Pretest Cardiorespiratory
Cardiovascular
TCA Toxicity
Close monitoring in the ICU and tricyclic antidepressant Fab antibody fragments (if available) are administered.
Rheumatic Fever
The major criteria are:
carditis, arthritis, erythema marginatum, chorea, and subcutaneous nodules. (Jones)
The minor criteria are:
arthralgia (most common) (joint pain with no objective findings), fever or history of rheumatic fever, increased erythrocyte sedimentation rate (ESR), positive C-reactive protein, increased WBC and anemia, and prolonged PR and QT intervals on ECG.
To make the diagnosis of rheumatic fever, the following criteria should be met: two major manifestations, one major and two minor manifestations plus strong evidence of a preceding group A β-hemolytic streptococcal infection (culture, rapid antigen-antibody rise, or elevation), or scarlet fever.

erythema marginatum
Tetralogy
Morphine sulfate, propranolol. O2, fluid
Prolonged hypoxia can lead to acidosis; correction may require infusion of sodium bicarbonate.
Hereditary Angioedema
autosomal dominant trait
symptoms: In addition to otherwise asymptomatic subcutaneous edema, edema can occur in the gastrointestinal tract and produce the symptoms accompanied by abdominal pain, vomiting, and diarrhea. Laryngeal edema with airway obstruction can also occur
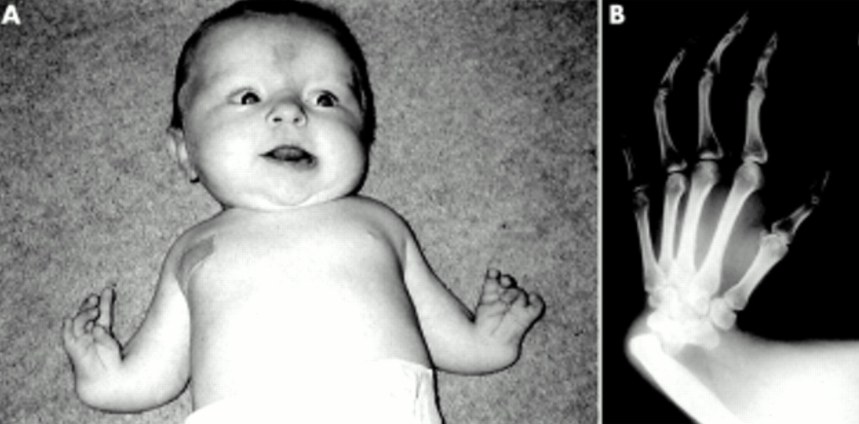
Ellis-van Creveld syndrome
path: genetics
inheritance: AR
pt: increased incidence among persons of Old Order Amish descent
symptoms: Disproportionate dwarfism, postaxial polydactyly, ectodermal dysplasia, a small chest, and a high frequency of congenital heart defects
association: (defect 4p16) is associated with ASD.,


CHD incidence
The incidence of congenital heart disease in the population is about 1%.
Overall, the rate averages from about 2% to 6% if the heart disease is not associated with a diagnosable syndrome.
If two children with congenital heart disease are diagnosed, the risk escalates to 20% to 30%.
Tricuspid Regurge
A history of birth asphyxia or findings of other cardiac lesions often is present.,
Kawasaki
Many conditions can be associated with prolonged fever (Kawasaki > 5 days), a limp caused by arthralgia, exanthem, adenopathy, and pharyngitis.
Conjunctivitis, however, is suggestive of Kawasaki disease. The fissured lips, although common in Kawasaki disease, could occur after a long period of fever from any cause if the child became dehydrated. The predominance of neutrophils and high ESR are common to all. An increase in platelets within this constellation of symptoms, however, is found typically in Kawasaki disease. Kawasaki disease presents as a picture of prolonged fever, rash, epidermal peeling on the hands and feet (especially around the fingertips), conjunctivitis, lymphadenopathy, fissured lips, oropharyngeal mucosal erythema, and arthralgia or arthritis.
WPW
increased HR > CHF
A pulse rate greater than 250 beats per minute, however, should suggest the presence of a tachyarrhythmia.
Common causes for supraventricular tachycardia include Wolff-ParkinsonWhite (WPW) syndrome, congenital heart disease, and sympathomimetic drugs.
Verapamil
Verapamil is contraindicated in this age group, as it may cause acute hypotension and cardiac arrest.
Cardio treatment
Synchronized DC cardioversion may be performed in patients in shock or with heart failure; it must, however, be synchronized to the QRS complex. Transthoracic pacing is typically useful in bradyarrhythmias. A precordial thump might help individuals with an acute arrest from ventricular fibrillation, but does not resolve SVT.
Ebstein
Path: atrialization of RA, cyanosis and HF from severe tricuspid regurge
symptoms: minimal cyanosis has an S3 and S4 (a quadruple rhythm), a systolic murmur in the pulmonic area, and a middiastolic murmur along the lower left sternal border. An ECG shows right atrial hypertrophy and a ventricular block pattern in the right chest leads.,
WPW
Active play and exposure to over-the-counter medications containing sympathomimetics in a healthy 4-year-old child can cause symptoms such as those described in the question in children with WPW syndrome by precipitating paroxysmal supraventricular tachycardia.
Ventricular Impulse
Patients with tricuspid atresia typically have a hypoplastic right ventricle, and therefore the ECG shows left-axis deviation and left ventricular hypertrophy; this translates to a left ventricular impulse on physical examination. Almost all other forms of cyanotic congenital heart disease are associated with elevated pressures in the right ventricle and increased right ventricular impulse. In those conditions, therefore, the ECG will show right-axis deviation and right ventricular hypertrophy
Cyanosis
Transposition of the great vessels with an intact ventricular septum presents with early cyanosis, a normal-sized heart (classic “egg on a string” radiographic pattern in one-third of cases), normal or slightly increased pulmonary vascular markings, and an ECG showing right-axis deviation and right ventricular hypertrophy.
In tetralogy of Fallot, cyanosis is often not seen in the first few days of life.
Tricuspid atresia, a cause of early cyanosis, causes diminished pulmonary arterial blood flow; the pulmonary fields on x-ray demonstrate a diminution of pulmonary vascularity, and left-axis and left ventricular hypertrophy are shown by ECG.
Total anomalous pulmonary venous return below the diaphragm is associated with obstruction to pulmonary venous return and a classic radiographic finding of marked, fluffy-appearing venous congestion (“snowman”).
In pulmonic atresia with an intact ventricular septum, cyanosis appears early, the lung markings are normal to diminished, and the heart is large.
MVP
inherited in an autosomal dominant fashion
demographics: manifests only during adolescence or later. It is more common in girls
diagnosis
confirmed with an echocardiogram that shows prolapse of the mitral leaflets during mid to late systole.
The ECG and chest x-ray are usually normal
treatment
β-Blockers and digitalis are unlikely to be required
penicillin prophylaxis for dental procedures for patients with mitral valve prolapse is no longer recommended
Thrombocytopenia Absent Radius Syndrome
diagnosed in the newborn who demonstrates profound thrombocytopenia, bilateral absence of radius, and abnormally shaped thumbs. (Shortened lower distal arms but with thumbs)
association: Cardiac lesions include TOF and ASD.
prognosis: About 40% of patients die in the newborn period as a result of low-plateletinduced bleeding.,
Noonan
symptoms: The most common features include short stature, downslanting palpebral fissures, ptosis, low set and malformed ears, webbed neck, shieldlike chest, pulmonic stenosis, edema of the dorsum of the hands and feet, hearing loss, pectus excavatum, bleeding diathesis, and cryptorchidism. Mental retardation is seen in oneforth of affected individuals. It is associated with advanced paternal age.,
HCM
A midsystolic ejection murmur and a left ventricular lift sometimes can be appreciated on physical examination.,
Neonatal Lupus
path: transferred maternal IgG autoantibodies
symptoms: Infants can have thrombocytopenia, neutropenia, rash, liver dysfunction (petechiae), and a congenital heart block.
Most manifestations are self resolved; however, the congenital heart block is permanent and frequently requires pacing.,
Respiratory
Phrenic
cause: Infants born to mothers with gestational diabetes are at risk for being LGA and thus at increased risk for peripheral nerve injuries such as Erb-Duchenne and phrenic nerve paralysis.
symptoms: you find that the infant is cyanotic, has irregular, labored breathing, and has decreased breath sounds on the right side. You also note decreased tone in the right arm. You provide oxygen and order a stat portable chest radiograph, which is normal.
An ultrasound or fluoroscopy of the chest would reveal asymmetric diaphragmatic motion in a seesaw manner
Amiloride for CF
amiloride by inhibiting sodium, and with it water reabsorption, thereby improving airway hydration
Hydrocarbon aspiration
cause:
Hydrocarbons with low viscosity and high volatility are the most likely agents to cause respiratory symptoms. Gasoline, kerosene, and furniture polish (which contain hydrocarbons) are common agents responsible for hydrocarbon aspiration.
symptoms: Hydrocarbon aspiration can produce dyspnea, cyanosis, and respiratory failure.
Treatment: symptomatic, sometimes requiring intubation and mechanical ventilation.
Induction of emesis is contraindicated, as this may cause further aspiration. Placement of a nasogastric tube is used only in high-volume ingestions or when the hydrocarbon is mixed with another toxin. Charcoal is not useful, and no intravenous binding agent is available.
TB
diagnosis
Three to eight weeks is required after exposure before hypersensitivity to tuberculin develops. This means that the tuberculin test must be repeated in exposed persons if there is a negative reaction at the time that contact with the source of infection is broken. TB skin tests are usually negative in infants of this age, even when active disease is ongoing.
Sputum, when produced in child of this age, is promptly swallowed, and for this reason specimens for microbial confirmation can be obtained by means of gastric lavage from smaller children.
Small children with primary pulmonary tuberculosis are not considered infectious to others, and they are not capable of coughing up and producing sputum.
IPH
demographics: found primarily in children
recurrent episodes of pneumonia and hemoptysis (diffuse alveolar hemorrhage). Recurrent alveolar bleeding may eventually produce pulmonary hemosiderosis and fibrosis. Diffuse alveolar hemorrhage is characterized by hemoptysis, dyspnea, alveolar opacities on chest radiographs, and anemia.
diagnosis:
can see clubbing: chronic process
bronchoalveolar lavage: see hemosiderin macrophages
Heiner syndrome: A distinct subset of patients with pulmonary hemosiderosis have hypersensitivity to cow’s milk (the association is called Heiner syndrome) and may improve with a diet free of cow’s milk products.,
Nasal foreign body
Small children frequently introduce any number of small objects into their noses, ranging from food to small toys. Initially, only local irritation occurs. Later, as prolonged obstruction is seen, symptoms increase to include worsening of pain, and a purulent, malodorous, bloody discharge can be seen. Unilateral nasal discharge in the presence of obstruction suggests the need to examine the patient for a nasal foreign body.
Tension Pneumo
Tension pneumothorax, a recognized complication of staphylococcal (and other) pneumonia is caused by toxin production by the bacteria leading to rupture of the alveoli into the pleural space. Tension pneumothorax can be quickly lethal if not recognized and treated; this makes a high index of suspicion and prompt diagnosis mandatory.
T Canis
Blindness. Tendency to eat dirt.,
Diagnosis with Elisa
Foreign body in esophagus
Initially, the foreign ody may cause a cough, drooling, and choking. Later, pain, avoidance of food (liquids are tolerated better), and shortness of breath can develop.
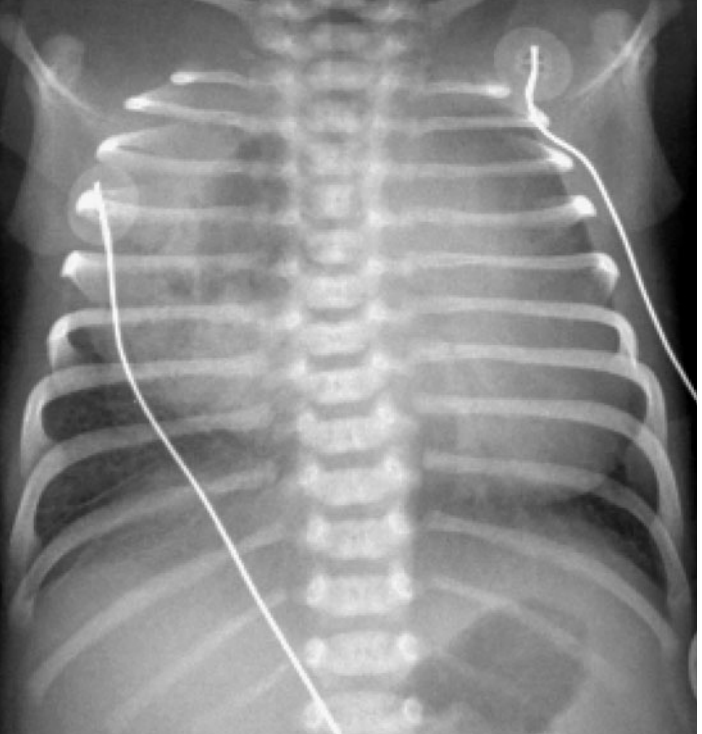
Congenital cystic adenomatoid malformation (CCAM)
path: thought to arise from an embryonic disruption before the thirty-fifth day that causes improper development of bronchioles.
symptoms: The infant has diminished breath sounds on the left, and the PMI is shifted toward the right.
diagnosis:
The cystic mass is usually identified on prenatal ultrasound around the 20th week.
Large lesions (as that noted on the radiograph on the right side) may compress the affected lung and cause pulmonary hypoplasia, which may cause midline shift away from the lesion (note the heart is shifted toward the left on the radiograph).
treatment: Treatment is typically surgical excision of the affected lobe. Some patients may be at risk for primary pulmonary malignancy.,
Asthma
Category
Symptoms
Treatment
Mild intermittent
< 2x/wk, <2 night/mo
PRN SABA
Mild persistent
> 2x/wk, 3-4 night/mo
ICS, SABA, others
Moderate persistent
> 1 night/mo
ICS, ICS with LABA, theophylline
Severe persistent
Ongoing, frequent night
ICS, LABA, oral steoids
ABG
The blood gases of row D are impossible in a patient breathing room air. The PCO2 cannot go up without the PO2 dropping roughly proportionately. An increase in PCO2 of 20 mm Hg, from 40 to 60 mm Hg, should therefore produce a fall in PO2 from 90 to 70 mm Hg. The test should be repeated after the blood gas equipment has been checked and recalibrated.
Last updated