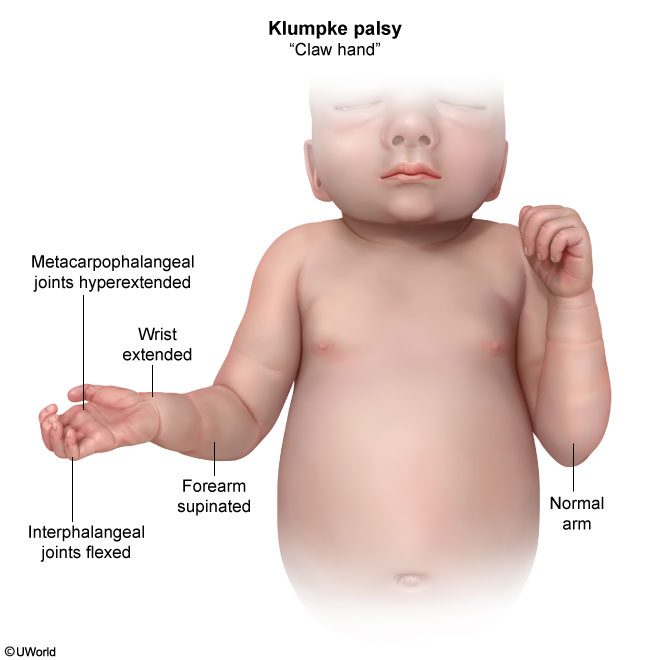
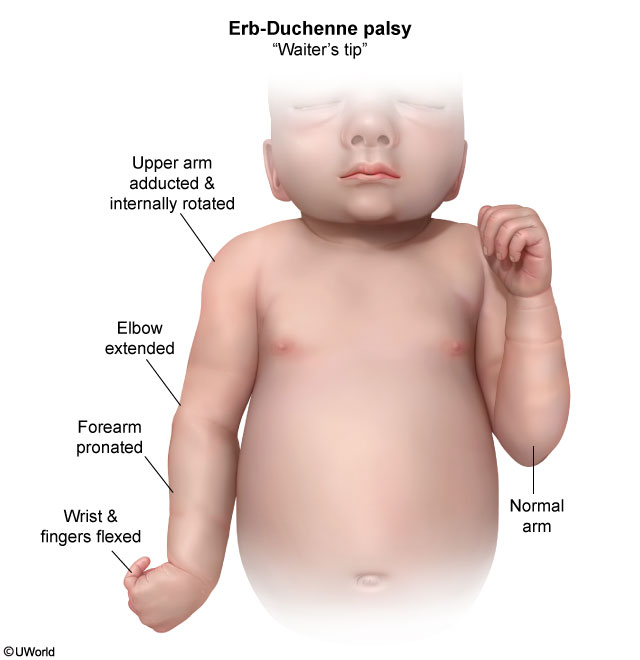
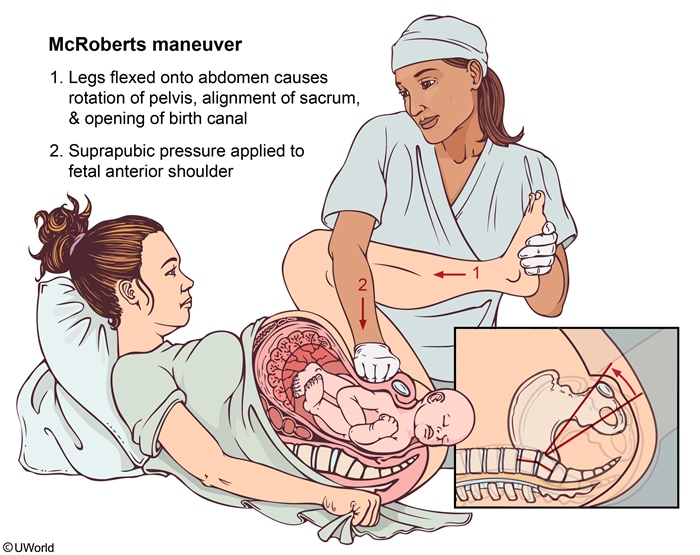
Shoulder Dystocia
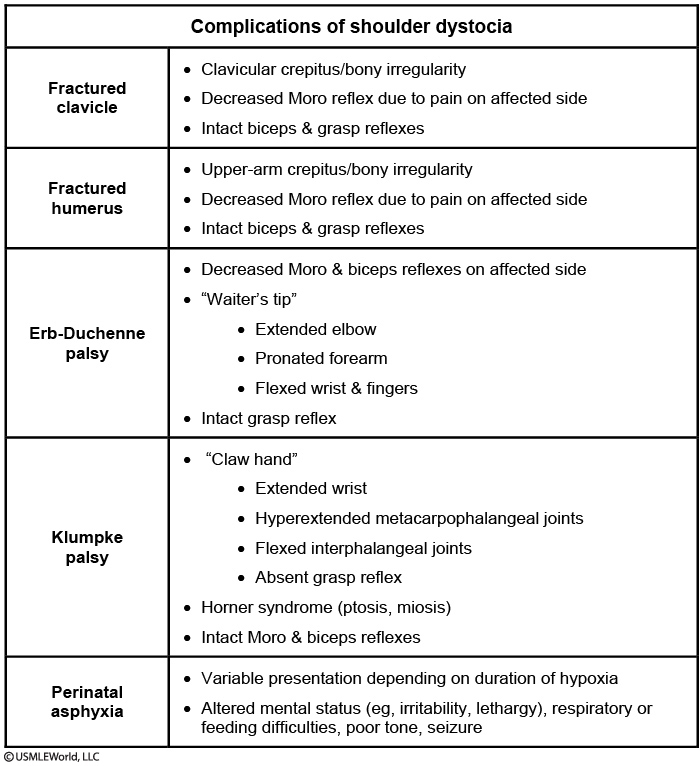
This infant has Klumpke palsy due to shoulder dystocia. Risk factors include infant large for gestational age (birth weight >4 kg), maternal diabetes, and maternal obesity. Excessive traction of the 8th cervical (C8) and 1st thoracic (T1) nerves during delivery can result in the rare complication of left hand paralysis. Sometimes, there is associated damage to the sympathetic fibers that run along C8 and T1 that manifests as ipsilateral miosis and ptosis (Horner syndrome).
Prognosis depends on whether damage was due to nerve stretching or compression as opposed to avulsion. Horner syndrome also portends a suboptimal outcome. Treatment is controversial but usually involves gentle massages and physical therapy to prevent contractures. In most cases, function returns within a few months. If there is no improvement by age 3-9 months, surgical intervention may be considered.
The differential diagnosis of abnormal arm movement includes such other potential complications of difficult shoulder delivery as fractures of the clavicle or humerus, Erb-Duchenne palsy, and cerebral injury from perinatal asphyxia.
HIV management
start ART asap, avoid any artificial ROM and vaginal operative delivery
viral load < 1000, ART + vaginal
viral load > 1000, ART + zidovudine + c section
postpartum: continue ART for mom, give zidovudine for baby if viral 1000
Stop Pap
When to stop Pap testing
Age 65 or hysterectomy PLUS No history of cervical intraepithelial neoplasia 2 or higher AND 3 consecutive negative Pap tests OR 2 consecutive negative co-testing results
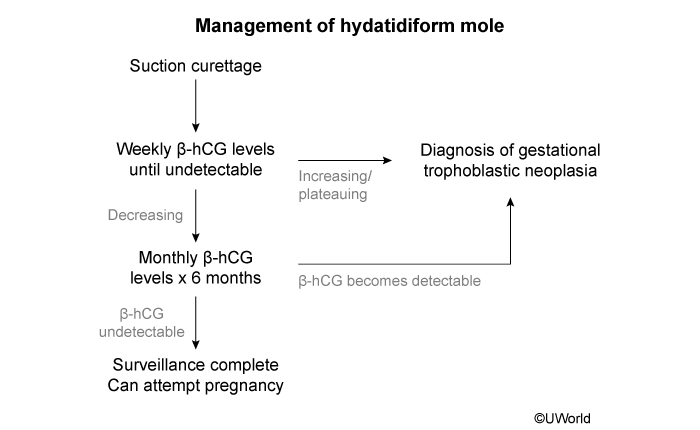
Mole
Pubic Symphysis Diastasis
Pubic symphysis diastasis
Risk factors
Fetal macrosomia Multiparity Precipitous labor Operative vaginal delivery
Presentation
Difficulty ambulating Radiating suprapubic pain Pubic symphysis tenderness Intact neurologic examination
Management
Conservative Nonsteroidal anti-inflammatory drugs Physical therapy Pelvic support
During pregnancy, increased levels of progesterone and relaxin increase pelvic mobility and promote a physiologic widening (diastasis) of the pubic symphysis to facilitate vaginal delivery. However, after a traumatic delivery, patients can develop a symptomatic pubic symphysis diastasis. Risk factors include fetal macrosomia, forceps-assisted vaginal delivery, and multiparity. Symptomatic pubic symphysis diastasis typically presents with suprapubic pain that radiates to the back or hips and is exacerbated by weight-bearing, walking, or position changes. The diagnosis is made clinically; patients have point tenderness to palpation over the pubic symphysis and sometimes have a waddling gait. Management is typically conservative with supportive care (eg, pelvic support, physical therapy), and most patients recover within the first 4 weeks postpartum.
Femoral Nerve Damage
Femoral nerve damage can occur during delivery as a result of hyperflexion of the thigh (eg, McRoberts maneuver). It presents with numbness over the anterior and medial thigh, inability to extend the leg or flex the thigh, and diminished patellar reflexes, none of which are seen in this patient.
Septic Abortion
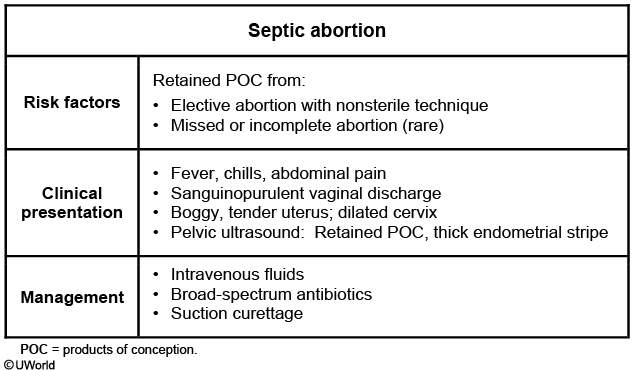
This patient's presentation is consistent with a septic abortion, which typically presents with fever; lower abdominal pain; heavy vaginal bleeding; and amalodorous, purulent vaginal discharge. It can occur as a complication of any type of abortion but most frequently follows an unsterile and/or incomplete procedure for an elective abortion. Findings of a purulent discharge and enlarged, boggy, tender uterus on pelvic examination and an ultrasound showing intrauterine echogenic material with blood flow are consistent with inflammation and infection from retained products of conception.
Although the infection usually remains confined to the placental tissue of the retained products of conception, if untreated or observed (Choice D) it can spread into the uterine myometrium and can cause widespread infection. Due to these potential complications, a septic abortion is a medical emergency that requires prompt treatment to prevent progression to peritonitis, septic shock, and death. Treatment includes broad-spectrum antibiotics and uterine evacuation with suction curettage.
Bartholin gland
Bartholin glands are located bilaterally at the posterior introitus and drain through ducts into the vestibule at the 4 and 8 o'clock positions. These pea-sized glands provide lubrication to the vestibule and are not palpable unless ductal blockage occurs, resulting in fluid buildup and cyst formation.
This patient has a Bartholin gland cyst, which is common in women age <30. Physical examination shows a mobile, soft, nontender, well-circumscribed mass behind the labium majus, with vaginal extension. Small cysts may be diagnosed incidentally on routine examination, or a partner may discover it during sexual activity. Larger cysts may cause discomfort during sexual activity, walking, sitting, or exercise. Symptomatic cysts require incision and drainage, followed by Word catheter placement.
Late term
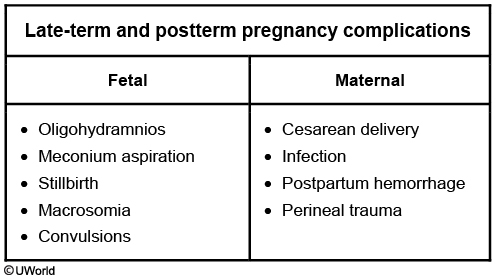
Pregnancies at 41 weeks or beyond are defined as late-term (41 weeks to 41 weeks and 6 days gestation) or postterm (>42 weeks gestation) from the last menstrual period. Risk factors include nulliparity, history of prior postterm pregnancy, maternal obesity, and fetal anomalies (eg, anencephaly). An induction of labor can be considered for late-term pregnancy and is recommended for postterm pregnancies to prevent complications (Table). Antepartum fetal testing may be started at 41 weeks gestation to assess fetal well-being. Oligohydramnios (single deepest vertical pocket of amniotic fluid <2 cm or an amniotic fluid index of <5 cm on transabdominal ultrasound) is a common complication of prolonged pregnancies. An aging placenta may have decreased fetal perfusion, resulting in decreased renal perfusion and decreased urinary output from the fetus. The diagnosis of oligohydramnios is an indication for delivery even if antepartum fetal testing is normal.
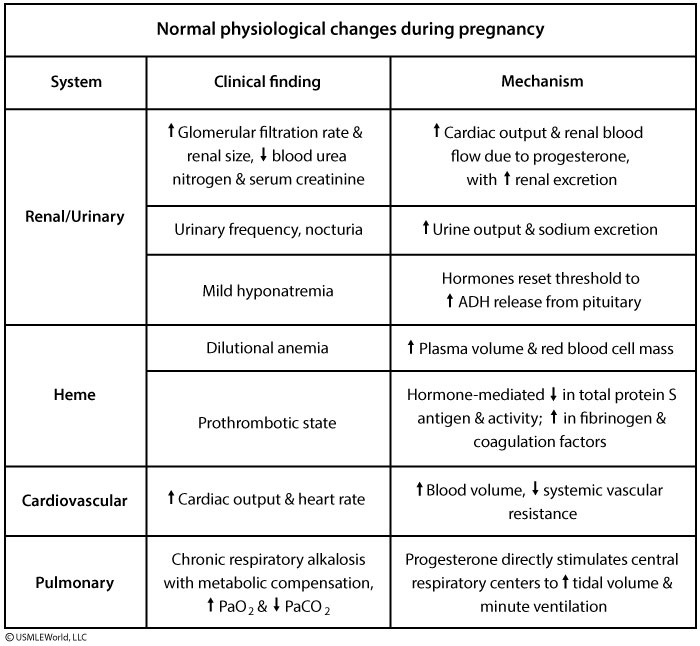
Renal
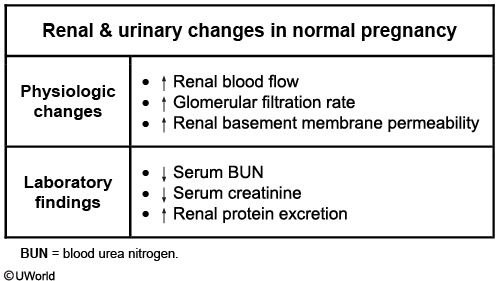
In a normal pregnancy, both the glomerular filtration rate (GFR) and renal blood flow are increased, which cause the serum blood urea nitrogen and creatinine to become decreased compared to prepregnancy levels. Renal function increases gradually in the first trimester and reaches 40%-50% above the nonpregnant state by midpregnancy, after which it remains unchanged until term. Renal basement membrane permeability is also increased in pregnancy.
Due to the increase in renal function during pregnancy, patients on medications that are renally excreted (eg, gabapentin) require close monitoring and dose adjustments as necessary. In addition, a serum creatinine of 1.2 mg/dL may be the upper limit of normal in a nonpregnant woman but is considered renal insufficiency in a pregnant woman.
Preterm Labor
Preterm labor
Gestational age (weeks)
Management
34 0/7 to 36 6/7
± Betamethasone Penicillin if GBS positive or unknown
32 0/7 to 33 6/7
Betamethasone Tocolytics (delay delivery) Penicillin if GBS positive or unknown
<32
Betamethasone Tocolytics Magnesium sulfate Penicillin if GBS positive or unknown
The management of preterm labor is largely dependent on gestational age. At >34 weeks gestation, tocolytics such as indomethacin and nifedipine are not recommended as the risks of indomethacin (oligohydramnios, closure of the ductus arteriosus) and nifedipine (maternal hypotension/tachycardia) outweigh the risks of premature delivery.
Because tocolysis is contraindicated, this patient's labor will likely progress. In the absence of contraindications to vaginal delivery, patients who present in preterm labor at >34 weeks gestation can be managed expectantly. However, due to an increased risk for fetal injury and asphyxia, a vaginal delivery is contraindicated for a singleton breech fetus. Consequently, the best option for managing this patient's preterm labor is cesarean delivery. Active labor is a relative contraindication for external cephalic version.
Regardless of delivery route, patients in preterm labor at <37 weeks gestation are candidates for betamethasone, which can reduce the incidence of neonatal respiratory distress syndrome. All patients in preterm labor who are either group BStreptococcus (GBS) positive or unknown and who will deliver vaginally should receive intravenous penicillin to prevent the vertical transmission of GBS. Patients at <37 weeks who will deliver by cesarean require penicillin only if they are GBS positive or unknown and have ruptured membranes.
Although magnesium sulfate is a weak tocolytic, it is not typically administered for tocolysis but instead for lowering the risk of neurologic comorbidities (cerebral palsy) in neonates born at <32 weeks gestation. Magnesium sulfate is therefore not indicated in this patient at 35 weeks gestation.
Routine Prenatal
Routine prenatal
Initial prenatal visit
Rh(D) type, antibody screen, Hemoglobin/hematocrit, MCV, HIV, VDRL/RPR, HBsAg, Rubella & varicella immunity, Pap test (if screening indicated), Chlamydia PCR, Urine culture, Dipstick for urine protein
24-28 weeks
Hemoglobin/hematocrit, Antibody screen if Rh(D) negative, 50-g 1-hour GCT
35-37 weeks
Group B Streptococcus culture
Emergency contraception
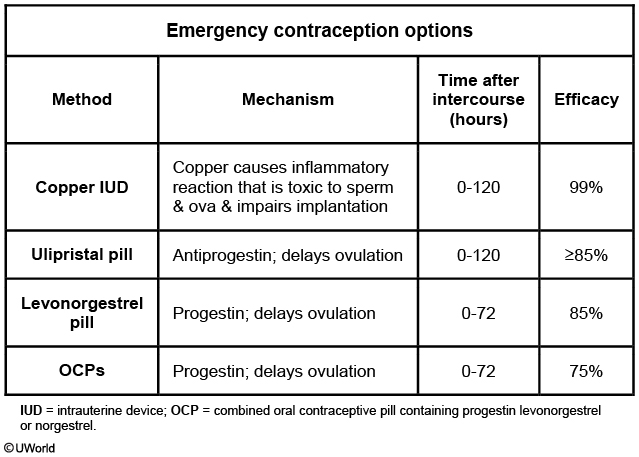
"Emergency" (or postcoital) contraception refers to medications or devices used after intercourse to prevent pregnancy by delaying ovulation or impairing implantation. They are not effective after implantation (when pregnancy has started). The copper intrauterine device (IUD), a precoital contraceptive, is the most effective emergency contraceptive. It may be inserted up to 5 days following unprotected intercourse. Age and parity are not contraindications; therefore, it may be used in nulligravid adolescents. However, acute cervicitis and pelvic inflammatory disease are contraindications.
Genital lesions
Infectious genital ulcers
Painful
Herpes simplex virus
Small vesicles or ulcers on erythematous base Mild lymphadenopathy
Haemophilus ducreyi (chancroid)
Larger, deep ulcers with gray/yellow exudate Well-demarcated borders & soft, friable base Severe lymphadenopathy that may suppurate
Painless
Treponema pallidum (syphilis)
Single ulcer (chancre) Regular borders & hard base
Chlamydia trachomatis serovars L1-L3 (lymphogranuloma venereum)
Small, shallow ulcers (often missed) Can progress to painful, fluctuant adenitis (buboes)
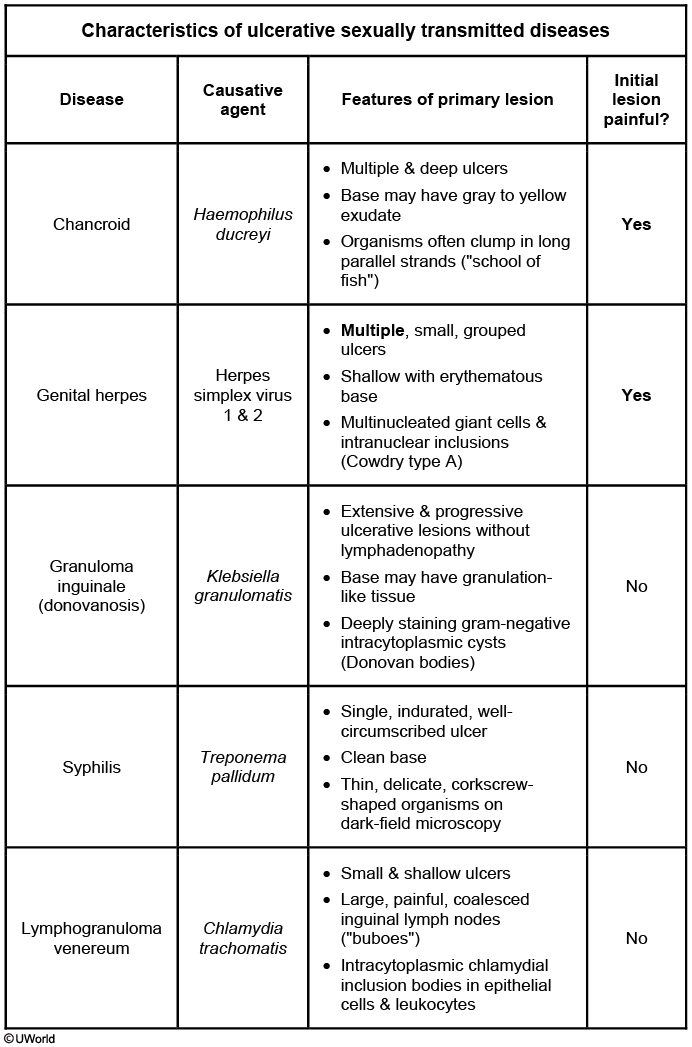
Patients with multiple sexual partners and substance abuse are at high risk for sexually transmitted infections. This patient has classic symptoms of primary syphilis - bilateral inguinal lymphadenopathy and a painless genital chancre. Syphilitic chancres form at the site of direct inoculation with Treponema pallidum. After exposure (3-60 days), patients develop a single papule that turns into a shallow, painless, nonexudative ulcer with indurated edges. Chancres are exceedingly infectious, with rates of T pallidum transmission as high as 30%. Most chancres resolve spontaneously in 6-8 weeks (if untreated), but the systemic spread of T pallidum results in continued infection.
Behçet syndrome, chancroid, and herpes genitalis are usually characterized by multiple, painful genital lesions (not a single, painless lesion). Chancroid, caused by Haemophilus ducreyi, is most commonly found in developing regions but is rare in the United States. Behçet syndrome is thought to be a vasculitis and is marked by recurrent oral aphthous ulcers, often with significant systemic manifestations (including genital ulcers).
Granuloma inguinale is caused by Klebsiella granulomatis and is marked by the formation of extensive, progressive, and painless genital ulcers, usually without lymphadenopathy. Granuloma inguinale is seen primarily in India, Guyana, and New Guinea. In the United States, <100 infections occur annually, most in patients who have traveled to these countries.
Postpartum
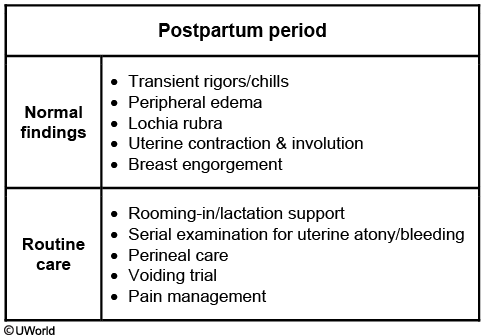
Early puerperium is characterized by several physiologic processes that can be mistaken for signs of pathology. Immediately after placental delivery, shivering occurs commonly and is theorized to be due to thermal imbalance. The uterus contracts and becomes firm and globular with the fundus typically 1-2 cm above or below the umbilicus. During the first few days after delivery, lochia rubra occurs, which is a red or reddish-brown vaginal discharge (the normal shedding of the uterine decidua and blood), as seen in this patient. After 3-4 days, the discharge becomes thin and pink or brown colored (lochia serosa). After 2-3 weeks, the discharge becomes white or yellow (lochia alba).
As this patient's examination is normal, only routine postpartum care is indicated. This includes perineal care, pain management, a voiding trial, and lactation support. Fundal and perineal pad checks should be performed to screen for signs of postpartum hemorrhage (eg, "boggy" uterus, heavy vaginal bleeding, unstable vital signs).
Postpartum fever
Postpartum fever is defined as a temperature >38 C (100.4 F) after the first 24 hours post delivery. This patient has a temperature of 37.9 C (100.2 F) and no signs of endometritis (eg, uterine tenderness, foul-smelling lochia) or other infection. Consequently, antibiotics are not indicated.
Preeclampsia
Uteroplacental insufficiency can lead to fetal growth restriction/low birth weight (ie, small for gestational age infant) even if the neonate is delivered at term. Maternal complications from preeclampsia include abruptio placentae, disseminated intravascular coagulation, and eclampsia.
Atypical Glandular Cells
Atypical glandular cells (AGC) on Pap testing may be due to either cervical or endometrial adenocarcinoma. AGC in women age >35 or women age <35 with risk factors (eg, obesity, anovulation) requires evaluation for endometrial cancer in addition to cervical pathology. Therefore, AGC on Pap testing is investigated with colposcopy, endocervical curettage, and endometrial biopsy to evaluate the ectocervix, endocervix, and endometrium. As a result, a return to routine Pap screening is not indicated.
Genito pelvic pain
Genito-pelvic pain/penetration disorder
Risk factors
Sexual trauma Lack of sexual knowledge History of abuse
Clinical features
Pain with vaginal penetration Distress/anxiety over symptoms No other medical cause
Treatment
Desensitization therapy Kegel exercises
This patient has genito-pelvic pain/penetration disorder, previously known as vaginismus, characterized by pain on and an aversion to attempted vaginal penetration. Genito-pelvic pain/penetration disorder may be limited to primarily a sexual context or include pain with tampon insertion and gynecologic examinations. This condition causes psychological distress and may have an identifiable cause, such as a history of vaginal trauma. The condition is underreported due to significant patient anxiety and avoidance of examinations. Examination differentiates it from other pathologies (eg, infectious vaginitis, vulvodynia) but may be limited as patients often cannot tolerate speculum insertion. Patients have no tenderness on external examination. Treatment is aimed at relaxing the vaginal muscles and includes desensitization therapy and Kegel exercises.
Preeclampsia severe features
SBP >160 mm Hg or DBP >110 mm Hg (2 times >4 hours apart)
Thrombocytopenia
↑ Creatinine
↑ Transaminases
Pulmonary edema
Visual or cerebral symptoms
ABO incompatibility
ABO hemolytic disease
Risk factors
Infants with blood types A or B born to a mother with blood type O
Clinical features
Jaundice within 24 hours of birth Anemia ↑ Reticulocyte count Hyperbilirubinemia Positive Coombs test
Management
Serial bilirubin levels, oral hydration & phototherapy for most neonates Exchange transfusion for severe anemia/hyperbilirubinemia
This patient with blood group O, whose husband is blood group AB, will bear a child with either blood group A or B. In these situations of ABO incompatibility, signs of hemolytic disease are typically mild and apparent only in approximately one-third of infants. Affected infants are usually asymptomatic or mildly anemic at birth; within the first 24 hours of life they may develop jaundice (eg, hyperbilirubinemia), which typically responds to phototherapy.
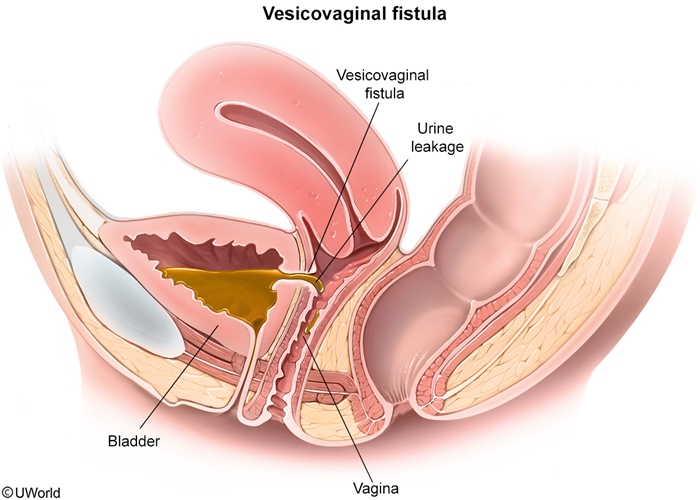
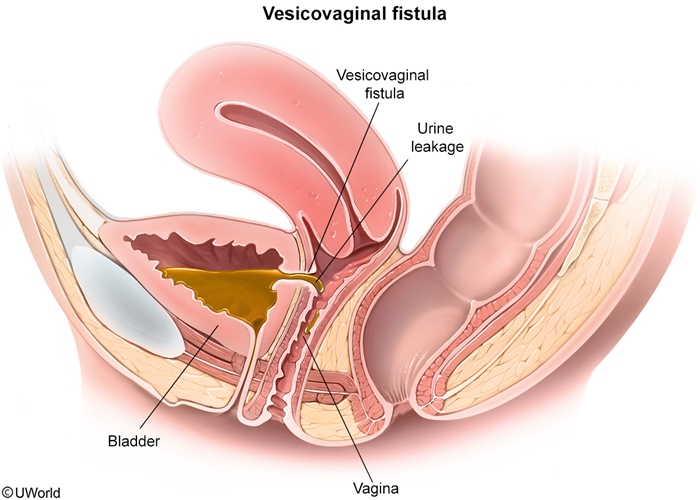
Vesicovaginal fistula
Vesicovaginal fistula
Risk factors
Pelvic surgery Pelvic irradiation Prolonged labor/childbirth trauma Genitourinary malignancy
Clinical features
Painless, continuous urine leakage from the vagina
Diagnostic studies
Physical examination Dye test Cystourethroscopy
This patient's continuous painless urine leakage is most likely due tovesicovaginal fistula after her recent pelvic surgery. In industrialized countries, most urogenital fistulas are due to pelvic surgery or radiotherapy for cancer. Fistulas may result from occult bladder injury during pelvic surgery or from tissue ischemia due to excessive surgical dissection. Urinary incontinence (eg, persistent uncontrolled leakage) into the vagina may present within a month after surgery.
The diagnosis is made clinically by visualization of urine leaking into the vagina. Sometimes a small area of granulation tissue or a hole may be seen. Dye tests and/or cystourethroscopy may be performed to identify a small fistula that is difficult to detect on visual inspection. Cystitis may be a complication, and urinalysis may indicate infection (positive leukocyte esterase/nitrites, bacteriuria, pyuria), as seen in this patient. Bladder catheterization in the immediate postoperative period allows a small fistula to heal. Otherwise, surgical correction is indicated.
Active Labor
Disorders of the active phase of labor
Diagnosis
Clinical features
Treatment
Protraction
Cervical change slower than expected ± Inadequate contractions
Oxytocin
Arrest
No cervical change for >4 hours with adequate contractions OR No cervical change for >6 hours with inadequate contractions
Cesarean delivery
The first stage of labor begins with the onset of regular contractions and ends when the patient is 10 cm dilated. It consists of a latent phase involving gradual cervical dilation and an active phase with rapid dilation. The transition between the latent and active phase typically occurs at 6 cm dilation.
Patients who are >6 cm dilated with slow dilation (labor protraction) or absence of further dilation (labor arrest) have an active phase abnormality. The etiology of active-phase labor abnormalities can be uterine (eg, inadequate contractions), fetal (eg, malpresentation, nonocciput anterior position, macrosomia), or pelvic (deformity or fracture). Arrest of active labor occurs when there is no cervical change for >4 hours with adequate contractions or no cervical change for >6 hours with inadequate contractions.
With an intrauterine pressure catheter in place, the peak contraction pressure minus the baseline intrauterine pressure (both in mm Hg) determines the number of Montevideo units (MVUs) for the contraction. Contractions generating >200 MVUsin a 10-minute interval are considered adequate. This patient has arrest of active labor as she has had no cervical change in 4 hours despite adequate contractions. Cesarean delivery is therefore indicated.
Amnioinfusion
Amnioinfusion involves the instillation of fluid into the uterine cavity to treat variable decelerations. This patient's fetal heart rate tracing has no variable decelerations.
Amnionic fluid embolism
Amniotic fluid embolism
Risk factors
Advanced maternal age Gravida >5 (live births or stillbirths) Cesarean or instrumental delivery Placenta previa or abruption Preeclampsia
Clinical presentation
Cardiogenic shock Hypoxemic respiratory failure Disseminated intravascular coagulopathy Coma or seizures
Treatment
Respiratory & hemodynamic support ± Transfusion
This patient's presentation is concerning for respiratory failure from amniotic fluid embolism syndrome (AFES), a rare but catastrophic complication during pregnancy or shortly after delivery. This patient's risk factors include advanced maternal age and high gravida (>5 live births or stillbirths). Amniotic fluid can enter the maternal circulation through endocervical veins, placental insertion site, or areas of uterine trauma (eg, cesarean incision site). This leads to an inflammatory response causing vasospasm, cardiogenic shock, hypoxemic respiratory failure, and coagulopathy with disseminated intravascular coagulopathy (DIC). Hypoxia can lead to seizures and loss of consciousness, as in this patient.
AFES is diagnosed clinically after excluding other causes of sudden postpartum cardiorespiratory failure (eg, eclampsia, peripartum cardiomyopathy, pulmonary embolism). Treatment is mainly supportive to correct the hypoxemia (eg, oxygen, intubation, mechanical ventilation) and hypotension (eg, vasopressors).
Early recognition with respiratory and hemodynamic support can reduce maternal and fetal mortality, but survivors have a high incidence of neurological damage. This patient did not improve with facemask ventilation and requires intubation with mechanical ventilation as the next step in improving the hypoxemia.
Pseudocyesis
This patient presents with amenorrhea, breast fullness, morning sickness, and abdominal distension - symptoms of early pregnancy - and believes she is pregnant. However, her office examination (thin endometrial stripe, negative urine pregnancy test) excludes pregnancy. This presentation is consistent with pseudocyesis; risk factors include a history of infertility and prior pregnancy loss.
Pseudocyesis likely occurs when the somatization of stress affects the hypothalamic-pituitary-ovarian axis and causes early pregnancy symptoms, or when bodily changes (eg, weight gain, amenorrhea) are misinterpreted. The end result is a nonpsychotic patient who believes she is pregnant. This belief is often strong enough that the patient misinterprets negative home pregnancy tests as being positive. Because pseudocyesis is a form of somatization, management requires psychiatric evaluation and treatment.
Fetal Anemia
Fetal anemia typically presents with a sinusoidal fetal heart tracing, a smooth, undulating waveform with no variability. This patient's tracing has moderate variability.
Chorioamnionitis
Intra-amniotic infection (chorioamnionitis)
Risk factors
Prolonged rupture of membranes (>18 hours) Prolonged labor Internal fetal/uterine monitoring devices Repetitive vaginal examinations Presence of genital tract pathogens
Diagnosis
Maternal fever PLUS >1 of the following: Fetal tachycardia (>160/min) Maternal leukocytosis Purulent amniotic fluid Maternal tachycardia (>100/min) Uterine fundal tenderness
This patient has a fetal heart tracing with moderate variability and fetal tachycardia, a sustained fetal baseline heart rate >160/min. Common causes of fetal tachycardia include maternal infection, poorly controlled maternal hyperthyroidism, medication use (eg, terbutaline), and abruptio placentae. This patient has an intra-amniotic infection (chorioamnionitis) of the uterine decidua, placenta, amniotic fluid, membranes, and umbilical cord that results from migration of vaginal or enteric flora through the cervix into the uterine cavity.
In the setting of protracted labor (slow labor progression) and prolonged membrane rupture (>18 hours), maternal fever suggests intra-amniotic infection as the etiology of the fetal tachycardia. Additional clinical features of intra-amniotic infection include maternal leukocytosis, purulent amniotic fluid, maternal tachycardia, and uterine fundal tenderness. Broad-spectrum antibiotics are administered to reduce the risk of neonatal (eg, sepsis, encephalopathy) and maternal (eg, postpartum hemorrhage, endometritis) morbidity.
Management: abx and induced labor
Tamoxifen
increased endometrial cancer and polyps
decreased risk of ovarian cancer
no change on fibroids
increased risk for DVT
hot flash most common SE
HPL
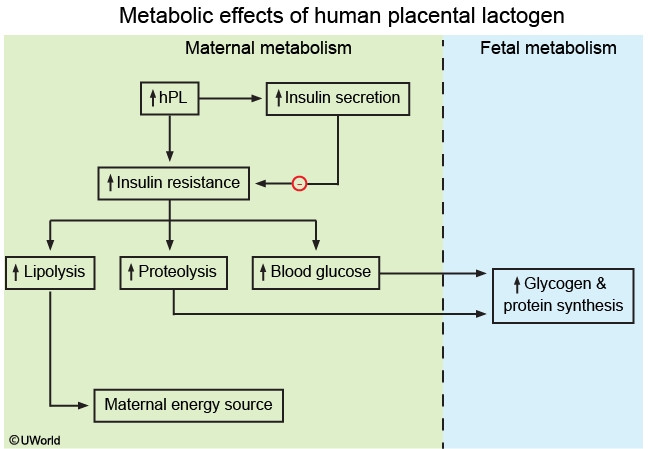
Physiologic adaptations of pregnancy include pancreatic β cell hyperplasia, increased insulin secretion, and increased peripheral insulin resistance. The majority of hormones needed for fetal growth and nutrition in the third trimester are regulated and produced by the placenta. Human placental lactogen (hPL), a placental somatomammotropin, has increased production in the third trimester resulting in pancreatic β cell hyperplasia and increased insulin resistance.
Gestational diabetes mellitus (GDM) occurs when peripheral insulin resistance exceeds pancreatic insulin secretion, resulting in pathologic maternal hyperglycemia.
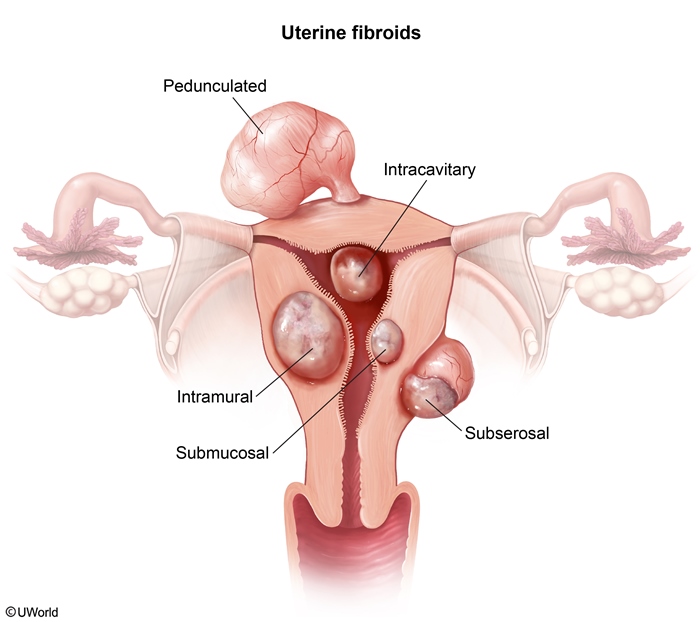
Fibroids vs Endometriosis
Fibroids are abnormal proliferations of the uterine myometrium that can cause urinary and bowel symptoms by putting pressure on these structures. Examination shows an irregularly enlarged uterus, not nodularity in the posterior cul-de-sac.
The classic triad of endometriosis includes dysmenorrhea, dyspareunia, and infertility. The pain in endometriosis occurs 1-2 weeks prior to menses and peaks just before menstruation. Endometriosis is unlikely in this patient with pain during menses and no dyspareunia.
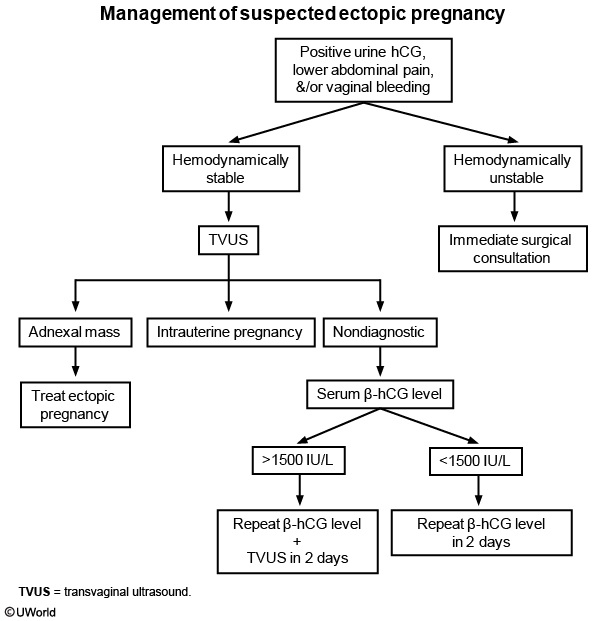
Ectopic
Pregnancy Physiology
Lupus vs Preeclampsia
However, lupus nephritis presents with the associated signs and symptoms of SLE (eg, joint pain, malar rash) and the presence of red blood cell casts on urinalysis. Lupus nephritis can be further distinguished from preeclampsia by decreased complement levels and increasing antinuclear antibody titers.
Uterine Rupture
Uterine rupture typically occurs in patients with prior uterine surgery. This patient has a uterine rupture at the scar of her prior cesarean delivery. Uterine rupture often presents with focal, intense abdominal pain prior to rupture that is relieved by the rupture but resumes shortly after in a diffuse distribution. Hyperventilation, agitation, and tachycardia are signs of imminent rupture, and bleeding may be vaginal and/or intra-abdominal. As in this patient, the presenting fetal part may retract (loss of fetal station), which is pathognomonic of rupture. Fetal limbs may be palpable on abdominal examination and fetal heart tracings are usually abnormal (eg, fetal tachycardia, recurrent decelerations).
To prevent maternal and/or fetal exsanguination, suspected uterine rupture necessitates emergency laparotomy to confirm diagnosis and expedite delivery.
Adenomyosis
Adenomyosis: heavy menstrual bleeding, painful menses (dysmonorrhea)
Fibroids: heavy bleeding, nonpainful menses
Endometriosis: non heavy bleed, painful menses
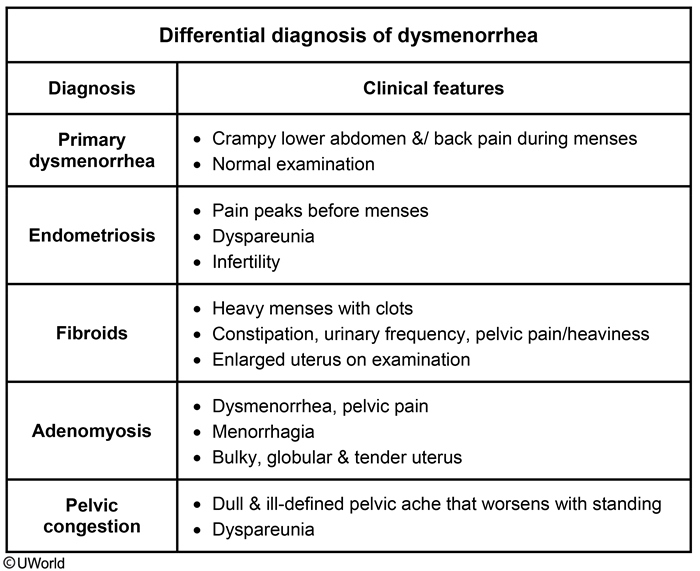
Primary Dysmenorrhea
In women with a normal examination, the presence of painful menses in the absence of dyspareunia or gastrointestinal symptoms is most consistent with primary dysmenorrhea. This patient did not experience pain with oral hormonal contraception and the onset coincides with discontinuing contraception.
Despite the lack of apparent physical findings, primary dysmenorrhea can be debilitating. The treatment objective is pain relief to minimize disruption in the patient's life. First-line treatment consists of nonsteroidal anti-inflammatory medication and/or hormonal contraception. Most women respond well to these oral medications within 3 months.
Anovulation
The most likely diagnosis for this patient is anovulation secondary to morbid obesity. In anovulation, the FSH and LH levels are normal. The ovaries are still producing estrogen, but progesterone is not being produced at the normal post ovulation levels. Therefore, progesterone withdrawal menses at the end of the cycle does not occur.
Hypothyroidism Amenorrhea
Hypothyroidism can present with menstrual dysfunction, fatigue, and hair changes, without signs of hypoestrogenism. Findings include an enlarged thyroid, elevated TSH, and low T3/T4 levels. In hypothyroidism, low T3/T4 increases thyrotropin-releasing hormone (TRH) secretion from the hypothalamus. Increased TRH stimulates prolactin secretion, which has inhibitory effects on GnRH production, thereby decreasing FSH and LH levels.
Premenopausal Uterine Bleed
An endometrial biopsy is indicated in all premenopausal patients age >45 with AUB. In contrast, an endometrial biopsy is performed in patients age <45 who have AUB and are at risk for endometrial hyperplasia and cancer from unopposed estrogen exposure due to obesity and/or chronic anovulation (eg, polycystic ovarian syndrome).
Mastitis
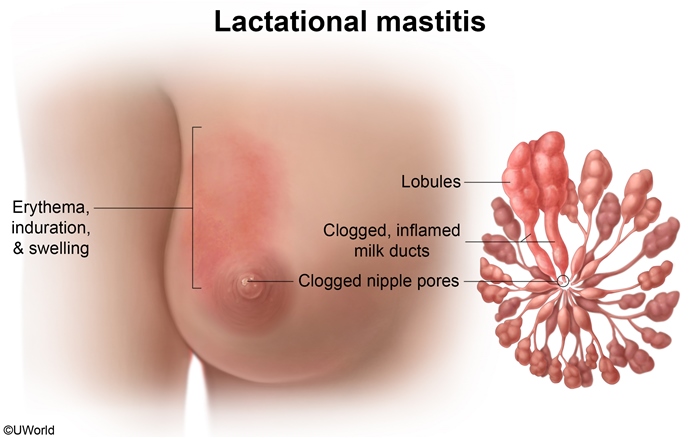
Abscess
Findings suggestive of an abscess include signs of mastitis - localized erythema/pain, fever, and malaise - along with a fluctuant, tender, palpable mass. The diagnosis is made clinically, and an ultrasound may be required to differentiate severe mastitis from an abscess if a mass is deep within the tissue.
Needle aspiration of a breast abscess, usually under ultrasound guidance, and antibiotics (eg, dicloxacillin, cephalexin) for the surrounding mastitis are first-line treatments. Continued breastfeeding is recommended for continued milk drainage.
Incision and drainage (eg, surgical drainage) with packing are recommended for abscesses not responsive to needle aspiration and antibiotics, suspected necrotic material, and large (>5 cm) pus collections. Surgical drainage may be required if the overlying skin is thin with imminent abscess rupture but is not indicated in this patient.
Galactorrhea
This patient's presentation (bilateral, gray, nonbloody nipple discharge) is consistent with physiologic galactorrhea. Galactorrhea is defined as lactation in men or non-breastfeeding women; it may be a sign of a potentially significant disorder and should be evaluated.
Physiologic galactorrhea is usually bilateral and guaiac negative (as in this patient); the appearance is typically milky or clear but can also be yellow, brown, gray, or green. This patient has bilateral, guaiac-negative discharge without signs of malignancy (eg, breast mass, lymphadenopathy, nipple changes, unilateral discharge). Initial evaluation should focus on identifying the etiology and includes serum prolactin, TSH, and a pregnancy test.
Hep C
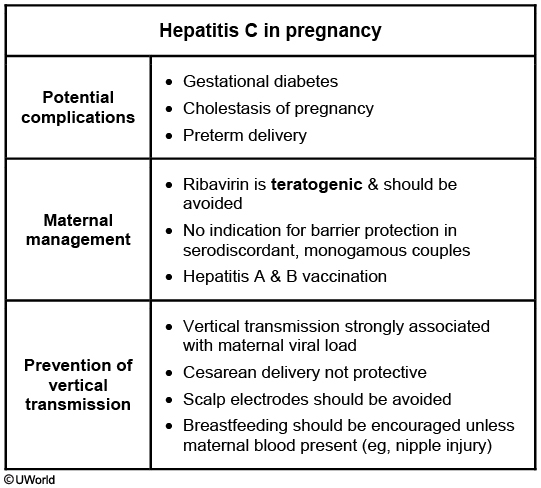
Up to 80% of patients infected with the hepatitis C virus (HCV) develop chronic hepatitis, making hepatitis C the most common cause of chronic hepatitis. HCV infection is acquired most commonly by exposure to infected blood. Pregnant women with chronic hepatitis C are generally asymptomatic during pregnancy, although they are at increased risk for gestational diabetes, cholestasis, and preterm delivery. Patients with chronic HCV infection are also at risk for cirrhosis. Acute viral hepatitis can be life threatening, especially in a patient with pre-existing chronic viral hepatitis. Therefore, all patients with chronic HCV should be immunized against hepatitis A and B if they are not already immune. The inactivated (killed) hepatitis A and B vaccines are both safe to administer during pregnancy.
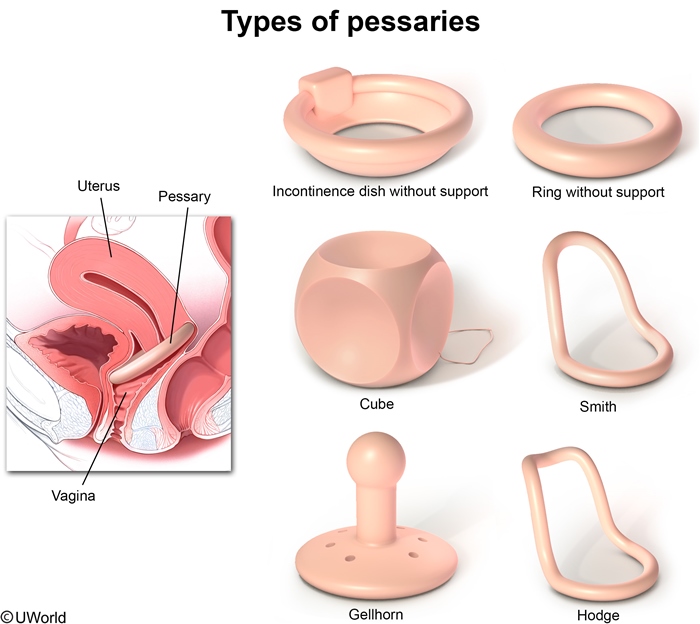
Pessary Fitting
Lichen sclerosis vs atrophic vaginitis
lichen sclerosis: no vaginal involvement
atrophic vaginitis: vaginal dryness and thinning
Hyperemesis
Nausea and vomiting are common during the first trimester of pregnancy. HG can be differentiated from typical nausea and vomiting of pregnancy by the presence of ketones on urinalysis, laboratory abnormalities and changes in volume status. Ketonuria, which occurs due to prolonged hypoglycemia and resultant ketoacidosis, suggests more severe disease. Serum chemistries can evaluate for a hypochloremic metabolic alkalosis, hypokalemia, and elevated serum aminotransferases, all of which can result from persistent vomiting. Severe HG (eg, dehydration, ketonuria, laboratory abnormalities) is an indication for hospital admission for intravenous antiemetics, rehydration, and electrolyte repletion.
Rheumatic Heart Disease
This patient's clinical presentation - cough, progressive dyspnea, and orthopnea - is consistent with pulmonary edema with rapid decompensation due to development of new atrial fibrillation (AF) with rapid ventricular response (RVR). Her history of recurrent sore throat and origin from a country with high incidence of rheumatic heart disease make rheumatic mitral stenosis the most likely diagnosis.
Rheumatic mitral stenosis is an insidious progressive disease, and patients can remain asymptomatic for several years. During pregnancy, physiologic increases in heart rate and blood volume raise the transmitral gradient and left atrial pressure (at rest and during exercise). As seen in this patient, these changes often precipitate symptoms of fatigue, exercise intolerance, or dyspnea in previously asymptomatic patients with rheumatic mitral stenosis. These patients are also at increased risk of developing AF. The loss of an effective "atrial kick" and decrease in diastolic filling times seen with AF and RVR (ie, pulse >100/min) further increases left atrial pressure, with dramatic worsening of pulmonary congestion and pulmonary edema.
Perpartum Cardiomyopathy
Peripartum cardiomyopathy (PPCM) causes rapid-onset systolic heart failure (fatigue, dyspnea, cough, pedal edema) at >36 weeks gestation or the early puerperium. This patient's medical and social history and symptom onset before 36 weeks gestation makes mitral stenosis more likely than PPCM. Also, AF with RVR is relatively rare in PPCM.
Genital Warts
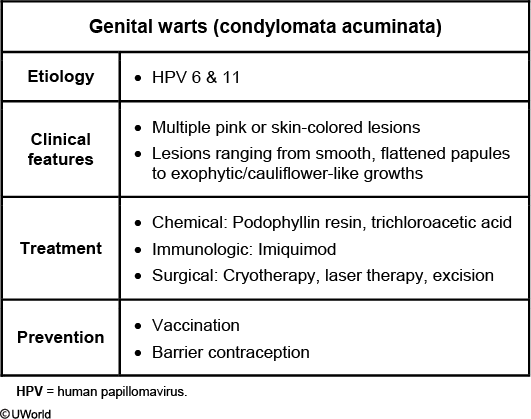
Genital warts (condylomata acuminata) are caused by the human papillomavirus (HPV), the most common sexually transmitted infection in the United States. HPV strains 6 and 11 are most likely to cause the warts, whereas high-risk strains 16 and 18 are associated with high-grade cervical intraepithelial neoplasia and cervical cancer. Internal and/or external vaginal lesions as well as anogenital lesions occur in women. Genital warts appear as clusters of soft, pink or skin-colored lesions. Most lesions are exophytic and cauliflower-like, although some may appear sessile and flat. Genital warts are most often asymptomatic, although pruritus and bleeding from a lesion are possible.
Diagnosis can be made based solely on the characteristic appearance of the lesions. Small lesions may be treated with applications of trichloroacetic acid or podophyllin resin. Excisional therapy may be considered for larger lesions. Recurrence rates are high, regardless of treatment modality.
Condylomata lata, caused by secondary syphilis, are flat, velvety lesions. In contrast to condylomata acuminata, condylomata lata have a broader base and flatter surface and are lobulated or plaque-like.
PPROM
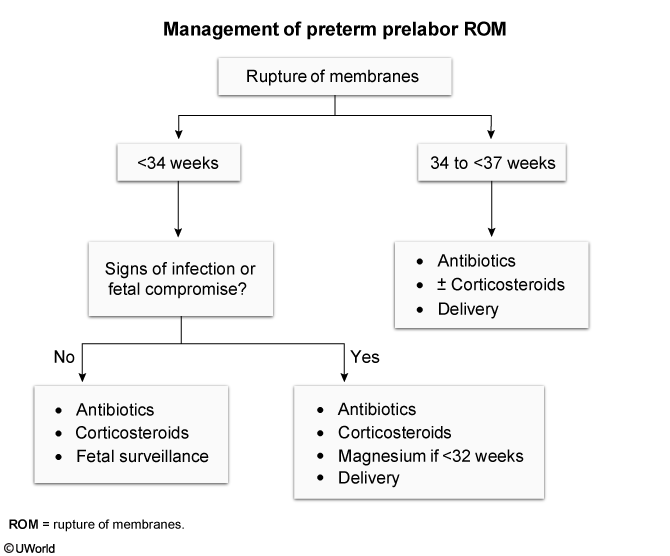
Preterm premature rupture of membranes (PPROM) refers to rupture of membranes at <37 weeks gestation prior to the onset of labor. Some patients with membrane rupture have a gush of vaginal fluid. Others experience intermittent leakage (as with this patient) or vaginal wetness, symptoms also seen with urinary incontinence. Although this patient has experienced stress urinary incontinence for the past 6 weeks, her increased leakage frequency, nitrazine-positive vaginal fluid, and decreased amniotic fluid index are consistent with PPROM.
Patients with PPROM at >34 weeks gestation should be delivered as the morbidity and mortality associated with premature delivery decrease after 34 weeks and delivery decreases the incidence of chorioamnionitis. Patients with PPROM at <34 weeks with signs of infection (eg, maternal fever, fetal tachycardia) or fetal compromise should also be delivered. To prevent neonatal group B Streptococcus(GBS) infection, intrapartum intravenous penicillin should be administered to patients with PPROM who are delivered and have either an unknown or positive GBS status. Tocolytics are contraindicated.
This patient has PPROM at 35 weeks gestation and her GBS status is unknown. She should be delivered and receive intrapartum penicillin.
Mastitis
Dicloxacillin
Endometritis
polymicrobial, clinda+gent
Postpartum Urinary Retention
Postpartum urinary retention
Risk factors
Primiparity Regional anesthesia Operative vaginal delivery Perineal injury Cesarean delivery
Clinicalfeatures
Inability to void or small-volume voids Incomplete bladder emptying Dribbling of urine
Management
Self-limited condition Intermittent catheterization
The patient has acute postpartum urinary retention and overflow incontinence due to multiple risk factors (eg, nulliparity, prolonged labor, instrumental delivery, regional anesthesia, perineal trauma). Regional anesthesia reduces sensory and motor impulses of the sacral spinal cord, which suppresses the micturition reflex and decreases detrusor tone (eg, bladder atony). Urinary retention can also result from pudendal nerve palsy from pelvic floor injury and perineal edema from tissue trauma.
The diagnosis should be suspected when the patient is unable to void by 6 hours after vaginal delivery or 6 hours after removal of an indwelling catheter after cesarean delivery. Other symptoms include urinary dribbling and lower abdominal or suprapubic pain/pressure. On examination, an over-distended bladder may be palpable in thin patients but difficult to detect in obese patients. Urethral catheterization is more accurate than bladder ultrasound and confirms retention when it produces >150 mL of urine.
If conservative measures (eg, analgesia, ambulation) do not result in voiding, urethral catheterization should be performed. Patients should be reassured that the retention is usually temporary and reversible.
Breast Cancer Contraceptive
Copper IUD. Combined and progesterone both CI
BPP
fetal hypoxia
Oxytocin Toxicity
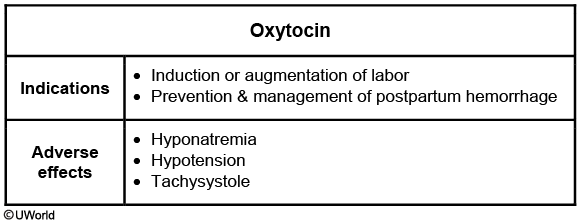
All agents used for labor induction, including oxytocin, can cause uterine tachysystole, which refers to abnormally frequent contractions (>5 contractions in 10 minutes averaged over a 30-minute period). Induction drugs also increase the risk of tetanic (intense or prolonged) contractions, particularly at higher doses, such as in this patient. Although many fetuses tolerate tachysystole with no adverse outcome, fetal heart rate tracing abnormalities are more common with tachysystole due to insufficient uterine relaxation between contractions, causing placental spiral artery constriction, a decrease in placental blood flow, and fetal hypoxia. Consequently, tachysystole is associated with an increased risk for cesarean delivery, low umbilical cord pH, and neonatal intensive care unit admission.
5a Reductase
5-alpha-reductase deficiency
Pathogenesis
46,XY genotype Impaired testosterone to DHT conversion Impaired virilization during embryogenesis Normal male testosterone & estrogen levels
Clinical features
Male internal genitalia (eg, testes, vas deferens) Female external genitalia (eg, blind-ending vagina) Phenotypically female at birth Virilization at puberty (↑ testosterone) Clitoromegaly Increased muscle mass Male-pattern hair development Nodulocystic acne
DHT = dihydrotestosterone.
During embryogenesis, sexual development in genotypically male fetuses (46,XY) occurs due to testicular hormone production. The testes produce testosterone, which promotes development of the male internal genitalia (eg, vas deferens, epididymis). Testosterone is also converted to dihydrotestosterone (DHT) via 5-alpha-reductase; DHT promotes development of the male external genitalia (eg, penis) and prostate. Patients with 5-alpha-reductase deficiency are unable to convert testosterone into DHT; therefore, they have no male external genitalia development, have undescended testes (eg, bilateral labial masses), and appear phenotypically female at birth.
At puberty, increased testosterone levels cause virilization, such as nodulocystic acne and clitoromegaly (ie, clitoris protruding from the clitoral hood), of phenotypically female patients. Additional features of virilization may include voice deepening and increased muscle mass. The testosterone levels at puberty are at the normal male range; therefore, patients develop additional normal secondary sexual characteristics (eg, axillary and pubic hair). Patients have no breast development because testosterone binds to the breast androgen receptor and inhibits breast tissue proliferation. Diagnosis in adolescents and adults is based on an elevated testosterone/DHT ratio. Management is dependent on age and gender identity.
Patients with androgen insensitivity syndrome (AIS) have a defective androgen receptor, which prevents virilization during embryogenesis. Fetuses have male internal genitalia (ie, testes) that produce testosterone but, due to peripheral testosterone resistance, do not develop male external genitalia. Therefore, patients with AIS appear phenotypically female at birth. However, in contrast to patients with 5-alpha-reductase deficiency, those with AIS have breast development at puberty as the defective androgen receptor is unable to inhibit breast tissue proliferation.
Exercises
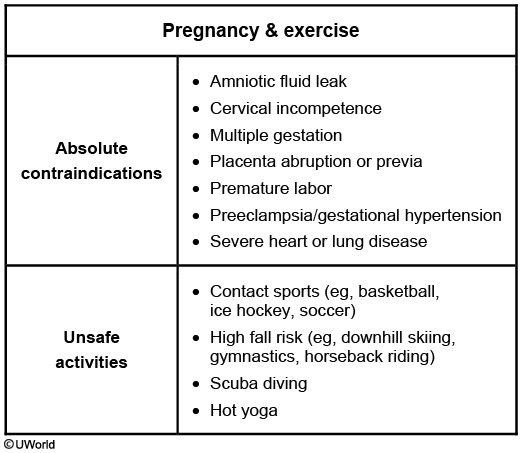
20-30 min
Mullerian Agenesis
Because of their common embryologic source and synchronous development in the first trimester, internal genital anomalies are often concurrent with renal abnormalities. Therefore, women with müllerian agenesis should undergo evaluation of the renal tract (ie, ureters, kidney) with a renal ultrasound. Common abnormalities include unilateral renal agenesis, pelvic kidneys, and duplications of the collecting system.
Last updated