Headache
Cluster
Cluster headaches are a type of chronic headache that occurs at the same time each day, which occur for days to weeks. The clusters of painful headache episodes are separated by periods of remission.
Males are more likely to have cluster headaches than females.
The pathogenesis of cluster headache is thought to be due to aberrant activation of trigeminal-hypothalamic pathways.
Occurs at the same time each day, which occur for days to weeks. The clusters of painful headache episodes are separated by periods of remission.
Symptoms of cluster headaches include severe unilateral periorbital pain. The pain is described as a boring or drilling sensation. Cluster headaches are associated with ipsilateral autonomic symptoms (e.g. ptosis, miosis, lacrimation, rhinorrhea).
Cluster headaches are often associated with Horner syndrome (which includes ptosis, miosis, and anhidrosis), lacrimation, and nasal congestion.
They can last from 15 to 180 minutes and classically awaken patients from sleep.
100% oxygen (preferred) or subcutaneous sumatriptan are the first-line abortive treatments for acute cluster headache.
Verapamil is the first-line treatment for patients with chronic cluster headaches.
Alternative agents include prednisone (especially in patients with active cluster periods <2 months), lithium, ergotamine, and topiramate.
Migraines
Symptoms
Migraines are severe, throbbing headaches, often unilateral, that may be accompanied by other symptoms such as nausea, vomiting, photophobia (sensitivity to lights), and phonophobia (sensitivity to noise), flushing, tearing, and rhinorrhea.
Migraines can last anywhere from 4-72 hours.
Migraine with aura (a.k.a. classic migraine) are severe headaches preceded by a visual change such as bright or flashing lights, dark spots occluding areas of vision (scotomas), visual field changes, and even focal neurological deficits such as hemiparesis. Auras typically last for 10-20 minutes.
Migraine without aura (a.k.a. common migraine) are severe headaches that are not preceded by an aura. Most cases of migraines do not involve an aura.
Migraines in children are often bifrontal and shorter in duration.
Basilar migraines occur due to cerebral vasospasm involving the brainstem. Patients typically have basilar aura symptoms (eg, vertigo, dysarthria, tinnitus, diplopia) without motor weakness, followed by a migraine-type headache.
Demographics
People that suffer migraines are often 10-30 years of age; females are more commonly affected than males.
The pathophysiology of migraines is poorly understood, but it is thought to be due to neuronal dysfunction.
Factors that can precipitate migraines include:
Stress
Oral contraceptives
Menstruation
Exertion
Foods containing tyramine or nitrates (chocolate, cheese, processed meats)
Treatment
Migraine treatment consists of:
NSAIDs (chronic NSAID use for treatment/prophylaxis can cause migraine headaches)
Ergotamine, dihydroergotamine
Selective serotonin agonists (e.g.sumatriptan, zolmitriptan)
IV antiemetics (e.g. metoclopramide, chlorpromazine)
Migraine prophylaxis includes the use of:
Tricyclic antidepressant (e.g. amitriptyline)
Beta blockers (e.g. metoprolol, propranolol, timolol)
Calcium channel blockers (e.g. nifedipine, verapamil)
Anticonvulsants (e.g. valproate, topiramate)
Tension
Tension headaches are a diffuse, mild to moderate headache that is often described as feeling like there’s a tight band around the head. It is the most common type of headache.
Tension headaches affect females more often than males.
Factors that precipitate tension headaches include stress and fatigue. (death of family member)
Pain from tension headaches is usually bilateral (unlike migraines and cluster headaches), with a feeling of tightness and occipital or neck pain. It is also associated with anxiety. Unlike migraines and cluster headaches, tension headaches have a variable duration.
Treatment of tension headaches includes:
NSAIDs
Amitriptyline
Ergotamine, dihydroergotamine
Sumatriptan, zolmitriptan
Relaxation exercises
Trigeminal Neuralgia
Trigeminal neuralgia is head and facial pain along the distribution of one or more branches of the trigeminal nerve distribution (most commonly V2 and/or V3).
It is thought to be caused by compression or irritation of the trigeminal nerve root.
Symptoms
The presentation of trigeminal neuralgia includes sudden severe pain in the maxillary and mandibular branches of the trigeminal nerve.
Pain may be induced by stimulating a “trigger zone,” which is an area that when lightly touched stimulates an attack.
Multiple sclerosis (MS), an autoimmune demyelinating central nervous system disorder, is one of the few conditions that may present with trigeminal neuralgia bilaterally. This occurs due to demyelination of the nucleus of the trigeminal nerve or the nerve root, which leads to improper signaling of the nerve and paroxysms of severe pain. This patient's episode of right hand numbness that lasted 2 weeks and spontaneously improved was likely her first symptom of MS.
Herpes zoster is caused by nerve inflammation from viral reactivation, leading to neuritis followed by a dermatomal vesicular rash. When the trigeminal nerve is involved, it is usually the V1 branch (herpes zoster ophthalmicus), which can lead to blindness. In a healthy patient, herpes zoster usually involves one dermatome and is unlikely to present bilaterally.
Diagnosis
In some cases MRI can be used to identify lesions related to nerve compression in those patients presenting with trigeminal neuralgia.
Carbamazepine is the drug of choice for patients with trigeminal neuralgia. Other medications include:
Phenytoin
Gabapentin
Valproic acid
Clonazepam
In some cases, surgical decompression of the nerve proves helpful.
Pseudotumor Cerebri
Idiopathic intracranial hypertension (pseudotumor cerebri) is increased intracranial pressure with no apparent cause on imaging.
Risk factors for idiopathic intracranial hypertension include:
Female of reproductive age
Vitamin A excess (isotretinoin for acne)
Danazol (old synthetic steroid used to suppress gonadotrophins, replaced by GnRH agonists). Glucocorticoids
OCP
Tetracyclines
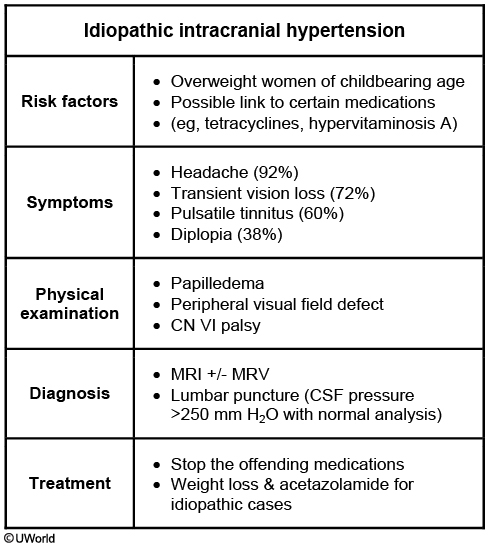
Patients with idiopathic intracranial hypertension will present with:
Headaches
Visual symptoms
Diplopia (CN VI palsy)
Loss of vision (sustained or transient)
Pulsatile tinnitus: whooshing sounds
Papilledema
No alterations in mental status
Empty sella can be present
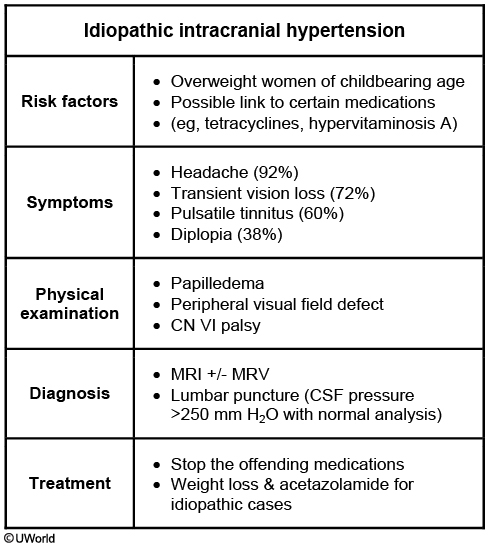
Lumbar puncture in patients with idiopathic intracranial hypertension will reveal elevated opening pressure that relieves the headache.
Treatment options for idiopathic intracranial hypertension include:
Acetazolamide
Topiramate
Weight loss
Invasive procedures (lumbar puncture, shunt placement, optic nerve fenestration)
For patients with symptoms refractory to medical therapy or those with progressive vision loss, surgical intervention with optic nerve sheath decompression or lumboperitoneal shunting is recommended. Short-term use of corticosteroids or serial lumbar puncture (LP) can serve as bridging therapy for patients awaiting definitive surgical treatment. These are not recommended as primary intervention due to side effects associated with long-term corticosteroid use and the complications associated with LPs.
Untreated idiopathic intracranial hypertension can lead to blindness.
Concussion
A concussion is a traumatic brain injury that temporarily disrupts brain function. A concussion is caused by blunt trauma such as a blow to the head.
Symptoms
A loss of consciousness is not required for the diagnosis.
Symptoms of a concussion include dizziness, confusion, trouble concentrating, headache, memory loss, balance or coordination problems.
Be aware of symptoms that suggest increased intracranial pressure such as vomiting, focal neurologic deficits, or delirium.
Diagnosis
Diagnosis and clinical workup of a concussion may involve a CT scan and thorough neurologic evaluation to assess for possible blood or swelling in the brain.
Concussed patients are often kept under observation in the hospital or at home to watch for the development of more serious neurological problems.
Subdural and epidural hematomas must be ruled out.
Management
Typically, these symptoms resolve with symptomatic treatment within a few weeks to months following TBI; however, some patients may have persistent symptoms lasting ≥6 months.
Treatment of a concussion involves mental and physical rest, use acetaminophen for headaches (ibuprofen or aspirin increase risk for bleeding).
Last updated